Chapter 672 The Neck
672.1 Torticollis
Torticollis is a symptom rather than a diagnosis, and describes the clinical findings of tilting of the head to the right or left side in combination with rotation of the head to the opposite side. Congenital muscular torticollis (CMT) is the most common etiology, but a variety of other conditions result in torticollis, and a detailed workup is often required to rule out other diagnoses in patients who lack the characteristic features of CMT (approximately 20%) (Fig. 672-1). The differential diagnosis includes trauma (clavicle fracture or brachial plexopathy), tumors or malformations of the central nervous system, ocular disorders, congenital bony abnormalities (Klippel-Feil syndrome), inflammatory conditions, and other diagnoses such as atlantoaxial rotatory displacement or Sandifer syndrome (Table 672-1).
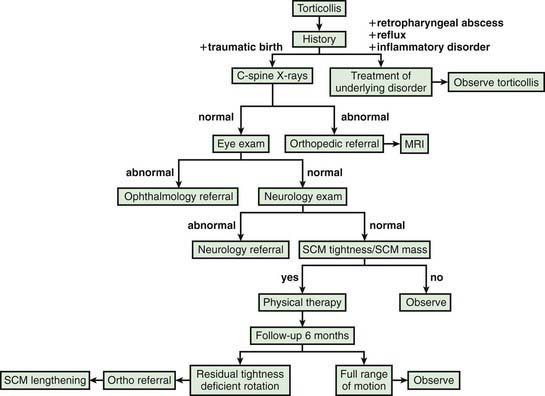
Figure 672-1 Algorithm for evaluation of muscular torticollis. SCM, sternocleidomastoid muscle.
(From Do TT: Congenital muscular torticollis: current concepts and review of treatment, Curr Opin Pediatr 18:26–29, 2006.)
Table 672-1 DIFFERENTIAL DIAGNOSIS OF TORTICOLLIS
CONGENITAL
ACQUIRED
INFLAMMATION
NEUROLOGIC
OTHER
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


