Fig. 1
“Waddell’s triad” (Courtesy of Dan Zlotolow, MD)
The American College of Surgeons has established criteria for pediatric trauma centers , very similar to those for adult trauma centers. The key guidelines are rapid transport and treatment by a dedicated multidisciplinary trauma team, headed by a pediatric general surgeon, and including a variety of other pediatric surgical specialists. Advanced imaging, such as CT scanning, and an operating room should also be available at all times. The basic premise underlying the concept of the trauma center is that of “the golden hour” (Cowley 1976): that initiation of definitive treatment within the first hour after injury is critical in improving survival after polytrauma. Numerous papers have supported the premise that survival rates and outcomes for severely injured and younger children are improved at a pediatric trauma center compared to a community hospital (Smith et al. 1990; Nakayama et al. 1992; Hall et al. 1996; Potoka et al. 2000; Davis et al. 2005; Odetola et al. 2005; Densmore et al. 2006; MacKenzie et al. 2006; Stylianos et al. 2006; Amini et al. 2011). However, such centers are costly and difficult to establish and maintain, and there are many regions without one. Therefore, many pediatric trauma patients are stabilized at other hospitals before transfer to a pediatric trauma center or are treated definitively at an adult trauma center. One European cohort study comparing 2,961 pediatric polytrauma patients to 21,435 adults found that the “golden hour” for pediatric patients often expires in the field or during transfer between hospitals (Wyen et al. 2010).
The use of a general trauma center for pediatric trauma care may be a necessary and acceptable alternative if it is not feasible to bring children directly to a pediatric trauma center (Knudson et al. 1992; Sanchez et al. 2001). Delayed transfer and improved transfer coordination may also optimize patient outcomes (Larson et al. 2004; Sabharwal et al. 2007; Soundappan et al. 2007).
Common Mechanisms of Injury
Child Abuse
Child abuse is a societal problem that crosses all socioeconomic and ethnic groups and is the most common cause of traumatic death in infants and toddlers. In 2011, there were 3.4 million reports of child abuse, involving 6.2 million children. Sixty-one percent of the reports were investigated, of which 18.5 % were substantiated, for a victimization rate of about 9.1 per 1,000 children. There were 1,570 child abuse fatalities in 2011 (United States Administration for Children, Youth, and Families, Child Welfare Information Gateway (U.S.) 2011). Non-accidental trauma has higher mortality and morbidity than accidental trauma (Roaten et al. 2006). This diagnosis must be suspected in all cases of multiple injuries in children younger than 2 years old if there is no obvious and/or witnessed plausible explanation of the injuries. Abuse should be considered a possible cause of injury in all young children with one or more long-bone fractures in association with head injury, or any other manifestations of physical abuse, such as burns. All long-bone fractures in non-ambulatory children should be considered suspicious until proven otherwise. Pediatrician confidence in identifying these injuries remains low (Trowbridge et al. 2005). Although the metaphyseal corner fracture (sometimes called a classic metaphyseal lesion, or CML) is the most highly specific fracture for child abuse, it is relatively rare. The most common extremity fracture secondary to abuse is a single transverse fracture of the femur or humerus (King et al. 1988). There is no fracture that is pathognomonic of abuse; child abuse is a clinical diagnosis made on the basis of the patient’s entire clinical and social picture. Orthopedic surgeons have difficulty distinguishing accidental from non-accidental trauma on the basis of X-ray evaluation alone (Lane and Dubowitz 2007). Although rib fractures occur in only about 5 % of children with multiple injuries from trauma of other causes, they are more common in child abuse (Garcia et al. 1990; Peclet et al. 1990). Whereas blunt compressive trauma to the thorax from other causes may result in lateral rib fractures, the rib fractures seen in child abuse are often posterolateral and adjacent to the transverse processes of the thoracic spine, in three or four sequential ribs on the child’s left side (Kocher and Kasser 2000; Barsness et al. 2003; Williams and Connolly 2004). As a result, posterior rib fractures are very characteristic of child abuse.
A skeletal survey is routinely performed in suspected cases of abuse. Some authors have recommended a bone scan in conjunction with the skeletal survey (Mandelstam et al. 2003), although this recommendation is controversial since the addition of a bone scan requires sedation, elevates radiation exposure, and increases cost (King et al. 1988; American Academy of Pediatrics 2000). Increasingly, a follow-up skeletal survey, performed several weeks after the index procedure, is being recommended (Harlan et al. 2009; Harper et al. 2013).
Falls
Falls are a common primary mechanism of multiple injuries in children (Greenberg 1978; Rozycki and Maull 1991; Buckley et al. 1994; Lallier et al. 1999; Wang et al. 2001). According to a CDC report published in 2008, falls were the leading cause of injury in children, accounting for 2.8 million emergency department visits (Borse and Sleet 2009). Falls occur more often in younger children, causing 50 % of nonfatal injuries in children under the age of 1 year (Borse and Sleet 2009). Fractures from falls usually result from direct impact, whereas internal injuries are the result of deceleration forces present at the time of landing. Many factors, including body position at impact and composition of the landing surface, affect injury severity after a fall (Greenberg 1978). Injuries associated with falls from heights include head injuries in 39 % of children (Lallier et al. 1999), orthopedic injuries in 34–65 % (Lallier et al. 1999; Pitone and Attia 2006), and mortality in 5 % (Demetriades et al. 2003).
Motor Vehicles
Accidents involving motor vehicles account for many multiple system injuries in school-age children and preadolescents. In 2009, 21,000 children aged 14 years and younger were injured, and 318 were killed after being struck by motor vehicles in the United States, an approximately 50 % decrease since 2000 (United States National Highway Traffic Safety Administration 2009). For children riding in cars, there were 179,000 injuries and 1,314 deaths in this age group in 2009 (United States National Highway Traffic Safety Administration 2009). The CDC reported that between 2000 and 2006, transportation-related injuries accounted for 66 % of all accidental deaths in children 0–19 years of age, corresponding to a death rate of 9.8 per 100,000 (Borse and Sleet 2009).
More than half of the children killed as passengers were unrestrained at the time of the accident (United States National Highway Traffic Safety Administration 2009). Child safety seats are effective when used properly: they reduce the risk of fatal injury by 71 % for infants and 54 % for toddlers (United States National Highway Traffic Safety Administration 2009). An unrestrained child is three times more likely than a restrained child to suffer an incapacitating injury in a rollover accident and eight times more likely in a side-impact accident (United States National Highway Traffic Safety Administration 2010b).
Noncompliance with car seat use contributes significantly to morbidity and mortality following MVAs. One trauma center reported that 80 % of children treated there following MVAs were unrestrained at the time of the accident (Thompson et al. 2003). Vaca et al. (2002) noted that many parents of young children were unaware of basic safety information regarding child car seats and airbags and that there are state laws mandating the proper use of child seat restraints. Severe injuries are higher for children in the front seat (Brown et al. 2006). A study of pediatric injuries sustained in MVAs showed higher mortality, longer mean hospital stays, higher mean hospital charges, more hospital admissions, and more fractures, intra-abdominal injuries, and head injuries in unrestrained passengers (Chan et al. 2006).
Even with the appropriate use of car seats, properly restrained children may be severely injured. Zuckerbraun et al. (Zuckerbraun et al. 2004) noted that younger children are more prone to cervical spine injuries. Maintaining proper padding in car seats can potentially decrease the risk of head injury while children are restrained (Kumaresan et al. 2002).
Most states require that infants and toddlers be restrained in car seats when riding in a car, and it is important to note that standard adult shoulder and lap belts do not adequately restrain children who are too big for car seats and too small for the standard restraints. Age- and size-appropriate car seats and restraints are essential for child occupant safety. The current recommendation from the National Highway Traffic Safety Administration is that children use car seats until the age of 4 and booster seats from 4 to 8 (Administration 2010). In addition, there is increasing public sentiment to require seat belt use on school buses, a policy that has been in place for physically disabled student transport for some time. The safety of automobile travel can be dramatically improved with appropriate parent education regarding child safety seats and airbags and by enforcement of current laws.
Pediatric bicyclists, as well as their adult counterparts, are at risk of injury from motor vehicles. All children (and adults) who ride a bicycle should wear a helmet. Bicycle helmets are the most important and cost-effective factor in preventing bike-related injuries. Helmets confer a 63–88 % reduction in brain injury from a bicycle accident (Gill 2012). One study estimated that universal helmet usage would prevent 56,000 head injuries per year at a cost savings of 1.3 billion dollars (Schulman et al. 2002).
Evaluation and Resuscitation
Initial Assessment
Initial resuscitation of a multiply injured child follows the Advanced Trauma Life Support (ATLS) or Pediatric Advanced Life Support (PALS) protocols and is essentially the same as that of an adult patient (Armstrong 1992; Cramer 1995; Maksoud et al. 1995). Regardless of the mechanism causing the multiple injuries, the initial medical management focuses on the life-threatening, non-orthopedic injuries to stabilize the child’s condition (Maksoud et al. 1995). The primary survey is comprised of the “ABCs” – airway, breathing, circulation, disability (neurologic), and exposure – and screening radiographs (cervical spine, chest, and pelvis). Immediate establishment of an adequate airway is the first priority in the care of the pediatric polytrauma patient. Special care should be taken to protect the cervical spine, particularly during transport of the patient. In children less than six years of age, the head is disproportionately large compared to the rest of the body. Because of this, children in this age group require a special transport board with a cutout for the occipital area. This prevents potentially dangerous flexion of the cervical spine (Herzenberg et al. 1989) (Fig. 2a–c).
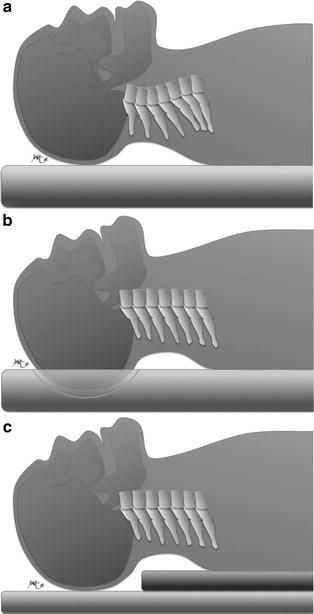
Fig. 2
Transport board use in children. (a) Adult backboard with no cutout flexes the c-spine in a pediatric patient. (b) Pediatric backboard with cutout allows slight extension of the c-spine. (c) An alternate to a pediatric backboard is to add an additional board from the shoulders distally to allow slight extension of the c-spine (Courtesy of Dan Zlotolow, MD)
Fluid Replacement
Since hypovolemia is the most common cause of shock in pediatric trauma patients, early and adequate fluid resuscitation is critical (Schafermeyer 1993). Hypovolemia can result in the “triad of death,” consisting of acidosis, hypothermia, and coagulopathy (Wetzel and Burns 2002). After the airway and breathing have been stabilized, circulation is assessed, and appropriate fluid replacement is begun, utilizing crystalloid solution administered intravenously. If intravenous access is difficult, the intraosseous administration route may be used. Guy et al. (1993) reported no complications in 15 children between the ages of 3 months and 10 years who underwent tibial intraosseous infusion of colloid solution, crystalloid solution, and blood. A rabbit tibia model has also shown that intraosseous infusion is well tolerated (Bielski et al. 1993).
The goal of fluid resuscitation is to maintain the child’s blood pressure at a level adequate for organ perfusion, while avoiding overhydration that can lead to increased intracranial pressure, internal fluid shifts, or pulmonary edema. A urinary catheter is essential to monitor urine output and gauge organ perfusion, and a central venous catheter may also be necessary.
Secondary Assessment
The secondary assessment begins with a full history and physical exam. Because most polytrauma in children is the result of blunt trauma, a careful abdominal exam is essential, as injury to the liver, spleen, pancreas, and kidneys is common. Abdominal ecchymosis is a marker of visceral or spinal injury (Sivit et al. 1991; Campbell et al. 2003). The entire spine should be examined, beginning with the removal of the cervical collar for palpation of the cervical spine for tenderness, crepitus, or step-off. It is necessary for a member of the team to stabilize the head while the collar is off. After replacement of the collar, the patient should be logrolled for assessment of the remainder of the spine and the skin and soft tissue of the back. A rectal exam to assess the sphincter tone is performed.
The extremity exam is also part of the secondary assessment, and all limbs should be evaluated for swelling, deformity, crepitus, and neurovascular status. Splints applied in the field should be removed so that a thorough exam may be made. The skin of an injured limb should be examined carefully for the possibility of an open fracture. If there are open wounds, they should be cleaned and dressed, and tetanus prophylaxis and antibiotics initiated. Splints can be reapplied when the exam is complete.
The pelvis should be carefully assessed, keeping in mind that a pelvic fracture combined with one or more other skeletal injuries can be associated with head and abdominal injuries (Vazquez and Garcia 1993). If instability is noted with compression of the iliac wings, a pelvic binder can be applied. Ideally, the neurologic exam should be performed prior to intubation or administration of any medications, but this is not always possible. Any neurologic deficit should be noted, and if the patient is unconscious, uncooperative, or unable to understand or comply with the examination, that should be noted as well.
It is important to remember that some injuries may be missed on the primary and secondary surveys, particularly in patients with a head injury. A tertiary survey, in which a full history and physical exam is performed again, 24–48 h after the initial assessment, is necessary to aid in the diagnosis of these late-presenting injuries. In one series of 149 pediatric polytrauma patients, 13 injuries were diagnosed an average of 15 days following injury, including five fractures (one involving the spine), four abdominal injuries, two aneurysms, one head injury, and one facial fracture (Letts et al. 2002). It is helpful to alert families of the possibility of such delayed diagnoses, so that they are not surprised in the event of one and so that they can inform the medical team of any emerging symptoms.
Trauma Rating Systems
Trauma rating systems perform two functions: to assist in the triage of injured patients and as prognostic indicators. Usually, the trauma rating is performed between the primary and secondary surveys. Many different trauma rating systems have been developed and are in use, each with its own strengths and weaknesses. There are a variety that have been validated for the pediatric population (Tepas et al. 1988; Champion et al. 1989; Eichelberger et al. 1989; Aprahamian et al. 1990; Pollack et al. 1996; Potoka et al. 2001; Schall et al. 2002; Slater et al. 2003; Schluter et al. 2010; Borgman et al. 2011), but the most commonly utilized are the Glasgow Coma Scale (GCS), the Injury Severity Score (ISS), and the Pediatric Trauma Score (PTS).
The Glasgow Coma Scale (GCS) is commonly used for the assessment of traumatic brain injury. It evaluates eye opening (1–4 points), motor function (1–6 points), and verbal function (1–5 points) on a total scale of 3–15 points (Teasdale and Jennett 1974). In verbal children, the GCS is a useful guide for predicting early mortality and later disability. A GCS score of less than 8 points indicates a significantly worse chance of survival for these children than for those with a GCS of more than 8. The GCS score can evolve with the underlying neurologic injury, so it should be noted on admission and again 1 h after the child arrives at the hospital. Moreover, the evolving GCS can have prognostic significance: the 72-h GCS motor response score has been noted to be very predictive of later permanent disability as a sequel to the head injury (Young et al. 1981; Michaud et al. 1992; Hannan et al. 2000).
Both the ISS and the PTS are valid and reproducible and can be used in varied pediatric settings. The choice of one or the other varies by trauma center, but each allows an objective means to assess mortality risk at the time of initial treatment, as well as allowing some degree of prediction of future disability (Ott et al. 2000; Yian et al. 2000; Sullivan et al. 2003). The ISS is based on the Abbreviated Injury Scale (AIS), which assigns a grade of moderate, severe, serious, critical, and fatal for each of the five major body systems. To determine the ISS, one computes the sum of the squares of the highest AIS grade in each of the three most severely injured areas. Twenty-five is the highest score for any individual area, and 75 is therefore the highest possible ISS score. However, it is an ordinal, not a linear scale (i.e., a score of 40 is not twice as bad as a score of 20). It has been found to be a valid predictor of mortality, length of hospital stay, and cost of care (Brazelton and Gozain 2012).
The PTS assigns each of six components a score of +2 (minimal or no injury), +1 (minor or potentially major injury), or −1 (major or potentially life-threatening injury). The potential score thus ranges from −6 to +12. The PTS has good predictive value for injury severity, mortality, and the need for transport to a pediatric trauma center; however, it is a poor predictor of internal injury in children with abdominal blunt trauma (Saladino et al. 1991).
Imaging
Radiographs
Primary screening radiographs classically consist of a cross-table lateral cervical spine, anteroposterior chest, and anteroposterior pelvis (Rees et al. 2001; Dormans 2002). Cervical spine clearance may require multiple studies. Though the lateral cervical radiograph will detect an injury, if present, in 80 % of cases (Lee and Fleisher 2012), some centers perform a CT scan of the cervical spine instead, particularly in cases of children with neck pain, with traumatic brain injury (TBI), or who have been drinking alcohol (Sanchez et al. 2005). Magnetic resonance imaging (MRI) is useful for cervical spine clearance in those who have persistent neck pain or tenderness despite normal plain films and CT and should be considered in patients who are obtunded (Frank et al. 2002).
Computed Tomography
CT scans are commonly used in the evaluation of the multiply injured child. CT of the head can diagnose skull fractures and intracranial hemorrhage, and the study can easily be extended distally to evaluate the cervical spine as well. Potential intra-abdominal injury in pediatric patients is also commonly diagnosed by CT scan. CT scans and serial hematocrit levels are also followed to determine whether or not visceral injuries, such as hepatic and splenic lacerations, need to be treated operatively (Hoffmann et al. 1992; Roche et al. 1992; Campbell et al. 2003).
A CT scan of the abdomen can also be extended to include the pelvis. There is evidence that CT is more sensitive than plain radiography in screening for pelvic fractures. In one study, a screening pelvic radiograph demonstrated only 54 % of pelvic fractures identified on CT scan (Guillamondegui et al. 2003). Pelvic CT scan also has the added benefits of providing more detail about fracture pattern than plain X-rays, thus aiding in preoperative planning.
Intravenous Pyelography (IVP)
Anterior pelvic fractures are often associated with urologic injury. Although CT, MRI, and U/S can be useful in evaluating the kidneys, IVP still has a role in imaging the bladder and urethra (Onuora et al. 1993). Urethral injuries in particular are difficult to fully delineate preoperatively, regardless of imaging modality (Andrich et al. 2003).
Magnetic Resonance Imaging
MRI is most commonly used to evaluate traumatic brain and spinal cord injuries. Because the spinal cord is less elastic than the growing spine, children can sustain a spinal cord injury without an evident spine fracture (Aufdermaur 1974; Evans and Bethem 1989; Bosch et al. 2002). This is referred to as spinal cord injury without radiographic abnormality (SCIWORA) syndrome. MRI is particularly valuable in demonstrating the site and extent of spinal cord injury in SCIWORA and in defining the level of injury to the disks or vertebral apophyses, which may not be obvious on conventional radiographs.
Ultrasound
Serial ultrasound evaluations can be used to monitor the liver, spleen, pancreas, and kidney injury in children with multiple injuries (Buess et al. 1992; Hoffmann et al. 1992; Roche et al. 1992), as U/S is an accurate means of detecting hemopericardium and intraperitoneal fluid following injury. The protocol most typically used is called “FAST” (focused assessment with sonography for trauma). A FAST scan rapidly evaluates four areas: the right upper abdominal quadrant, the left upper abdominal quadrant, the subxiphoid area, and the pelvis. Assessment of the role of FAST in the management of pediatric trauma patients is ongoing (Coley et al. 2000; Holmes et al. 2001; Stafford et al. 2002; Eppich and Zonfrillo 2007; Holmes et al. 2007); therefore, CT is still more commonly used for assessment and monitoring of visceral injury in children sustaining multiple injuries. Comparisons of CT and ultrasonography have demonstrated the superiority of CT for diagnosing visceral injury in children with polytrauma (Richardson et al. 1997; Mutabagani et al. 1999; Coley et al. 2000; Suthers et al. 2004), but there is evidence that hemodynamically unstable children with a positive FAST should be taken for laparotomy rather than for CT scanning (Levy and Bachur 2008).
Non-orthopedic Injuries
Head Injury
Traumatic brain injury (TBI) is extremely common in the multiply injured child (Letts et al. 2002; Schalamon et al. 2003). Though severity of the head injury is the principle determinant of the overall morbidity and mortality in the setting of pediatric polytrauma (Jakob et al. 2010), children often make a significant recovery from even severe head trauma. The two factors that have been linked to poorer long-term outcomes in cases of TBI are low oxygen saturation levels at presentation and persistently decreased GCS score at 72 h. However, most children who sustain a significant TBI do exhibit some residual cognitive impairment and behavior problems (Greenspan and MacKenzie 1994; Swift et al. 2003; Hanten et al. 2004). Because substantial neurologic recovery is expected, the management of musculoskeletal injuries in these children should be based on the assumption that restoration of cognitive and motor function will ensue.
It is typically not necessary to wait until a comatose child is awake to undertake fracture fixation, as waiting may lead to fracture malunion, since fractures tend to heal very rapidly in patients with TBI (Zhao, Zhao et al. 2007). Moreover, motion at fracture sites can lead to increased intracranial pressure, so definitive fracture treatment can help control intracranial pressure. If definitive stabilization is not possible, interim stabilization with splints, traction, or external fixation may be used.
Head trauma can also lead to several other musculoskeletal system sequelae, including increased spasticity, contracture, and heterotopic bone formation. Spasticity tends to occur quite early after TBI. In the clinical scenario of TBI and concomitant fracture, the pull of spastic muscles can lead to fracture shortening and angulation. Operative fixation may be necessary for acceptable reduction in these cases (Tolo 1983, 2000). Persistent spasticity leads to joint contracture. Contracture can develop very quickly, so it is imperative to institute early preventative stretching and splinting. Surgical release is sometimes necessary for persistent contractures.
Heterotopic bone formation is common in the extremities of patients with TBI and persistent coma, particularly around the hip and elbow (Mital et al. 1987; Kluger et al. 2000). Surgical incisions may exacerbate the problem (Keret et al. 1990). Heterotopic bone that does not interfere with range of motion or function typically is observed, whereas symptomatic heterotopic ossification may be excised. The timing of excision is controversial, as is the use of nonsteroidal medications or salicylates for initial prophylaxis. After surgical excision, Mital et al. (1987) reported success in preventing recurrence of heterotopic bone formation by the use of salicylates at a dosage of 40 mg/kg/day in divided doses for 6 weeks postoperatively. Though low-dose radiation therapy has also been successfully used for prevention of post-excision recurrence, there are now two case reports in the literature of postradiation sarcoma from doses as low as 700 cGy (Farris et al. 2012; Mourad et al. 2012).
Abdominal Injury
Abdominal injuries are relatively common in pediatric polytrauma patients, with an incidence of 8–27 % (Dereeper et al. 1998; Letts et al. 2002). Physical exam findings indicative of such injuries are abdominal distension, bruising, and tenderness. Initial evaluation is usually performed by CT scan and less commonly by peritoneal lavage, ultrasound, or laparoscopy. The classic “lap belt triad,” consisting of abdominal bruising in association with the spinal cord and abdominal viscera injury, is rarely seen, and therefore, all children who were injured while wearing a lap belt should be examined carefully for abdominal injury even in the absence of visible ecchymosis (Tso et al. 1993; Campbell et al. 2003). The presence of pelvic fractures also correlates strongly with both intra-abdominal and genitourinary injuries (Bond et al. 1991). Hepatic and splenic injuries are the most common, but about 22 % of cases of pediatric pancreatitis are traumatic (Benifla and Weizman 2003).
In children, most visceral lacerations are treated nonoperatively. The hematocrit and abdominal exams are followed closely, and serial CT or ultrasound exams are often utilized (Canarelli et al. 1991; Coburn et al. 1995; Uranus and Pfeifer 2001; Cloutier et al. 2004; Cochran et al. 2004; Leinwand et al. 2004; Tataria et al. 2007). It is usually possible to perform definitive operative fixation of fractures in a child who is under observation for an abdominal viscera injury.
Genitourinary Injury
Though rare in isolation, genitourinary injuries occur in 9–24 % of children with pelvic fractures (Torode and Zieg 1985; Silber et al. 2001; Letts et al. 2002). In boys, anterior pelvic ring injuries are typically associated with bulbourethral injuries, though other areas of the bladder and urethra may also be involved (Onuora et al. 1993; Batislam et al. 1997). Despite such injuries being less common in girls, they are typically quite serious when they do occur, with damage to the vagina and rectum. Sequelae of these injuries include strictures, incontinence, and difficulty with childbirth (Podesta and Jordan 2001; Rourke et al. 2003). There is an increased rate of cesarean section in young women who have had a pelvic fracture (Copeland et al. 1997), and girls with displaced pelvic fractures, particularly if there has been a permanent change to the shape of the pelvic ring, should be informed that vaginal delivery may be difficult or impossible.
Fat and Pulmonary Embolism
Though hypoxemia can occur in the multiply injured child, the full clinical presentation of fat embolism and acute respiratory distress syndrome is rare (Limbird and Ruderman 1978; Robinson 2001). When a child does present with the symptoms of fat embolism (change in mental status, hypoxemia, axillary petechiae, and the presence of lung infiltrates on chest radiograph), the treatment is similar to that for adults: endotracheal intubation, positive pressure ventilation, and hydration with intravenous fluid. Other interventions that have been used in adults, such as early fracture stabilization, intravenous alcohol, and high-dose corticosteroids, have not been studied in children.
Deep venous thrombosis and pulmonary thromboembolism in children is rare but has been reported (Levy et al. 2004; Azu et al. 2005; Babyn et al. 2005; Truitt et al. 2005; Cyr et al. 2006). Risk factors for deep venous thrombosis and pulmonary thromboembolism in the multiply injured child include age greater than 9, ISS greater than or equal to 25, and/or GCS lower than or equal to 8 and the presence of an indwelling central venous catheter (Champion et al. 1989; Roche et al. 1992). The role of prophylaxis for deep venous thrombosis and pulmonary thromboembolism in pediatric patients is unclear (Rohrer et al. 1996; Truitt et al. 2005; Sandoval et al. 2008; Brandao et al. 2011).
Orthopedic Injuries
Timing of Fixation
Though fractures are common in pediatric trauma patients, they are rarely life threatening. Initial management of fractures thus often consists simply of splinting until the child is deemed systemically stable enough for operative fracture fixation if indicated. “Damage control orthopedics,” in which temporary external fixation is utilized in the period between presentation and definitive fracture fixation, has been well studied and accepted in the adult literature (Scalea et al. 2000; Pape et al. 2002; Taeger et al. 2005; Tuttle et al. 2009). The concept behind damage control orthopedics is that early definitive surgery is a significant stressor that acts as a physiological “second hit” to an already critically ill patient. Delaying the second hit allows for some interim recovery and decreases the incidence of acute respiratory distress syndrome and multisystem organ failure. Damage control orthopedics has not been studied in children. There is one case series of three patients with femur fractures, initially treated with an external fixator and subsequently revised to submuscular plating (Mooney 2012).
Timing of definitive surgery has also not been studied extensively. Loder (1987) reported shorter hospital and intensive care unit stays and a shorter time on ventilator assistance, in 78 children with multiple injuries who underwent operative stabilization of fractures within the first 2 or 3 days after injury. The cohort of patients treated with immediate fracture stabilization also had fewer complications than those who had surgical treatment more than 72 h after injury. Another more recent study (Loder et al. 2001) reported a trend toward a higher rate of complications of immobilization (including pulmonary complications) in fractures treated late (after 72 h), but the difference did not reach statistical significance.
Pelvic Fractures
Pelvic fractures have been reported in up to 7 % of children referred to level 1 regional trauma centers (Smith et al. 2004; Vitale et al. 2005). Most of these fractures are stable, though unstable patterns have been reported in up to 30 % of cases (Blasier et al. 2000). It is important to remember that pelvic fractures are often associated with other injuries. In one study of 166 children with pelvic fractures, there was substantial head trauma in 39 %, chest trauma in 20 %, visceral or abdominal injuries in 19 %, concomitant acetabular fractures in 12 %, and a mortality rate of 3.6 % (Silber et al. 2001). In another series, 62 % of children (8/13) with pelvic fractures had other orthopedic injuries (Spiguel et al. 2006). Anterior pelvic ring fractures frequently cause urethral injuries (Abou-Jaoude et al. 1996; Batislam et al. 1997; Podesta and Jordan 2001; Rourke et al. 2003). Mortality in children with pelvic fractures appears to be caused more often by an associated head injury rather than from abdominal or retroperitoneal bleeding from the pelvic fracture or adjacent viscera, though such hemorrhages can be significant (Musemeche et al. 1987; Demetriades et al. 2003). Non-orthopedic injuries associated with pelvic fractures led to long-term morbidity or mortality in 31 % (11/36) of patients in one review of pediatric pelvic fractures (Garvin et al. 1990).
In cases in which it is necessary to acutely stabilize a fractured pelvis either to control bleeding or facilitate care or transport of the child, a pelvic binder or an external fixator may be used (Reff 1984; Taeger et al. 2005; Jakob et al. 2010). The C-clamp is not typically utilized for the pediatric population, though it has been reported to be safe (Holt and Mencio 2003). In cases in which operative treatment is necessary, rapid healing with a low complication rate is expected (Karunakar et al. 2005).
Open Fractures
In the setting of polytrauma , approximately 10 % of fractures are open (Buckley et al. 1994; Schalamon et al. 2003). Twenty-five to fifty percent of patients with open fractures have associated injuries of the head, chest, abdomen, or other extremities (Schalamon et al. 2003). Open fractures are classified by the system of Gustilo (Gustilo and Anderson 1976; Gustilo et al. 1984), which takes into account the size of the wound, the degree of soft tissue damage and wound contamination, and the presence or absence of an associated vascular injury. A type I wound is less than 1 cm in diameter and has minimal associated soft tissue damage. A type II wound is greater than 1 cm in diameter and has some associated soft tissue damage, but typically will not require skin grafting or flaps. Type III injuries are large wounds with extensive soft tissue damage and contamination and sometimes associated vascular injury as well.
Initial emergency management of open fractures includes application of a dressing, provisional reduction and splinting, and administration of tetanus toxoid and antibiotics. The dose of tetanus toxoid is 0.5 mL intramuscularly to be given if the patient’s immunization status is unknown or if it is more than 5 years since the last dose. A typical antibiotic regimen is a first-generation cephalosporin (cefazolin 100 mg/kg/day divided q 8 h, maximal daily dose 6 g) for all type I and some type II injuries, the addition of an aminoglycoside (gentamicin 5–7.5 mg/kg/day divided q 8 h) for more extensive type II and all type III injuries, and the addition of penicillin (150,000 units/kg/day divided q 6 h, maximum daily dose of 24 million units) for farm injuries, gross contamination, and associated vascular injuries (Lavelle et al. 2008). Antibiotics are usually given for 48 h initially, with an additional course for every surgery. Keep in mind that evidence-based medicine does support the use of a short course of a first-generation cephalosporin, but the data are inadequate to support the other treatment of the limbs outlined above (Hauser et al. 2006). Moreover, the guidelines above were developed prior to the recent increase in prevalence of community-acquired methicillin-resistant Staphylococcus aureus (MRSA). Clindamycin or vancomycin should be added to the regimen if contamination with MRSA is suspected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


