On successfully completing this topic, you will be able to:
describe the principles of treatment of the unconscious patient
understand the concept of secondary brain injury and how to prevent it
identify types of lesion amenable to surgery (extradural and subdural haematoma).
Incidence
Each of the last three Confidential Enquiries have described approximately 40 indirect deaths in women due to disease related to the central nervous system. These include deaths from: subarachnoid haemorrhage; intracerebral haemorrhage; cerebral thrombosis and epilepsy.
The immediate management of the patient unconscious from any cause should be a basic skill of every obstetrician and midwife. The obstetric team should be aware of the potential causes of a decreased level of consciousness and treat the underlying cause, with appropriate specialist assistance where necessary.
Causes of decreased level of consciousness
A B Failure of airway or breathing: hypoxia/hypercarbia
C Failure of circulation: shock or cardiac arrest
D Failure of central nervous system:
eclampsia or epilepsy
intracranial haemorrhage, trauma, thrombosis, tumour or infection
drugs, alcohol or poisoning.
Principles of treatment
Although these principles were developed in the context of trauma cases and traumatic brain injury, the same principles apply to any medical situation that threatens the supply of oxygen to the injured or uninjured brain.
Primary and secondary brain injury
Primary brain injury is the neurological damage produced by the initial event, such as a brain haemorrhage. Secondary (further) brain injury is the neurological damage caused by lack of oxygen delivery to the brain. This may be caused by:
A B – failure of ventilation, caused by airway obstruction or inadequate breathing, resulting in poor oxygenation. In addition, both airway obstruction and inadequate breathing may lead to a rise in arterial carbon dioxide levels. This has direct consequences on intracranial pressure (ICP) (see below).
C – failure of circulation due to shock including hypotension.
D – intracerebral damage may cause an excessive rise in ICP, leading to reduced cerebral perfusion pressure (CPP).
Cerebral perfusion
Cerebral perfusion refers to the supply of oxygenated blood to the brain. The blood supply to the brain is more complex than other organs, because the brain is enclosed inside a rigid box. The volume of this box is fixed, so one component can only increase in volume at the expense of another, or at the expense of an increase in ICP. The main components inside the box are:
brain substance or space-occupying lesions
cerebrospinal fluid
cerebral blood vessels and the blood contained within these vessels
extracellular fluid.
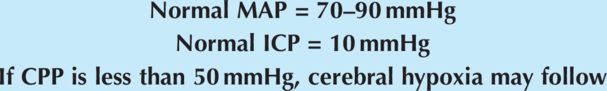
CPP is the mean arterial pressure (MAP) of blood in the brain minus the resistance to flow from the mean ICP:
any factors affecting MAP or ICP will affect CPP and potentially contribute to further neuronal damage
adequate blood pressure (MAP) must be maintained to maintain CPP
any rise in volume of intracranial contents may need to be controlled if the normal mechanism of cerebral autoregulation of ICP has failed:
brain tissue can increase in volume as a result of tumour growth or there may be increased volume caused by blood clot; both conditions may require surgery
cerebrospinal fluid can increase in volume if there is an obstruction to free drainage of the fluid, e.g. by blood clots leading to hydrocephalus and can be drained by temporary or permanent surgical shunts
cerebral blood volume can increase if the arterial carbon dioxide levels are allowed to rise resulting in cerebral vasodilatation; carbon dioxide levels can be reduced by maintaining a clear airway and controlling ventilation to restore a normal level of PaCO2
extracellular fluid levels can increase as a result of response to injury, such as around tumours or following cell damage caused by a major head injury; this is difficult to treat but careful fluid management avoiding excess intravenous fluids will be part of the care
raised ICP may also be due to obstruction of venous drainage from the head from pressure on the neck veins, head down position or excess intrathoracic pressure.
There are limits beyond which the MAP itself will contribute to a rise in ICP: systolic BP >160 mmHg. This rise may be caused by known factors such as pre-eclampsia and may lead to a disastrous intracranial haemorrhage. Some women may have unknown risk factors, such as an intracranial aneurysm, and will be particularly vulnerable to surges in MAP.
Priorities in management to prevent secondary brain injury
1. Primary survey and resuscitation
2. Assessment of fetal wellbeing and viability
3. Secondary survey.
It follows that preventing a rise in ICP or a fall in cerebral perfusion is vital for the overall management and prevention of brain injury.
1. Primary survey and resuscitation
A Airway
Clear the airway. A patient with a reduced level of consciousness is more likely to have a compromised airway as the tongue falls back into the posterior pharynx. Further, she is at risk of aspiration as she has obtunded laryngeal reflexes.
B Breathing
Adequate ventilation ensures that the brain receives blood containing enough oxygen, thereby preventing further brain injury. Adequate ventilation prevents the accumulation of carbon dioxide. Ventilation may be impaired by a reduced level of consciousness. Raised intrathoracic pressure (as happens in tension pneumothorax) will compromise venous drainage from the head and raise ICP.
C Circulation
An adequate BP is required to maintain CPP. Use fluids and vasopressors appropriately. In a trauma situation, hypotension resulting from other injuries must be swiftly recognised and managed to prevent secondary brain injury. It is equally important to remember that excessive fluids are rarely needed in an isolated head injury and may contribute to worsening cerebral oedema.
In trauma, never assume that an isolated head injury is the cause of hypotension. Scalp lacerations may bleed profusely but not sufficiently to cause shock. Always presume that hypotension is due to lesions outside the brain, not brain injury, and look for a source of blood loss elsewhere or other cause of hypotension such as tension pneumothorax or spinal lesion.
Cushing’s response (progressive hypertension, bradycardia and slowing of respiratory rate) is an acute response to rapidly rising ICP and is a premorbid sign. This needs urgent attention, which may include establishing controlled ventilation, use of mannitol and/or urgent surgery.
D Disability
A decrease in level of consciousness is the marker of brain injury. Generally, the more deeply unconscious a patient becomes and the longer this persists, the more serious is the injury.
AVPU: a rapid assessment of conscious level is made in the primary survey. Is the patient Alert, responding to Voice, only responding to Pain, or Unresponsive?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree