Chapter 670 The Hip
Growth and Development
The hip joint begins to develop at about the 7th week of gestation, when a cleft appears in the mesenchyme of the primitive limb bud. These precartilaginous cells differentiate into a fully formed cartilaginous femoral head and acetabulum by the 11th week of gestation (Chapter 6.1). At birth, the neonatal acetabulum is completely composed of cartilage, with a thin rim of fibrocartilage called the labrum.
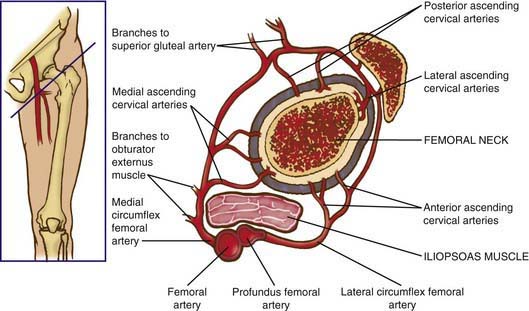
Vascular Supply
The blood supply to the capital femoral epiphysis is complex and changes with growth of the proximal femur. The proximal femur receives its arterial supply from intraosseous (primarily the medial femoral circumflex artery) and extraosseous vessels (Fig. 670-1). The retinacular vessels (extraosseous) lie on the surface of the femoral neck but are intracapsular because they enter the epiphysis from the periphery. This makes the blood supply vulnerable to damage from septic arthritis, trauma, thrombosis, and other vascular insults. Interruption of this tenuous blood supply can lead to avascular necrosis of the femoral head and permanent deformity of the hip.
670.1 Developmental Dysplasia of the Hip
Clinical Findings
The Neonate
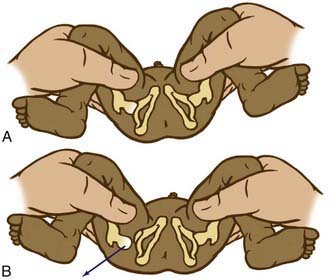
The Barlow provocative maneuver assesses the potential for dislocation of a nondisplaced hip. The examiner adducts the flexed hip and gently pushes the thigh posteriorly in an effort to dislocate the femoral head (Fig. 670-2). In a positive test, the hip is felt to slide out of the acetabulum. As the examiner relaxes the proximal push, the hip can be felt to slip back into the acetabulum.
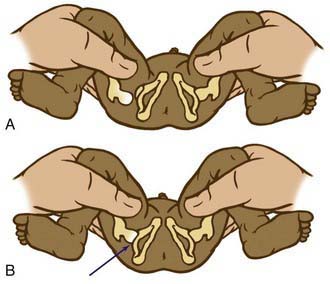
The Ortolani test is the reverse of Barlow test: The examiner attempts to reduce a dislocated hip (Fig. 670-3). The examiner grasps the child’s thigh between the thumb and index finger and, with the 4th and 5th fingers, lifts the greater trochanter while simultaneously abducting the hip. When the test is positive, the femoral head will slip into the socket with a delicate clunk that is palpable but usually not audible. It should be a gentle, nonforced maneuver.
The Infant
As the baby enters the 2nd and 3rd months of life, the soft tissues begin to tighten and the Ortolani and Barlow tests are no longer reliable. In this age group, the examiner must look for other specific physical findings including limited hip abduction, apparent shortening of the thigh, proximal location of the greater trochanter, asymmetry of the gluteal or thigh folds (Fig. 670-4), and pistoning of the hip. Limitation of abduction is the most reliable sign of a dislocated hip in this age group.
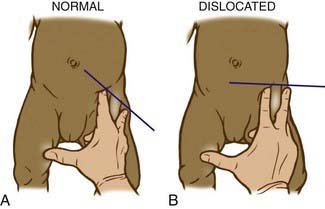
Shortening of the thigh, the Galeazzi sign, is best appreciated by placing both hips in 90 degrees of flexion and comparing the height of the knees, looking for asymmetry (Fig. 670-5). Asymmetry of thigh and gluteal skin folds may be present in 10% of normal infants but suggests DDH. Another helpful test is the Klisic test, in which the examiner places the 3rd finger over the greater trochanter and the index finger of the same hand on the anterior superior iliac spine. In a normal hip, an imaginary line drawn between the two fingers points to the umbilicus. In the dislocated hip, the trochanter is elevated, and the line projects halfway between the umbilicus and the pubis (Fig. 670-6).
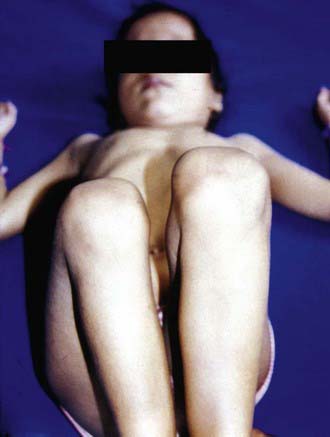
Figure 670-5 Positive Galeazzi sign noted in a case of untreated developmental dysplasia of the hip.
Diagnostic Testing
Ultrasonography
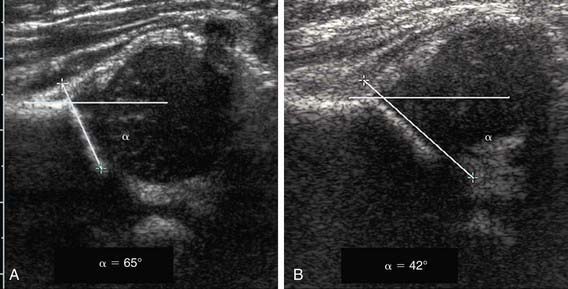
In the Graf technique, the transducer is placed over the greater trochanter, which allows visualization of the ilium, the bony acetabulum, the labrum, and the femoral epiphysis (Fig. 670-7). The angle formed by the line of the ilium and a line tangential to the boney roof of the acetabulum is termed the α angle and represents the depth of the acetabulum. Values >60 degrees are considered normal, and those <60 degrees imply acetabular dysplasia. The β angle is formed by a line drawn tangential to the labrum and the line of the ilium; this represents the cartilaginous roof of the acetabulum. A normal β angle is <55 degrees; as the femoral head subluxates, the β angle increases. Another useful test is to evaluate the position of the center of the head compared to the vertical line of the ilium. If the line of the ilium falls lateral to the center of the head, the epiphysis is considered reduced. If the line falls medial to the center of the head, the epiphysis is undercovered and is either subluxated or dislocated.
Radiography
Radiographs are recommended for an infant once the proximal femoral epiphysis ossifies, usually by 4-6 mo. In infants of this age, the radiographs have proved to be more effective, less costly, and less operator dependent than an ultrasound examination. An anteroposterior (AP) view of the pelvis can be interpreted through several classic lines drawn on it (Fig. 670-8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree