CHAPTER 22 Thoracic outlet syndrome
Summary box
Introduction
Historically, these varied syndromes were named based on their presumed site of vascular or neurologic compression, either static or dynamic: scalenus anticus syndrome, cervical rib syndrome, etc. (Box 22.1). Each of the different syndromes described in the early 20th century had its own specific, anatomically directed treatment, but none were clearly effective. The unifying theme of these syndromes was their origin in the area bounded by the cervical spine, the first rib, and the scalene muscles – the thoracic outlet. Some authors also include the cervicoaxillary tunnel, which contains both the costoclavicular space and the subcoracoid space. Although some of the symptom complexes may be caused by compression between the clavicle and the first rib (the costoclavicular space) or beneath the pectoralis minor tendon at the coracoid process (subcoracoid space), the vast majority of these symptom complexes appear to be caused by vascular or neural compression in the space bounded by the first rib, the cervical spine, and the scalene muscles – the true thoracic outlet. In 1956, Peet et al.1 brought all these syndromes together under one common diagnosis – thoracic outlet syndrome – indicating the common area of origin of the disparate syndromes, the thoracic outlet.
The syndromes can be divided into 2 types: vascular (arterial and venous) and neurologic.2 The arterial syndrome, caused by compression of the subclavian artery in the thoracic outlet, counts for only about 2% of these diagnoses. In this syndrome, ischemic and embolic phenomena predominate. Patients present with a diffusely painful, easily fatigued arm. The radial pulse is reduced or absent. Distal emboli may cause gangrene of the fingertips. The venous syndrome, called effort thrombosis or Paget-Schroetter syndrome, is quite different from the others and is caused by thrombosis of the subclavian vein, often after heavy exercise. It presents with edema of the arm, venous engorgement, cyanosis, and deep pain and tenderness. It often presents acutely and is more common than the arterial syndrome. Vascular forms of TOS account for approximately 10% of all surgery for this diagnosis, and are well-covered in the vascular and thoracic surgery literature. They will not be further discussed here. The vascular and neurogenic forms rarely coexist in the same patient.
The neurogenic form of TOS accounts for the vast majority of patients. The varied combinations of symptoms and signs and tests and treatments have led to confusion and controversy as to what constitutes neurogenic TOS. Many patients in this group have few objective neurologic findings. The diagnosis is often made largely on history and subjective findings alone. In the past, before electrodiagnostic testing, many patients may have had distal entrapment neuropathies of the ulnar or median nerves or a cervical radiculopathy. These difficulties and controversies are reflected in the vast literature concerning this syndrome.3,4,5,6
Anatomy and physiology
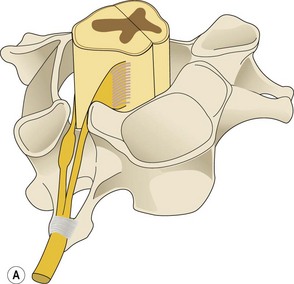
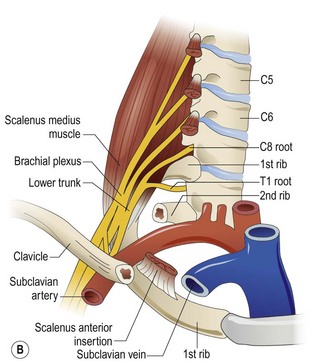
In understanding neurogenic TOS, the most important structure is the scalene, or inter-scalene, triangle formed by the anterior scalene muscle anteriorly and medially, the middle scalene posteriorly and laterally, and the superior border of the first rib inferiorly. Both scalene muscles insert at the first rib, the anterior scalene inserts at the scalene tubercle, and the middle scalene inserts 1 or 2 cm further laterally. The anterior scalene has its origin on the anterior tubercles of the lateral masses of the C3–C6 cervical vertebrae. The middle scalene originates from the posterior tubercles of the C2–C7 vertebrae. The spinal nerves of the brachial plexus exit their neural foramina between the tubercles and thus, descend between the scalenes in a lateral, caudal, slightly anterior direction. As the C5–C8 spinal nerves pass superior to the first rib, the T1 root must take a different course. Exiting the neural foramen between the T1 and T2 vertebrae in the thorax caudal to the first rib, the T1 spinal nerve passes superiorly, crossing the first rib anteriorly, and then turning superiorly around its neck to join the C8 nerve at the superior surface of the rib and form the lower trunk (Figure 22.1). Thus, the origins of the lower trunk embrace the neck of the first rib.
The subclavian artery leaves the thorax and ascends between the scalenes anterior to the lower trunk of the plexus before entering the axilla above the first rib. Although the entire brachial plexus traverses the scalene triangle, only the lower trunk of the plexus and the subclavian artery come into contact with the first rib between the insertions of the scalenes. It is in this area of the inferior scalene triangle that the lower trunk of the plexus and the subclavian artery can be compressed by anatomic anomalies such as an aberrant or fused scalene muscle insertion, cervical ribs, fibrous bands, or an anomalous first rib. Nearly all of the signs and symptoms of the various appearances of the TOS appear to involve the lower trunk of the brachial plexus. Although “upper plexus” TOSs involving the C5–C7 (upper and middle trunks) have been described, a convincing anatomic basis for them is not apparent.7
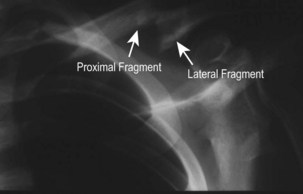
Chronic compression however, can occur in the costoclavicular space in the case of a fractured, displaced clavicle with bone or healing callus compressing the plexus between the fracture and the first rib.8 This is the “traumatic” TOS. Fractures here largely occur in the middle third of the clavicle; the lateral fragment ends up deep and inferior to the proximal one (Figure 22.2). If this malalignment persists and a large callus forms, the plexus, especially the medial cord, will be compressed. Because neurologic deficits arising from medial cord compression closely resemble those of lower trunk compression, the clinical picture does resemble the true TOS. This entity, however, is quickly recognized by injury history and the deformity on x-ray. It can be relieved by improved reduction and fixation of the fracture if found acutely, or by resection of the callus if the diagnosis is delayed.9,10
In addition to the known anatomic anomalies in the thoracic outlet, a number of postural and dynamic factors have also been implicated as leading to brachial plexus stretch or compression. The importance of these factors is unknown. Due to our upright posture, the shoulder girdle descends gradually with aging. This may cause increased traction on the lower trunk of the plexus as it crosses over the first rib. The relatively greater shoulder descent in females and their weaker shoulder suspensory muscles may account for the four-fold greater prevalence of the outlet syndrome in women.11,12 The effect of prolonged hyperabduction of the arms in some jobs and the repetitive strain changes of abnormal neck postures with forward thrust of the head and neck in keyboard workers have also been implicated.13 The latter is thought to result in muscle imbalance with tightly contracted, “spastic” scalene muscles and weak trapezius. Mackinnon14 believes that these postures and muscle imbalances may be responsible for the neck and shoulder pain in TOS. Stretch and strain on the plexus caused by these factors may cause the more distal neurological symptoms.
Moderate trauma, particularly whiplash injuries, is also believed by many to be the proximate cause of TOS, and accounts for most cases of TOS with an identifiable cause. Anatomic anomalies at the outlet are believed to be simply predisposing factors. Up to 75% of patients have neck pain and a similar number had a prior injury, frequently an auto accident.15 Another theory holds that acute or chronic injury to the scalene muscles leads to persistent spasm and eventually to changes in the fine structure of the muscle and fibrosis of the muscle, which compresses the plexus.16 The roles of litigation and secondary gain in these settings of trauma cannot be ignored.
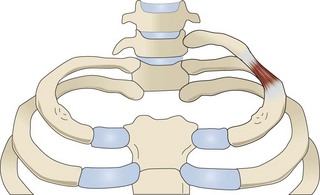
Even though all these factors have an uncertain significance, clear anatomical proof is available that cervical ribs, anomalous first ribs, and the fibrous bands arising from the tips of cervical ribs or abnormally long C7 transverse processes can elevate and kink the proximal lower trunk or the T1 spinal nerve as they pass over the first rib within the scalene triangle (Figure 22.3). The distortion of the lower plexus associated with these particular anomalies is virtually always associated with a clear neurologic deficit.4
Indications and constraints
The two neurogenic syndromes
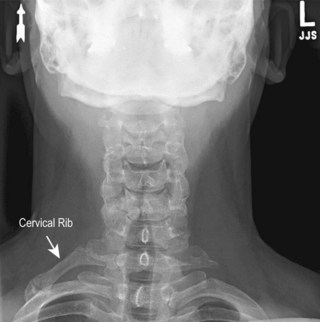
The first type, termed the “true” or “classic” syndrome, is rare, occurring in about one per million people and almost exclusively affecting young to middle-aged females at a 9 : 1 ratio with men. It is virtually always associated with radiologically visible cervical ribs or elongated, downward-sloping and beaked C7 transverse processes (Figure 22.4).17 First described by Gilliatt et al.18 in 1970, it presents with mild-to-moderate aching pain in the ulnar side of the forearm, sometimes extending to the ulnar hand. Mild paresthesias are frequent along the medial side of the forearm as well. These early symptoms are rarely severe enough to cause patients to seek medical attention and may be present for years before definitive diagnosis. Shoulder and arm pain is uncommon. Vasomotor disturbances are rare, as is a history of trauma. Sensory loss in the medial forearm is mild; it occasionally may involve the ulnar side of the hand. The presenting complaint is nearly always progressive hand weakness and atrophy of the intrinsic hand muscles. Muscles of the ulnar forearm are sometimes also involved. The most dramatic wasting is in the thenar eminence, especially in the abductor pollicis brevis, producing a “guttering” in the lateral thenar area, termed Gilliatt-Sumner hand (Figure 22.5).19 Unfortunately, the benign early symptoms lead to delay, and cause patients to have significant motor impairment by the time of presentation and diagnosis. This weakness can severely limit strength and mobility of the hand, especially in thumb function. Left untreated, the weakness and atrophy of all the intrinsic hand muscles will be progressive.
Cervical ribs are uncommon, occurring in less than 1% of the population; abnormal cervical transverse processes may be rarer still. Cervical ribs are twice as common in females, which may account for their higher incidence of “true” TOS. These abnormalities are bilateral in 50% of cases, but the smaller rib or process is often the symptomatic one. Many cervical ribs are asymptomatic (Figure 22.6). Cervical ribs may be “complete,” attaching to the first rib near the intersection of the scalenes, but size is of little importance. Often the rib or transverse process abnormalities are overlooked. It is usually not the bone, but the fibrous band extending from its tip that is compressing the lower trunk. This firm, fibrous band runs from the tip to insert on the first rib just anterior to the insertion of the middle scalene (Figure 22.7). At times the band appears to be the fibrous anterior medial edge of the middle scalene muscle. At surgery, this fibrotic band is seen to be elevating and kinking the lower trunk of the brachial plexus and often involving the T1 spinal nerve.
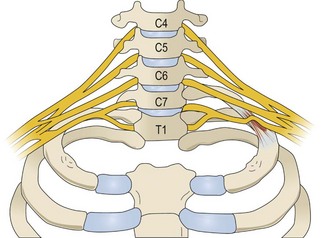
Figure 22.7 Schematic diagram of a left sided “true” TOS. The fibrous band is elevating and deforming the lower trunk.
The “classic” TOS is characterized not only by the combination of intrinsic hand muscle atrophy and typical bony abnormalities on imaging studies. It also has a characteristic electrodiagnostic picture. Patients demonstrate a chronic axonal (axon-loss) neuropathy of the lower trunk especially involving T1 axons. Nerve conduction studies show: (1) a low amplitude median motor unit action potential (MUAP) measured at the abductor pollicis brevis; (2) a low amplitude ulnar sensory nerve action potential (SNAP); (3) a slightly low-to-normal ulnar MUAP; (4) a normal median nerve sensory amplitude. The sensory amplitude measured in the medial antebrachial cutaneous (MAC) nerve is also absent or reduced. Electromyographic (EMG) needle electrode studies show a chronic neurogenic lower trunk plexopathy with decreased numbers of motor units and increased amplitude and duration of the remaining motor units, principally in the median nerve innervated thenar muscles. Less severe, but similar changes can be seen in ulnar-innervated intrinsic muscles as well. Fibrillations are sparse and are largely limited to the abductor pollicis brevis, though not exclusively so.17,20 Conduction velocities in the median and ulnar nerves are normal (Table 22.1). Somatosensory evoked potentials (SSEPs) are often obtained and tend to be normal on median nerve stimulation and delayed and reduced on ulnar nerve stimulation. Neither SSEP nor F-wave studies are of much value here, because the findings on nerve conduction and electromyography are so characteristic.
Table 22.1 Electrodiagnostic findings in classic thoracic outlet syndrome.*
| Amplitudes | Median | Ulnar |
|---|---|---|
| Motor | Markedly reduced | Slightly reduced or normal |
| Sensory | Normal | Reduced |
| Conduction velocity | Normal | Normal to slightly reduced |
* Note that the amplitudes for the medial antebrachial cutaneous nerve are markedly decreased or absent.
The importance of the profound decrease, or even loss, of SNAP of the MAC nerve has become understood in the past decade.21 Seror22 has shown abnormal MAC amplitudes in patients with very early findings (no atrophy) of true TOS. This decrease has been present in nearly all patients with the true neurogenic syndrome so evaluated in the past 2 decades.23 Fibers of the MAC nerve are purely derived from the T1 spinal nerve, and these amplitude changes clinch localization of the injury in this syndrome to the proximal lower trunk of the brachial plexus.
The second type of TOS is far more common, accounting for over 90% of patients with this diagnosis. It is widely reported, analyzed, and discussed, especially in the vascular and thoracic surgery literature. It is primarily a pain syndrome. It is this group in which the history of prior trauma and repetitive strain injury figure prominently. Patients present with combinations of arm, shoulder, and neck pain that is quite often disabling. The pain is typically worsened by exertion or by elevating the arms. It is usually dull, deep, and diffuse, and it does not follow a clear dermatomal pattern. Headache and chest pain may also occur. Distal paresthesias are common and of varied distributions, though they most usually involve the medial (ulnar) forearm and the ulnar side of the hand, at least suggesting involvement of the lower trunk. Although paresthesias may progress to subjective numbness in some areas, clearly defined sensory loss is quite rare. Complaints of hand weakness and clumsiness are frequent, but objective weakness and atrophy are almost never present. Vasomotor instability is prominent, with coolness, blanching, hyperemia, and cyanosis precipitated both by cold and by emotional stimuli. The bony abnormalities universally seen in the “true” syndrome are rarely seen here, accounting for only 5% to 8% of patients in several large series reporting this type of TOS. Standard electrodiagnostic studies are normal. This form of the syndrome is described by some authors as the “nonspecific,” “disputed,” or “common” neurogenic TOS because of the paucity of demonstrable neurologic or radiologic abnormalities. Many basic aspects of this syndrome are in dispute, even among the surgeons who treat it frequently. The lack of objective findings makes the diagnosis very physician-dependent, and even among the most experienced surgeons, there are significant differences as to what set of symptoms or diagnostic tests constitute this syndrome.3,7 Each surgeon appears to have a unique personal set of diagnostic criteria.
The absence of clear neurologic deficits or electrodiagnostic abnormalities has led to a search for ancillary tests that might make or confirm the diagnosis. Initially, “provocative” tests were used to test for obliteration of the radial pulse, assuming that if the subclavian or axillary artery was compressed, there would also be compression of the brachial plexus in the thoracic outlet. These tests include Adson’s maneuver, hyperabduction of the arms (Wright’s test), the exaggerated military brace position (Halstead’s position), and the elevated arm stress test (EAST) of Roos (Table 22.2). These tests examined the wrong system – the vascular system – and have been shown to be unreliable. They are now considered positive if they reproduce or increase patient symptoms, but loss of the radial pulse is no longer considered a significant finding. The specificity of these tests is questionable. Several studies have shown that 50% or more of normal people have radial pulse loss in each of these tests.24,25 The EAST is considered the most reliable test; positive if it reproduces symptoms in less than 3 minutes when the arm is held in the “hold-up” or “surrender” position while rapidly opening and closing the hands. Separate trials, however, have shown that it can produce pain and paresthesias in 35% to 75% of controls.24,25
Table 22.2 Provocative tests initially used to determine presence, absence, or marked reduction in radial pulse, but are now used to reproduce or worsen patient symptoms
| Adson’s Maneuver | Head is turned to the symptomatic side and neck is hyperextended. Patient takes and holds a deep breath. Some descriptions have the head away from the symptomatic side. |
| Wright’s Hyperabduction Test | Arms are fully abducted and raised above the head with elbows extended. |
| Halsted’s Military Brace Test | Shoulders are thrust backward and downward in an exaggerated version of the military posture of attention. |
| Elevated Arm Stress Test (EAST) of Roos | Both arms are in the 90° abducted and externally rotated (hold-up) position. Shoulders and elbows are in the coronal plane of the torso. The hands are then opened and closed for 3 minutes. The test is positive if symptoms are reproduced or increased in less than 3 minutes. |
Electrodiagnostic tests have also been evaluated as diagnostic aids in this group and are also controversial. There are usually no abnormalities in those standard nerve conduction and EMG tests used in the diagnosis of “true” TOS. Slowed ulnar conduction across the thoracic outlet, once widely used, is now largely discredited. SSEPs showed delayed, decreased ulnar potentials in some studies. Others have not found SSEPs to be reliable in this setting.26,27 When the arms are tested in both the relaxed and the EAST position, reliable changes in latency of the evoked potential secondary to position change have not been reliably demonstrated either.27 The principal use of electrodiagnostics in this setting is to identify or rule out other peripheral neuropathies such as carpal tunnel, ulnar entrapment, as well as cervical radiculopathies. Surgeons using these tests in the work-up of TOS usually consider TOS a diagnosis of exclusion and exclude these diagnoses first. Other surgeons do not feel electrical studies are of any value whatsoever and do not order them.
Despite these problems, there may indeed be an element of plexus compression in some “disputed” patients, as a positive Tinel’s sign on percussion in the supraclavicular area occurs occasionally in patients with the “common” syndrome. Also, the marked reduction in MAC nerve SNAPs so characteristic of the “true” syndrome may occur in these patients as well. In 3 studies21,22,28 of patients presenting with a symptom complex most compatible with the “disputed” TOS without any objective neurologic findings or abnormality on standard electrodiagnostic studies, specific testing of MAC nerve conduction revealed a significant decrease in amplitude in the symptomatic arm in comparison with both the contralateral arm and controls. In one of the studies,22 75% of patients had a cervical rib or an abnormal C7 transverse process. It is possible that this picture of female gender, pain and paresthesia in the arm, a bony anomaly in the thoracic outlet, and abnormal MAC nerve conduction, may represent an early stage of the “true” syndrome. It does seem quite reasonable that there should be an early stage of the “true” syndrome, as atrophy takes some time to develop.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree