The Newborn Intensive Care Unit
Richard A. Ehrenkranz
Newborn intensive care developed from the concept that a more intensive approach to neonates who require special care (both preterm infants and full-term infants with medical or surgical problems) would result in a significant decrease in neonatal morbidity and mortality. The first newborn special care unit was established at Yale–New Haven Hospital (YNHH) in 1960, and the subspecialty of neonatology evolved during the following years. Remarkable advances have been
made in the care of neonates, and about 900 newborn special care units or newborn intensive care units (NICUs) have been established; each provides essentially everything necessary for the life support of a preterm or sick neonate. Many of the advances in neonatal care have been based on research in developmental physiology, biochemistry, pharmacology, and nutrition, which has increased manyfold the understanding of the uniqueness of neonates, particularly of the very low-birth-weight infant. In addition, advances in medical technology have led to the development and neonatal application of life-support systems, monitors, equipment, and techniques such as ultrasound, computed tomography, and magnetic resonance imaging.
made in the care of neonates, and about 900 newborn special care units or newborn intensive care units (NICUs) have been established; each provides essentially everything necessary for the life support of a preterm or sick neonate. Many of the advances in neonatal care have been based on research in developmental physiology, biochemistry, pharmacology, and nutrition, which has increased manyfold the understanding of the uniqueness of neonates, particularly of the very low-birth-weight infant. In addition, advances in medical technology have led to the development and neonatal application of life-support systems, monitors, equipment, and techniques such as ultrasound, computed tomography, and magnetic resonance imaging.
In many university and large community hospitals today, newborn intensive care is just one component of a perinatal center. Such a center also includes facilities for prenatal evaluation, observation, and care of the fetus and mother both before and during labor; facilities for observation of neonates at risk of difficulties during their adaptation to the extrauterine environment; and facilities for continuing and rehabilitative care of growing preterm infants and of infants recovering from acute problems. In some perinatal centers, observation of high-risk neonates is done within the NICU; in others, within a transitional nursery. In addition, the perinatal center has become a regional resource, accepting transfers of women in premature labor, with toxemia, or with other risk factors that indicate the probable need of maternal or neonatal special care or observation, and accepting transfers of neonates who are preterm or have other medical or surgical problems.
Finally, a NICU may exist in a hospital without an obstetric service (e.g., a free-standing children’s hospital) and then provides care only for transferred neonates.
CHARACTERISTICS OF NEWBORN INTENSIVE CARE UNIT PATIENTS
A large percentage of neonates admitted to NICUs are preterm infants. However, any infant who requires or may require the special attention available within a NICU is an appropriate admission. Because many neonatal problems can be anticipated before delivery, communication between the obstetric and pediatric members of the perinatal center (the perinatologists and the neonatologists, respectively) is essential to optimize management plans.
Factors associated with high-risk pregnancies and infants are listed in Tables 24.1 and 24.2. High-risk pregnancy is associated with social and lifestyle characteristics of the pregnant woman, such as her socioeconomic status, and with her prior obstetric and medical history, such as a history of premature labor or delivery or diabetes mellitus. Some of these factors have been shown to adversely affect maternal well-being with increasing gestation and necessitate a preterm delivery for maternal indications. Other factors develop during the pregnancy or are recognized during the process of labor and delivery, such as oligohydramnios, polyhydramnios, preeclampsia and eclampsia, or meconium staining of the amniotic fluid. The prevalence of second-trimester ultrasound examinations has led to the antenatal diagnosis of many congenital malformations, including diaphragmatic hernia, omphalocele, gastroschisis, and cardiac defects such as hypoplastic left heart syndrome and transposition of the great vessels. However, unexpected medical or surgical problems may be recognized in the immediate neonatal period. Because these risk factors and problems correlate with an increased incidence of fetal and neonatal problems and account for a substantial percentage of perinatal mortality and morbidity, most of these high-risk infants are admitted to a NICU for observation, diagnosis, and management.
TABLE 24.1. FACTORS ASSOCIATED WITH HIGH-RISK PREGNANCIES AND INFANTS: SOCIAL AND HISTORICAL | |
|---|---|
|
Regional Organization of Perinatal Care
Table 24.3 correlates neonatal patient types with the level of perinatal services to be provided by a hospital. Such categorization of perinatal care levels was designated by the first Committee on Perinatal Health in a 1976 publication, Toward Improving the Outcome of Pregnancy, and was useful in the development and organization of coordinated regional perinatal
services. Health care economic pressures since then have tended to undo regionally coordinated perinatal systems by encouraging hospitals to raise their level of obstetric, neonatal, or both types of services. In an effort to respond to this changing environment, functional descriptions were used to define basic, specialty, and subspecialty levels of care by the second Committee on Perinatal Health in a 1993 publication, Toward Improving the Outcome of Pregnancy: The 90s and Beyond. Although the individual needs of the mother and neonate might require different levels of care, maintenance of the mother–infant dyad was urged. Table 24.4 lists the responsibilities of in-hospital perinatal services designated by basic, specialty, and subspecialty care levels. Recommended standards for NICU design have also been proposed; the recommendations reflect the severity of illness and types of patients treated at a hospital.
services. Health care economic pressures since then have tended to undo regionally coordinated perinatal systems by encouraging hospitals to raise their level of obstetric, neonatal, or both types of services. In an effort to respond to this changing environment, functional descriptions were used to define basic, specialty, and subspecialty levels of care by the second Committee on Perinatal Health in a 1993 publication, Toward Improving the Outcome of Pregnancy: The 90s and Beyond. Although the individual needs of the mother and neonate might require different levels of care, maintenance of the mother–infant dyad was urged. Table 24.4 lists the responsibilities of in-hospital perinatal services designated by basic, specialty, and subspecialty care levels. Recommended standards for NICU design have also been proposed; the recommendations reflect the severity of illness and types of patients treated at a hospital.
TABLE 24.2. FACTORS ASSOCIATED WITH HIGH-RISK PREGNANCIES AND INFANTS: CURRENT PREGNANCY LABOR AND DELIVERY AND NEONATAL | |
|---|---|
|
TABLE 24.3. NEONATAL PATIENT TYPES AND LEVEL OF PERINATAL SERVICES | |
|---|---|
|
A reclassification of level II and level III NICU services has been recently considered by the American Academy of Pediatrics Committee on Fetus and Newborn. It has been proposed that level II units be divided into IIa and IIb units and that level III units be divided into IIIa, IIIb, and IIIc units. Level IIa units would care for physiologically immature, moderately ill, or convalescing infants over 1,500-g birth weight or 32 weeks’ gestation, while IIb units could also provide brief periods of mechanical ventilation or continuous positive airway pressure (CPAP) to these infants. Level IIIa units would provide sustained life support (i.e., conventional mechanical ventilation) for infants over 1,000-g birth weight or 28 weeks’ gestation and might perform minor surgical procedures. Level IIIb units would provide comprehensive care for infants under 1,000-g birth weight or less than 28 weeks’ gestation. Those NICUs would also provide such therapies as high-frequency oscillatory ventilation and inhaled nitric oxide, and have prompt on-site access to a full range of pediatric subspecialty and surgical consultants. Hospitals with level IIIc NICUs would provide extracorporeal membrane oxygenation (ECMO) and surgical repair of complex cardiac anomalies.
Related to this discussion of NICU level, several recent studies have reported an association between NICU patient volume and NICU level of care at the hospital of birth on neonatal mortality. Although delivery at a hospital with a large NICU does not guarantee a good outcome, level IIIb and IIIc units with a patient census of at least 15 patients tend to have the best outcomes. This relationship appears to be due to structural and organizational aspects of care that are possible at hospitals with large delivery services and NICUs.
TABLE 24.4. RESPONSIBILITIES OF IN-HOSPITAL PERINATAL SERVICES | ||
|---|---|---|
|
Local Organization of Newborn Care
Newborn nursery services are often divided between the normal newborn nursery and a NICU. Medical staff assigned to the NICU are called to be present at the delivery of any infant believed to be at risk for developing neonatal problems because of the presence of factors associated with high-risk pregnancies (see Tables 24.1 and 24.2). Many of these infants, as well as other infants in whom high-risk clinical findings (see Table 24.2) are observed postnatally, are admitted to the NICU for observation, diagnosis, or management. Most of these infants are transferred to the normal nursery within 12 hours of birth or admission and are considered short-term admissions.
Survival Trends
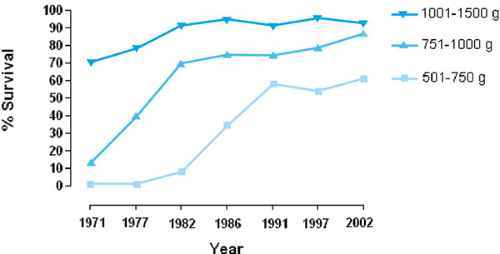
Survival of very low-birth-weight infants improved steadily until the mid-1990s and then tended to plateau. Figure 24.1 graphs survival data for infants born at YNHH in 1971, 1977, 1982, 1986, 1991, 1997, and 2002 with birth weights between 501 and 750 g, 751 and 1,000 g, and 1,001 and 1,500 g. Although survival of infants with birth weights of 1,001 to 1,500 g has ranged from 92% to 96% since 1986, survival of infants with birth weights of 751 to 1,000 g rose from about 76% to 87%, and survival of infants with birth weights of 501 to 750 g almost doubled, increasing from about 35% to 61%. The improved survival for infants with birth weights of 501 to 1,000 g most likely reflects continued refinement in the management of extremely low-birth-weight infants, the widespread use of surfactant replacement therapy since 1991, and antenatal corticosteroids since 1994. Survival of infants with birth weights less than 500 g has, however, remained at less than 20%. Surfactant replacement therapy is discussed in Chapter 42.
Birth weight–specific survival statistics and percentage of survival without severe intraventricular hemorrhage, necrotizing enterocolitis, or bronchopulmonary dysplasia are shown in Table 24.6 for a recent 4-year period from 15 centers participating in the National Institute of Child Health and Human Development (NICHD) Neonatal Research Network. This table also displays the intercenter differences in birth weight–adjusted survival; variation is most evident in the lowest birth-weight groups. Differences in the philosophy of care and management policies most likely account for much of the intercenter variability in survival and suggest that, as Hack put it, “the practice of neonatal medicine remains in part an art rather than an exact science.” Network data shown in Table 24.7 demonstrate an increasing trend of survival without an increase in morbidity until the mid-1990s, but a leveling off of those outcomes since that time.
Figure 24.2 displays survival plots by gender for infants 501- to 800-g birth weight cared for at NICHD Neonatal Research Network centers from 1997 to 2000. For each 100-g birth weight interval, females have higher survival rates. Although the majority of deaths occurred within the first 7 days following birth, this graph demonstrates the continued mortality beyond the first month of life.
Surviving preterm infants with birth weights of less than 1,000 g remain patients within NICUs or intermediate care units for an average of 2 to 4 months. The length of hospitalization tends to be inversely related to birth weight and may be prolonged if complications develop. Therefore, although they may account for a minority of the admissions to a NICU, the
majority of infants found on any day within an intensive care nursery may be very low-birth-weight (1,500 g or less) infants at various points in their hospitalization.
majority of infants found on any day within an intensive care nursery may be very low-birth-weight (1,500 g or less) infants at various points in their hospitalization.
TABLE 24.5. ADMISSIONS TO THE NEWBORN SPECIAL CARE UNIT, YALE–NEW HAVEN CHILDREN’S HOSPITAL, 1997 TO 2002 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
NEWBORN INTENSIVE CARE UNIT STAFF
The size and composition of the medical staff varies according to the size of the NICU; the type of perinatal and neonatal services offered at the hospital (see Tables 24.3 and 24.4); whether the NICU is part of a university medical center, a large community hospital, or a moderate-sized community hospital; and the role that the NICU plays within the regional perinatal system. Most NICUs are directed by full-time physicians who are board-certified pediatricians with subspecialty training and usually certification in perinatal–neonatal medicine.
The size of the NICU nursing staff, particularly the number of nurses assigned per shift, is also a function of the size of the NICU, the level of neonatal care provided, and the case mix. Most NICUs employ only registered nurses. Nurse-to-patient ratios of 1:1 for the sickest infants, 1:2 for intermediate-care patients, and 1:4 for healthier infants who require little extra care have often been used to determine the number of nurses needed per shift. However, patient classification scoring systems that more accurately reflect the actual number of nursing care hours needed by the patients each shift have become common.
Expanded nursing roles are common in the NICU. Neonatal nurse transport teams have been trained at many centers. Using management protocols, they have assumed the responsibility of performing most neonatal transfers.
In addition to medical and nursing staffs, respiratory therapists and social workers play essential roles in the NICU. Because respiratory distress is one of the most common medical problems of NICU patients, respiratory therapists are often assigned to the NICU around the clock. The respiratory therapist ensures that all respiratory equipment is functioning, assists in giving chest physiotherapy, and assists in monitoring the response to various respiratory treatments, such as bronchodilator therapy in infants with bronchopulmonary dysplasia. The respiratory therapist may also perform pulmonary function tests on intubated NICU patients, obtaining data about the infant’s need for continued ventilatory assistance or response to medical therapies. It is common for a respiratory therapist to participate in a neonatal transport. Furthermore, respiratory therapists have become part of the DR resuscitation team since mechanical ventilation or nasal CPAP has been increasingly initiated in the delivery room with extremely low-gestational-age neonates.
Having an infant admitted to a NICU, even for short-term observation, produces stress and anxiety in the parents. For parents whose infants are very small or very sick or have multiple problems, such stress is often overwhelming. Social workers assigned to NICUs work with parents during this emotionally and psychologically draining time. They ensure that the parents understand the information being told to them by the medical team so that they can play an active role in selecting management options. If necessary, the social worker helps the parents begin the grieving process. Often, the social worker continues to counsel parents long after an infant’s discharge or death.
NEONATAL TRANSPORT
Although the best transport isolette is the uterus, maternal transfer of a woman who develops a risk factor during labor (see Table 24.2) is not always possible. In addition, because many neonatal problems (see Table 24.2) are not predicted before delivery, regional neonatal transport systems have been developed. Maternal and neonatal transfers should be performed as soon as possible after a potential problem appears likely. If the medical and nursing staffs at referring hospitals can identify and stabilize high-risk neonates quickly while awaiting the transfer team, the birth weight–adjusted mortality of outborn infants will be similar to that of inborn infants.
Transport back to the referring hospital once an infant no longer requires the special services available at the NICU is
an essential component of a regional perinatal system. Back-transfer helps to ensure the availability and efficient use of NICU beds for the care of critically ill neonates. Therefore, parents should be informed about this policy during discussions after maternal and neonatal transfer.
an essential component of a regional perinatal system. Back-transfer helps to ensure the availability and efficient use of NICU beds for the care of critically ill neonates. Therefore, parents should be informed about this policy during discussions after maternal and neonatal transfer.
TABLE 24.6. ADMISSIONS BY BIRTH WEIGHT, NEWBORN SPECIAL CARE UNIT, YALE-NEW HAVEN CHILDREN’S HOSPITAL, 1997 TO 2002 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Parents
The parents of a neonate admitted to a NICU must be encouraged to visit their infant regularly. Unlimited visiting privileges for parents are the rule in most NICUs. Provisions are usually made for visiting by grandparents, siblings, other family members, and friends. The NICU staff should explain to the parents the reason for admission, initial management plan, expected hospital course with the more common difficulties, and standard NICU routines. The NICU staff should be prepared to repeat and augment this information so that each infant’s parents understand it. Before an infant’s discharge home, especially after a prolonged hospitalization, parents should be encouraged to become actively involved in daily care, such as feeding, diaper changing, and bathing. If the infant will continue to receive medications after discharge, the parents must also learn to measure the dose and administer it. Finally, although the medical staff must direct medical care, parental input and guidance should be sought and considered when medical care becomes extraordinary and possibly futile.
TABLE 24.7. SURVIVAL AND MORBIDITY STATISTICS 1997–2000, NATIONAL INSTITUTE OF CHILD HEALTH AND HUMAN DEVELOPMENT, NEONATAL RESEARCH NETWORKA | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
COST-EFFECTIVENESS OF NEWBORN INTENSIVE CARE UNIT CARE
In the United States and other developed countries, continued advances in neonatal–perinatal medicine have improved markedly the chance of survival and the quality of outcome for very low-birth-weight infants. As shown in Fig. 24.1 and Tables 24.7 and 24.8 approximately 50% of infants with birth weights of 501 to 750 g now survive. These infants, however, especially those with birth weights below 600 g, are at high risk for significant morbidities during their initial neonatal hospitalization, for significant long-term neurodevelopmental sequelae, and for continued health problems requiring ongoing care and often rehospitalization. Because hospital charges for the initial hospitalization may exceed $2,000 per day, the smallest, sickest infants commonly incur initial hospital charges well in excess
of $150,000. In addition, many incur significant posthospitalization costs. Therefore, the cost-effectiveness of NICU care for infants with birth weights of less than 600 g or less than 24 weeks’ gestation has been questioned.
of $150,000. In addition, many incur significant posthospitalization costs. Therefore, the cost-effectiveness of NICU care for infants with birth weights of less than 600 g or less than 24 weeks’ gestation has been questioned.
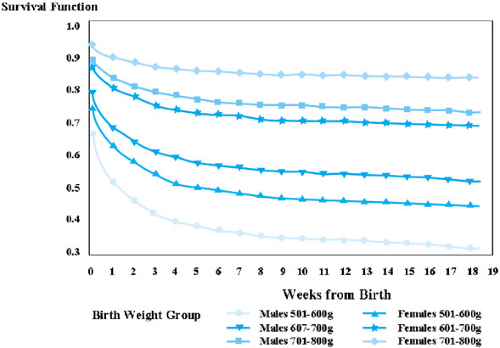 FIGURE 24.2. Survival plots by gender for infants with birth weights of 501 to 800 g at National Institute of Child Health and Human Development Neonatal Research Network Centers, 1997 to 2000. |
Neonatal intensive care is costly not only to the individual family, but also to society. These costs increase with decreasing birth weight and gestational age. However, any attempt to limit neonatal intensive care to those extremely low-birth-weight infants least likely to benefit raises important ethical questions. In addition, neonatologists are usually unable to determine at birth which extremely low-birth-weight preterm infant will survive intact and which will survive with significant health or neurodevelopmental problems. Thus, as survival rates have steadily improved, the absolute number of handicapped survivors has increased with the number of normal survivors. Therefore, neonatologists must include parents in any discussion about whether to continue the extreme measures being provided to their extremely low-birth-weight preterm infants.
NEWBORN RESUSCITATION
Birth is a transition from the intrauterine to the extrauterine environment. It encompasses a series of complex events through which every infant must pass to achieve successfully an independent existence. Such adaptation demands major physiologic changes in several organ systems as well as a reorganization of overall metabolic processes. For example, in utero the human fetus is totally dependent on the mother for respiratory gas exchange, nutrient supply, waste product removal, and thermoregulation. After delivery, the neonate’s lungs must replace the placenta as the site of respiratory gas exchange; stored glycogen and absorption of nutrients by the gastrointestinal tract provide for metabolic homeostasis and growth; the task of waste elimination is taken over by the gastrointestinal tract and kidneys, with the latter also responsible for the maintenance of water and electrolyte balance; and the neonate must be prepared to supply energy to maintain body temperature. In most newborn infants (approximately 85% to 90%), these changes proceed smoothly, and the infants require little or no assistance after delivery. However, a few require help and close observation until they complete the transition successfully, and the occasional infant fails completely to adapt.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree