KEY POINTS
• Third-trimester bleeding complicates about 4% of all pregnancies.
• Serious causes include placenta previa, abruption, and vasa previa and can result in significant maternal and/or fetal compromise.
• Availability of blood products and support systems is important for optimal patient management.
• Absence of placenta previa should be confirmed by ultrasound before proceeding with digital examination of the cervix.
VAGINAL BLEEDING
Background
Definition
• Third-trimester bleeding is defined as any episode of vaginal bleeding that occurs after 24 completed weeks of pregnancy.
• Third-trimester bleeding complicates about 4% of all pregnancies.
• Vaginal bleeding during pregnancy is a worrisome symptom to the patient and is usually brought to the attention of her physician at the time that it occurs during pregnancy.
Etiology
• In approximately 50% of cases, vaginal bleeding is secondary to placental abruption or placenta previa. Both of these conditions carry significant risk of maternal and fetal morbidity and mortality and therefore must be expeditiously diagnosed.
• Once these two life-threatening situations are convincingly excluded as a cause of bleeding, attention can be turned to alternate causes of vaginal bleeding in pregnancy.
Evaluation
History
The following information should be obtained:
• Is there a history of trauma?
• What is the amount and the character of the bleeding?
• Is there pain associated with the bleeding?
• Is there a history of bleeding earlier in the pregnancy?
Physical Examination
• Vital sign measurement, including pulse pressure; normal vital signs are reassuring; however, they can be misleading because hypotension and tachycardia are signs of serious hypovolemia, and generally not present until significant blood loss has occurred. Additionally, mild tachycardia can be a normal finding in pregnancy.
• Fetal heart rate and/or category of continuous fetal heart rate tracing.
• Physical examination, initially excluding speculum and digital pelvic examination until after ultrasound is complete.
• Assessment of uterine activity.
• Ultrasound examination of the uterus, placenta, and fetus (transabdominal first and then transvaginal when indicated).
• Speculum and digital pelvic examination once placenta previa has been excluded.
Laboratory Tests
• Hemoglobin and hematocrit determination.
• Coagulation studies when placental abruption is suspected or when there has been significant hemorrhage, including prothrombin time, partial thromboplastin time, platelet count, fibrinogen level, and fibrin split products.
• Red-top tube of blood to perform a bedside clot test.
• Blood type and crossmatch.
• Anti-D immunoglobulin for those who are Rh(D) negative to protect against sensitization.
• Urinalysis for hematuria and proteinuria.
• Apt test may be used to determine maternal or fetal source of bleeding. (Mix vaginal blood with an equal part of 0.25% sodium hydroxide. Fetal blood remains red; maternal blood turns brown.) In general, fetal bleeding will be apparent on fetal heart rate tracing and intervention should not be delayed for Apt testing.
• Kleihauer-Betke (K-B) test is used to quantify fetal to maternal hemorrhage. However, it is positive in only a small proportion of placental abruptions. While the K-B test is helpful to assure adequate anti-D immunoglobulin dosing, it is generally not helpful for diagnosis of abruption (1,2).
PLACENTAL ABRUPTION
Background
Definition
Placental abruption (also known as abruptio placentae) occurs when a normally implanted placenta completely or partially separates from the decidua basalis after the 20th week of gestation and before the third stage of labor.
Incidence
Placental abruption occurs in approximately 1 in 100 deliveries and accounts for 15% of perinatal mortality (3,4).
Classification
Placental abruptions are graded by clinical criteria. Ultrasound is not an accurate or reliable method for diagnosis or classification. Clinically, the classification of abruption can be helpful when deciding on the need for interventions and the need for further monitoring (Fig. 9-1).
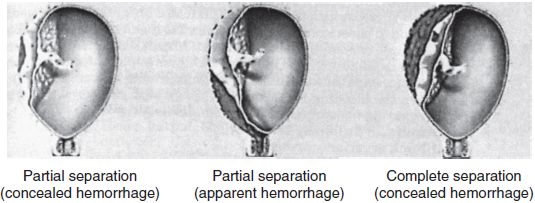
Figure 9-1. Types of placental abruption. (From Beckmann CRB, Ling FW. Obstetrics and gynecology. 6th ed. Lippincott Williams & Wilkins, 2009).
• Grade 1, mild (40% of abruptions):
• Vaginal bleeding is slight or absent (less than 100 mL).
• Uterine activity may be slightly increased.
• Uterine activity often described as having closely spaced, low-intensity contractions—a hyperstimulation-type pattern.
• No fetal heart rate abnormalities are present.
• No evidence of shock or coagulopathy.
• Grade 2, moderate (45%):
• External bleeding may be absent to moderate (100 to 500 mL).
• Uterine tone may be increased. Tetanic uterine contractions and uterine tenderness may be present.
• Fetal heart tones may be absent and, when present, often show evidence of fetal distress.
• Maternal tachycardia, narrowed pulse pressure, and orthostatic hypotension may be present.
• Early evidence of coagulopathy may be present (fibrinogen 150 to 250 dL).
• Grade 3, severe (15%):
• External bleeding may be moderate or excessive (greater than 500 mL) but may be concealed.
• The uterus is often tetanic and tender to palpation.
• Fetal death is common.
• Maternal shock is usually present.
• Coagulopathy is frequently present.
Etiology
The cause of placental abruption is unknown, but defective placental vasculature has been postulated to be a contributing factor. In the following conditions, the incidence of placental abruption is increased: (3,5)
• Preeclampsia and hypertensive disorders
• History of placental abruption (recurrence rate ~10%)
• High multiparity
• Relatively older maternal age
• Trauma, both direct and indirect uterine traumas
• Cigarette smoking, in a dose-responsive fashion, which is synergistic with hypertension (5)
• Illicit drug use, most notably cocaine use
• Excessive alcohol consumption
• Preterm, premature rupture of the membranes, where the risk increases with length of latency
• Rapid uterine decompression (e.g., after delivery of the first fetus in a twin gestation or rupture of membranes with polyhydramnios)
• Uterine leiomyomas, especially if located retroplacentally, rapidly enlarging, or degenerating
Diagnosis
Clinical Manifestations
• The diagnosis of placental abruption is made by clinical findings, with the symptoms of vaginal bleeding, abdominal pain, uterine tenderness, and uterine contractions.
• Vaginal bleeding is present in 80% of patients and concealed in 20%.
• Pain is present in most cases of placental abruption and is usually of sudden onset, constant, and localized to the uterus, low abdomen, and lower back.
• Localized or generalized uterine tenderness and increased uterine tone are found with the more severe forms of placental abruption.
• The uterus may increase in size with placental abruption when the bleeding is concealed. This may be monitored by serially measuring abdominal girth and/or fundal height.
• Amniotic fluid may be bloody.
• Shock is variably present.
• Fetal compromise is variably present.
• Placental abruption may cause rapidly progressive preterm labor and/or preterm premature rupture of membranes.
Laboratory Findings
Laboratory findings that are frequently helpful in the diagnosis include (6)
• Consumptive coagulopathy
• Placental separation precedes the onset of the consumptive coagulopathy, which in turn progresses until the uterus is evacuated.
• Coagulation occurs retroplacentally as well as intravascularly, with secondary fibrinolysis.
• Levels of fibrinogen, prothrombin, factors V and VIII, and platelets are decreased.
• Fibrin split products are elevated, adding an anticoagulant effect.
• Hypofibrinogenemia occurs within 8 hours of the initial separation.
Ultrasonography
Ultrasonography is very poorly sensitive in making the diagnosis.
• The three locations of placental hemorrhage are
• Subchorionic (more common less than 20 weeks)
• Retroplacental (more common greater than 20 weeks)
• Preplacental (unusual)
• Symptoms associated with retroplacental hemorrhage are frequently the most severe.
• The sensitivity of ultrasonography in detecting placental abruption is only approximately 25% to 50% at best (7).
• If abruption is visualized on ultrasound, the predictive value is high (88%) (7).
Treatment
Management
• Mild placental abruption
• Close observation is required to assure maternal stability and reassuring fetal status. The facility should be fully capable of immediate delivery should the condition of the patient or fetus deteriorate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


