Source: From FIGO Committee on Gynecologic Oncology. Current FIGO staging for cancer of the vagina, fallopian tube, ovary, and gestational trophoblastic neoplasia. Int J Gynaecol Obstet. 2009;105(1):3–4, with permission.
Table 6.2 American Joint Commission on Cancer (AJCC, 7th Edition) Staging of Vaginal Cancer
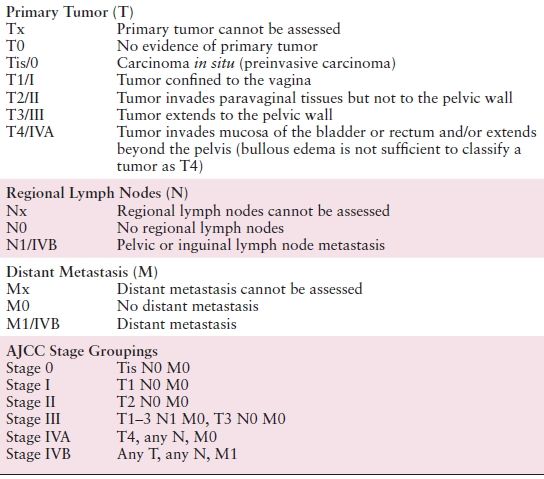
Source: Edge SB, Byrd DR, Compton CC, et al. American Joint Committee on Cancer, American Cancer Society. AJCC Cancer Staging Manual, 7th ed. New York: Springer; 2010:388.
PATHOLOGIC CLASSIFICATION
Squamous Cell Carcinoma
The most common malignant tumor of the vagina is SCC, representing about 80% to 90% of primary vaginal cancers. These tumors occur in older women and are most often located in the upper, posterior wall of the vagina. For a neoplasm to be considered a vaginal primary, there must not be involvement of the cervix or vulva or a history of cervical cancer for 5 years prior to the diagnosis. Histologically, keratinizing, nonkeratinizing, basaloid, warty, and verrucous variants have been described. Tumors may also be graded as well, moderately, or poorly differentiated, based on a combination of cytologic and histologic features. However, there is little correlation between tumor grade and survival.
Verrucous carcinoma is a rare distinct variant of well-differentiated SCC, usually with the appearance of a large, well-circumscribed, soft, cauliflower-like mass. Verrucous carcinoma may recur locally after surgery but rarely, if ever, metastasizes.
VAIN is a precursor of SCC and is graded from 1 to 3, based on the thickness of epithelial involvement. Alternatively, VAIN can be classified as low or high grade. High-grade lesions indicate involvement of the outer third of the mucosa and include CIS, which encompasses the entire thickness of the epithelium. The true incidence of VAIN and its rate of progression to invasive carcinoma are unknown, ranging in several series from 9% to 28%. High-risk HPV was noted in 35% of VAIN 1 and 94% of VAIN 3 lesions. Comparison of the distribution of HPV types in the vagina, vulva, and cervix suggests that VAIN is more closely related to CIN than to VIN.
Clear Cell Adenocarcinoma and Vaginal Adenosis
DES-associated CCA has a predilection for the upper third of the vagina and the exocervix. It is frequently located at or near the lower margin of the zone of glandular tissue in the vagina or cervix. Most CCAs are exophytic and superficially invasive. About 97% will be associated with mucosal adenosis. CCA is mainly composed of clear and hobnail-shaped cells. The major determinant of outcome in CCA is stage, but some pathologic features are statistically associated with better outcome, including a tubulocystic growth pattern, size less than 3 cm2, and less than 3 mm of stromal invasion.
Vaginal adenosis is a condition in which müllerian-type glandular epithelium is present after vaginal development is complete. Although adenosis is the most common histologic abnormality in women exposed to DES in utero, it is not strictly confined to this population. Atypical adenosis of tuboendometrial type appears to be a precursor lesion of CCA.
Other Adenocarcinomas
Primary adenocarcinoma of the vagina is rare and occurs predominantly in postmenopausal women.
Melanoma
Malignant melanoma of the vagina accounts for less than 3% of vaginal neoplasms. In contrast to SCC, the most common locations of vaginal melanoma are the lower third and the anterior vaginal wall. Grossly, these tumors are typically pigmented and show considerable variation in size, color, and growth patterns, being polypoid or nodular in the majority of cases. Immunohistochemical stains are frequently positive for S100 protein, HMB-45, and melan-A. Tyrosinase and MART-1 are useful markers when S100 is negative or only focally positive. Tumor thickness correlates with prognosis and may be measured by the method of Breslow.
Mesenchymal Tumors
Embryonal RMS is a rare pediatric tumor. The botryoid variant, or sarcoma botryoides, is the most common malignant vaginal tumor in infants and children. Ninety percent of cases occur in children younger than 5 years of age. Sarcoma botryoides has a characteristic macroscopic appearance consisting of multiple gray-red, translucent, edematous, grapelike masses that fill the vagina and may protrude from it.
Leiomyosarcoma is the most common vaginal sarcoma in adults. Smooth muscle tumors 3 cm or greater in diameter have an increased risk of recurrence. Although they may originate in any part of the vagina, most are submucosal.
PROGNOSTIC FACTORS INFLUENCING CHOICE OF TREATMENT
KEY POINTS
- Primary malignancies of the vagina are all staged clinically.
- The most common malignant tumor of the vagina is SCC.
- VAIN is a precursor of SCC.
- Exposure to DES in utero is associated with the development of clear cell adenocarcinoma.
- Stage of disease is the dominant prognostic factor in terms of outcome.
- Vaginal melanoma has a higher propensity for the development of distant metastases, and these patients do more poorly than patients with SCC.
Invasive Squamous Cell Carcinoma
Stage of disease is the dominant prognostic factor in terms of outcome. In the report by Creasman et al. (1998), the 5-year survival rate was 96% for patients with stage 0, 73% for stage I, 58% for stage II, and 36% for those with stage III and IV diseases, respectively. In Perez’s series, including 165 patients with primary vaginal carcinomas treated with definitive RT, the 10-year actuarial disease-free survival (DFS) was 94% for stage 0, 75% for stage I, 55% for stage IIA, 43% for stage IIB, 32% for stage III, and 0% for those with stage IV.
The impact of lesion location has been controversial. Several investigators have shown better survival and decreased recurrence rates for patients with cancers involving the proximal half of the vagina when compared with those in the distal half or those involving the entire length of the vagina. In addition, lesions of the posterior wall have a worse prognosis than those involving other vaginal walls (10-year recurrence rates of 32% and 19%, respectively), which probably reflects the greater difficulty of performing adequate brachytherapy procedures in this location.
The prognostic importance of lesion size has also been controversial. Chyle et al. (1996) noted that lesions measuring less than 5 cm in maximum diameter had a 20% 10-year local recurrence rate compared to 40% for those lesions larger than 5 cm. Similarly, in the Princess Margaret Hospital experience and more recently in the Stanford experience, tumors larger than 4 cm in diameter fared significantly worse than smaller lesions. Other data suggest that disease volume, a likely surrogate for stage or lesion size, adversely impacted survival as well as local control.
Several series have shown histologic grade to be an independent, significant predictor of survival. Chyle et al. (1996) also noted histology was a significant predictor of outcome, with a higher incidence of local recurrence in patients with adenocarcinoma compared with SCC (52% and 20%, respectively, at 10 years), as well as a higher incidence of distant metastases (48% and 10%, respectively) and lower 10-year survival rate (20% vs. 50%).
Other Histologies
An increased propensity for distant metastases to the lung and supraclavicular nodes has been reported in patients with CCA. Stage, tubulocystic pattern, size less than 3 cm, and depth of invasion less than 3 mm were all noted to be associated with superior survival.
Vaginal melanoma has a higher propensity for the development of distant metastases, and affected patients do more poorly than patients with SCC.
Patients with malignant mesenchymal tumors of the vagina do less well than those with invasive SCC. Specific, adverse prognostic factors for vaginal sarcoma identified by Tavassoli and Norris included infiltrative versus pushing borders, high mitotic rate of 5 or more mitoses per 10 HPFs, size greater than 3 cm in diameter, and cytologic atypia.
GENERAL MANAGEMENT: TREATMENT OPTIONS AND OUTCOME BY FIGO STAGES
KEY POINTS
- Treatment options for VAIN range from partial or complete vaginectomy to more conservative approaches such as local excision, electrocoagulation, laser vaporization, topical 5% fluorouracil, or intracavitary brachytherapy.
- Surgery may be preferable in select stage I and II patients with small, superficially invasive SCC lesions at the apex and upper third of the posterior or lateral vagina.
- External beam radiotherapy (EBRT) is advisable in patients with deeply infiltrating or poorly differentiated stage I and II lesions and in all patients with stage III to IVA disease.
- Consideration should be given to delivering cisplatin-based chemotherapy concurrently with RT in patients with advanced vaginal cancer.
Vaginal Intraepithelial Neoplasia—Carcinoma In Situ
VAIN has been approached both surgically and medically by multiple investigators. Treatment options range from partial or complete vaginectomy to more conservative approaches such as local excision, electrocoagulation, laser vaporization, topical 5% fluorouracil (5-FU) administration, or ICB. For patients in whom invasive disease cannot be ruled out, as well as for those who fail conservative therapy, surgical resection remains the treatment of choice. Overall, the reported control rates are very similar among the different approaches, ranging from 48% to 100% for laser, 52% to 100% for colpectomy, 75% to 100% for topical 5-FU, and 83% to 100% for RT. The degree of VAIN and the age and general health of the patient are important treatment considerations.
Partial colpectomy is favored by many for the treatment of focal VAIN without any prior history of pelvic RT. Patients who have received prior pelvic RT, wherein partial colpectomy would have high risk of fistula formation, may benefit from a medical approach with topical application of 5-FU. This acts by inciting a desquamation of the vaginal squamous epithelium, which later reepithelializes with presumably normal cells. Several schedules of topical 5-FU have been reported; however, one preferred schedule is one third applicator weekly for 10 weeks. Regardless of which 5-FU application schedule is chosen, it is important that the perineal skin be protected with a topical ointment, such as zinc oxide, to prevent painful vulvar erosions. More recently, investigators have demonstrated the feasibility and efficacy of topical imiquimod in the treatment of VAIN, with cure rates of up to 86% reported in small single institution studies. Imiquimod is a heterocyclic imidazoquinoline amine that acts through Toll-like receptor 7 to induce cytokine expression and subsequent activation of both the innate and adaptive immune responses. This topical medication is generally well tolerated with the majority of side effects limited to mild skin reactions, such as redness, swelling, itching/burning, tenderness, and flaking.
Partial or total vaginectomy has been considered by many to be an acceptable treatment for VAIN. However, one of its main drawbacks is shortening or stenosis of the vagina, frequently with poor functional results. Prior RT is probably a contraindication to vaginectomy owing to significantly increased morbidity. Control rates of 66% to 100% following partial colpectomy have been achieved.
RT has a long history of documented efficacy with control rates ranging between 80% and 100%, and a significantly better therapeutic ratio than other modalities. Using conventional low dose rate (LDR) ICB techniques, the entire vaginal mucosa should receive between 50 and 60 Gy, given the high incidence of multicentricity; the area of involvement should receive 70 to 80 Gy, in one or two implants, prescribed to the mucosal surface. Higher doses may cause significant vaginal fibrosis and stenosis. Perez et al. (1999) reported only one distal local failure in the 20 patients treated for CIS. A more recent publication from Blanchard et al. (2011) reported only one “in-field” recurrence in 28 patients treated with LDR brachytherapy for VAIN 3. Pelvic recurrences or distant failures have not been observed in the absence of invasive component after ICB.
There have been some reports in the literature regarding the use of high dose rate (HDR) ICB for patients with VAIN 3; however, data are limited, and there is a lack of consensus regarding fraction schedules. Based on the excellent local control and functional results obtained with LDR-ICB, this remains the treatment of choice when definitive RT is used, unless unavailable.
Invasive Squamous Cell Carcinoma
Surgical Approach and Outcomes
In general, SCC of the vagina has been treated with RT. However, several surgical series have reported acceptable to excellent outcomes in well-selected patients, with survival rates after radical surgery for stage I disease ranging from 75% to 100%. Cases in which surgery may be the preferred treatment include selected stage I and II patients with lesions at the apex and upper third of the posterior or lateral vagina that could be approached with radical hysterectomy, upper vaginectomy, and pelvic lymphadenectomy, providing adequate margins for very superficial lesions. Lesions in the lower third of the vagina would require vulvovaginectomy in addition to dissection of inguinofemoral nodes to achieve negative margins. If the margins are found to be close or positive after resection, adjuvant RT is recommended. However, for lesions at other sites, and those cases requiring more extensive resection, definitive RT is the treatment of choice since it offers excellent results. Exenteration should be reserved for those with central failure after RT or as primary therapy in those with disease not fixed to the bone.
Advanced-stage patients should receive definitive RT, probably in combination with concurrent chemotherapy, although the role of combined modality therapy is unknown and is used as an extrapolation from the cervical data.
Radiation Therapy Techniques and Outcome
Stage I
In patients with stage I lesions, usually 0.5 to 1 cm thick that may involve one or more vaginal walls, it is important to individualize radiation therapy techniques to obtain optimal functional results. Superficial lesions can be adequately treated with ICB alone using afterloading vaginal cylinders. The entire length of the vagina is generally treated to a mucosal dose of 60 to 65 Gy (LDR), and an additional mucosal dose of 20 to 30 Gy is delivered to the area of tumor involvement. For lesions thicker than 0.5 cm at the time of implantation, it is advisable to combine ICB and interstitial brachytherapy (ITB) with a single-plane implant to increase the depth dose and limit excessive irradiation to the vaginal mucosa. An additional 15 to 20 Gy at a depth of 0.5 cm beyond the plane of the implant will be delivered with the ITB such that the base of the tumor receives between 65 and 70 Gy, with the involved vaginal mucosa receiving an estimated 80 to 100 Gy. The proximal and distal vaginal mucosal doses should be limited to 140 and 100 Gy, respectively. The optimal fractionation schedule and dose for HDR brachytherapy remain to be defined, especially for HDR monotherapy. The HDR dose schedules proposed in the American Brachytherapy Society consensus guidelines are for HDR brachytherapy combined with EBRT and are based on empirical protocols or extrapolated from LDR parameters.
There is general consensus that EBRT is advisable for larger, more infiltrating, or poorly differentiated tumors that may have a higher risk of lymph node metastasis. The whole pelvis is treated to 45 to 50 Gy to the parametria and pelvic sidewalls. Chyle et al. (1996) recommended EBRT in addition to brachytherapy for stage I disease to cover at least the paravaginal nodes and, in larger lesions, to cover the external and internal iliac nodes. About 95% to 100% of local control has been achieved with intracavitary and interstitial techniques, with 5-year survival for patients with stage I disease treated with RT alone ranging from 70% to 95% (Table 6.3).
Table 6.3 FIGO Stage I and II Vaginal Cancers: Treatment Approach and Results
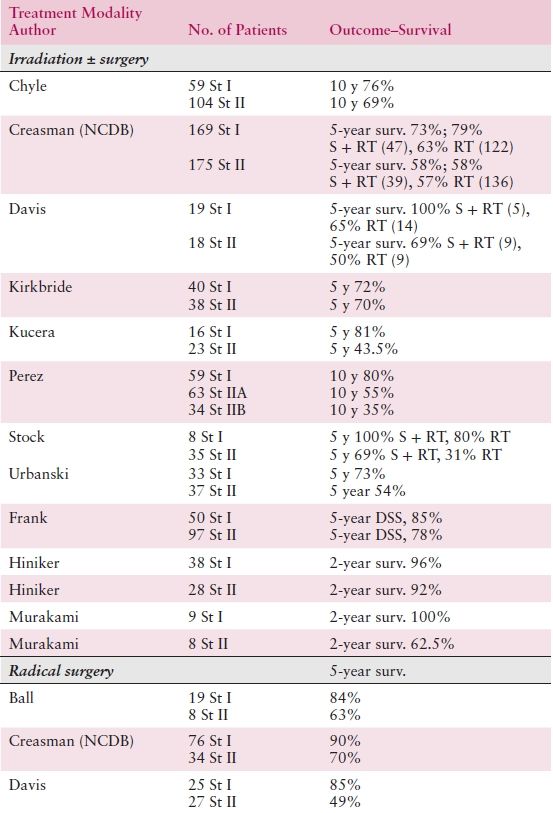
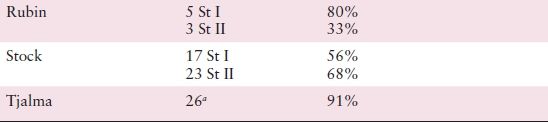
aFour patients received adjuvant irradiation.
St, stage; RT, radiotherapy; S, surgery; surv., survival; DSS, disease-specific survival.
Source: Adapted from Cardenes VR, Schilder JM
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


