The High-Risk Newborn: Anticipation, Evaluation, Management, and Outcome
Vincent C. Smith
I. HIGH-RISK NEWBORNS
are often associated with certain maternal, placental, or fetal conditions; when one or more are present, nursery staff should be aware and prepared for possible difficulties. The placenta should be saved after delivery in all cases of high-risk delivery, including cases that involve transfer from the birth hospital, since an elusive diagnosis such as toxoplasmosis may be made on the basis of placental pathology. The following factors are associated with high-risk newborns:
Maternal characteristics and associated risk for fetus or neonate
Age at delivery
Over 40 years. Chromosomal abnormalities, macrosomia, intrauterine growth retardation (IUGR), blood loss (abruption or previa).
Under 16 years. IUGR, prematurity, child abuse/neglect (mother herself may be abused).
Personal factors
Poverty. Prematurity, IUGR, infection.
Smoking. Increased perinatal mortality, IUGR.
Drug/alcohol use. IUGR, fetal alcohol syndrome, withdrawal syndrome, sudden infant death syndrome, child abuse/neglect.
Poor diet. Mild IUGR to fetal demise in severe malnutrition.
Trauma (acute, chronic). Abruptio placentae, fetal demise, prematurity.
Medical conditions
Diabetes mellitus. Stillbirth, macrosomia/birth injury, respiratory distress syndrome (RDS), hypoglycemia, congenital anomalies (see Chap. 2).
Thyroid disease. Goiter, hypothyroidism, hyperthyroidism (see Chap. 3).
Renal disease. Stillbirth, IUGR, prematurity.
Urinary tract infection. Prematurity, sepsis.
Heart and/or lung disease. Stillbirth, IUGR, prematurity.
Hypertension (chronic or pregnancy-related). Stillbirth, IUGR, prematurity, asphyxia.
Anemia. Stillbirth, IUGR, hydrops, prematurity, asphyxia.
Isoimmunization (red cell antigens). Stillbirth, hydrops, anemia, jaundice.
Alloimmunization (platelet antigens). Stillbirth, bleeding.
Thrombocytopenia. Stillbirth, bleeding.
Obstetric history
Past history of infant with prematurity, jaundice, RDS, or anomalies. Same with current pregnancy.
Bleeding in early pregnancy. Stillbirth, prematurity.
Hyperthermia. Fetal demise, fetal anomalies.
Bleeding in third trimester. Stillbirth, anemia.
Premature rupture of membranes. Infection/sepsis.
TORCH infections. (see Chap. 48)
Trauma. Fetal demise, prematurity.
Fetal characteristics and associated risk for fetus or neonate
Multiple gestation. IUGR, twin—twin transfusion syndrome, prematurity, birth trauma, asphyxia.
IUGR. Fetal demise, congenital anomalies, asphyxia, hypoglycemia, polycythemia.
Macrosomia. Congenital anomalies, birth trauma, hypoglycemia.
Abnormal fetal position/presentation. Congenital anomalies, birth trauma, hemorrhage.
Abnormality of fetal heart rate or rhythm. Congestive heart failure, heart block, hydrops, asphyxia.
Decreased activity. Fetal demise, asphyxia.
Polyhydramnios. Anencephaly, other central nervous system (CNS) disorders, neuromuscular disorders, problems with swallowing (e.g., agnathia, any mass in the mouth, esophageal atresia), chylothorax, diaphragmatic hernia, omphalocele, gastroschisis, trisomy, tumors, hydrops, isoimmunization, anemia, cardiac failure, intrauterine infection, inability to concentrate urine, large for gestational age, maternal diabetes.
Oligohydramnios. Fetal demise, placental insufficiency, IUGR, renal agenesis, pulmonary hypoplasia, deformations, intrapartum distress, postterm delivery.
Conditions of labor and delivery and associated risk for fetus or neonate
Preterm delivery. RDS, other issues of preterm birth (see Chap. 13).
Postterm delivery (occurring more than 2 weeks after term) (see IV). Stillbirth, asphyxia, meconium aspiration.
Maternal fever. Infection/sepsis.
Maternal hypotension. Stillbirth, asphyxia.
Rapid labor. Birth trauma, intracranial hemorrhage (ICH), retained fetal lung fluid/transient tachypnea.
Prolonged labor. Stillbirth, asphyxia, birth trauma.
Abnormal presentation. Birth trauma, asphyxia.
Uterine tetany. Asphyxia.
Meconium-stained amniotic fluid. Stillbirth, asphyxia, meconium aspiration syndrome, persistent pulmonary hypertension.
Prolapsed cord. Stillbirth, asphyxia.
Cesarean section. RDS, retained fetal lung fluid/transient tachypnea, blood loss.
Obstetric analgesia and anesthesia. Respiratory depression, hypotension, hypothermia.
Placental anomalies
Small placenta. IUGR.
Large placenta. Hydrops, maternal diabetes, large infant.
Torn placenta and/or umbilical vessels. Blood loss.
Abnormal attachment of vessels to placenta. Blood loss.
Immediately evident neonatal conditions and associated risk for fetus or neonate
Prematurity. RDS, other sequelae of prematurity.
Low 5-minute Apgar score. Prolonged transition (especially respiratory).
Low 15-minute Apgar score. Neurologic damage.
Pallor or shock. Blood loss.
Foul smell of amniotic fluid or membranes. Infection.
Small for gestational age (SGA). (see V.)
Postmaturity syndrome. (see IV.D.)
II. GESTATIONAL AGE (GA) AND BIRTH WEIGHT CLASSIFICATION.
Neonates should be classified by GA, if at all possible, as this is generally more physiologically important than birth weight.
GA classification.
Assessment based on obstetric information is covered in Chapter 1. Note that GA estimates by first-trimester ultrasonography are accurate within 4 days.
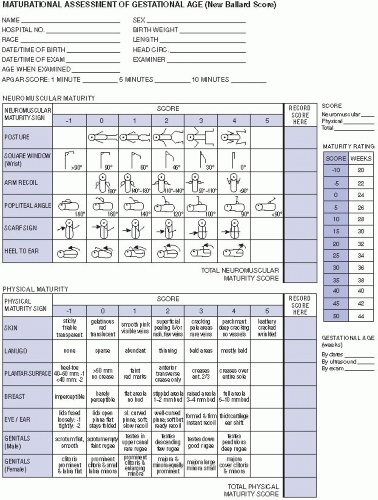
To confirm or supplement obstetric dating, the modified Dubowitz (Ballard) examination for newborns (see Fig. 7.1) may be useful in GA estimation. There are limitations to this method, especially with use of the neuromuscular component in sick newborns.
Infant classification by gestational (postmenstrual) age
Preterm. Less than 37 completed weeks (259 days).
Late preterm. A subgroup of infants born at 34 through 36 weeks GA (238-258 days).
Term. Thirty-seven to 41 6/7 weeks (260-294 days).
Postterm. Forty-two weeks (295 days) or more.
Birth weight classification. Although there is no universal agreement, the commonly accepted definitions are as follows:
Normal birth weight (NBW). From 2,500 to 4,000 g.
Low birth weight (LBW). Less than 2,500 g. Note that, while most LBW infants are preterm, some are term but SGA. LBW infants can be further subclassified as follows:
III. PRETERM BIRTH.
As noted above, a preterm neonate is one whose birth occurs before the end of the 37th week (258th day; i.e., 36 6/7 weeks) following onset of the last menstrual period.
Incidence. Approximately 12.7% of all births in the United States are preterm. The distribution of this group is gradually shifting to a relatively older gestational age because of a 25% increase in late preterm infants (34 to 36 weeks) since 1990 to current rate of 9.1%.
Etiology is unknown in most cases. Preterm and/or LBW delivery is associated with the following conditions:
Low socioeconomic status (SES), whether measured by family income, educational level, geographic area/ZIP code, social class, and/or occupation.
Non-Hispanic black women are more than three times as likely to deliver an extremely preterm infant (<28 weeks of gestation) (1.9%) compared with non-Hispanic white and Hispanic women (0.6%). This disparity in very short gestation delivery by race/ethnicity contributes to the substantial black—white gap in infant mortality. Disparities persist even when SES is taken into account.
Women younger than 16 or older than 35 are more likely to deliver preterm or LBW infants; the association with age is more significant in whites than in African Americans.
Maternal activity requiring long periods of standing or substantial amounts of physical stress may be associated with IUGR and prematurity.
Acute or chronic maternal illness is associated with early delivery, whether spontaneous or, not infrequently, induced.
Multiple-gestation births frequently deliver preterm (60% of twins and 94% of triplets in the United States in 2005). In such births, higher rate of neonatal mortality is primarily due to prematurity.
Prior poor birth outcome is the single strongest predictor of poor birth outcome. A preterm first birth is the best predictor of a second preterm birth.
Obstetric factors such as uterine malformations, uterine trauma, placenta previa, abruptio placentae, hypertensive disorders, preterm cervical shortening, previous cervical surgery, premature rupture of membranes, and chorioamnionitis also contribute to prematurity.
Fetal conditions such as nonreassuring testing of fetal well-being (see Chap. 1), IUGR, or severe hydrops may require preterm delivery.
Inadvertent early delivery because of incorrect estimation of GA is increasingly uncommon.
Problems of preterm birth are related to difficulty in extrauterine adaptation due to immaturity of organ system.
Respiratory. Preterm infants may experience the following:
Perinatal depression in the delivery room due to poor transition to breathing (see Chaps. 5 and 55).
RDS due to surfactant deficiency and pulmonary immaturity (see Chap. 33).
Apnea due to immaturity in mechanisms controlling breathing (see Chap. 31).
Chronic lung disease (CLD) of prematurity formerly called bronchopulmonary dysplasia (BPD), Wilson-Mikity disease, and chronic pulmonary insufficiency of prematurity (see Chap. 34).
Neurologic. Preterm infants have a higher risk for neurologic problems, including the following:
Cardiovascular. Preterm infants may present with cardiovascular problems, including the following:
Hypotension
Hypovolemia.
Cardiac dysfunction.
Sepsis-induced vasodilation.
Patent ductus arteriosus is common and may lead to pulmonary overcirculation and diastolic hypotension (see Chap. 41).
Hematologic. Conditions for which preterm infants are at higher risk include the following: