Background
The risk of preterm birth increases with plurality. However, data are limited about the role of cervical length in triplet pregnancies and how the greater predisposition for preterm birth in triplet pregnancies, compared with twin pregnancies, is reflected by cervical length. Specifically, it is unclear whether the greater predisposition of triplet pregnancies for preterm birth is reflected by a more rapid cervical shortening during gestation compared with twin pregnancies (and therefore a shorter cervical length at any given gestational age), by a greater risk for preterm birth per given cervical length at any given gestational age, or both.
Objective
The purpose of the study was to compare the rate of cervical shortening during gestation and the correlation between cervical length and gestational age at birth in asymptomatic women with triplet vs twin pregnancies.
Study Design
This was a retrospective study of women with triplet or twin pregnancies who were who were observed in a tertiary center who underwent serial sonographic measurement of cervical length from 16–32 weeks gestation. Change in cervical length during gestation and relationship of cervical length with gestational age at birth were compared between the triplets and twins groups.
Results
A total of 431 measurements of cervical length from 86 women with triplets was analyzed and compared with 2826 measurements of cervical length from 441 women with twins. The rate of cervical shortening among triplet pregnancies was higher than among twin pregnancies starting from 18 weeks of gestation (slope of regression line, –1.297 vs –0.907; P < .001). Similarly, the proportion of women with cervical length of <25 mm or 15 mm was higher among triplet pregnancies than among twin pregnancies (34.0% vs 21.0% [ P < .001] and 16.7% vs 8.4% [ P = .001]), respectively. For any given cervical length measured after 22 weeks of gestation, the associated gestational length at birth in triplet pregnancies was lower by 2.7 weeks on average compared with twin pregnancies ( P < .001).
Conclusion
The higher rate of preterm birth in triplet pregnancies, compared with twin pregnancies, is reflected by both a more rapid cervical shortening during gestation and a lower gestational age at birth per any given cervical length.
Preterm birth (PTB) is the leading cause of perinatal death and morbidity. The risk of PTB is especially high in multifetal gestations and increases with plurality. For example, the rate of PTB at <34 and <32 weeks in triplet pregnancies has been shown to be 50% and 30%, compared with 17% and 9% in twin pregnancies, respectively.
Early prediction of PTB is of major importance, and sonographic cervical length (CL) is 1 of the important predictors of PTB in both singleton and twin pregnancies. However, data regarding the role of CL in triplet pregnancies and how the greater predisposition for PTB in triplet pregnancies, compared with twin pregnancies, is reflected by CL are limited. Specifically, it is unclear whether the greater predisposition of triplet pregnancies for PTB is reflected by a more rapid cervical shortening during gestation compared with twin pregnancies (and therefore a shorter CL at any given gestational age), by a greater risk for PTB per given CL at any given gestational age, or both. This information is of importance because it may assist clinicians in correctly interpreting CL at different points during gestation in women with triplet pregnancies. Only few reports assessed the role of CL in triplet pregnancies at different time points during gestation, and only 1 of these studies compared the rate of cervical shortening between triplet pregnancies (n = 7) and twin pregnancies (n = 13).
Thus, our aim was to compare the rate of cervical shortening during gestation and the relationship between CL and gestational age at birth in asymptomatic women with triplet vs twin pregnancies.
Methods
Study population
This was a retrospective cohort study. The study group included all women with triplets who were observed in the Multiple Gestations Clinic of a single tertiary referral center (Sunnybrook Health Sciences Centre, Toronto, Canada) between January 2000 and December 2014. Changes in CL during gestation and pregnancy outcomes were compared with a control group of women with twin pregnancies who were observed in the same clinic between January 2012 and December 2014. Pregnancies that were complicated by any of the following conditions were excluded: <2 measurements of CL during gestation, cervical cerclage, uncertain pregnancy dating, indicated PTB at <34 weeks of gestation for maternal or fetal indications, gestational age at birth <24 weeks, birthweight of any of the fetuses at <500 g, stillbirth or reduction of ≥1 fetuses, complicated monochorionic pregnancies (ie, twin-to-twin transfusion syndrome, selective intrauterine growth restriction), monoamniotic twins or triplet pregnancies, or genetic or structural anomalies. The study was approved by the Sunnybrook Health Sciences Center Research Ethics Board.
Monitoring of CL
All women who were observed in the Multiple Gestations Clinic underwent serial transvaginal measurement of CL every 2–3 weeks at 18–32 weeks of gestation. Progesterone was not used in the treatment of women with triplet pregnancies or twin pregnancies and a short cervix, given the lack of solid evidence regarding the benefit of progesterone in this context. Cervical cerclage was performed in selected cases of women with suspected mechanical cervical incompetence; these cases were excluded from the analysis. All sonographic measurements that were included in the study involved only asymptomatic women.
All sonographic examinations were performed by experienced sonographers. The measurement of CL was performed transvaginally after the women emptied their bladder and according to the standard technique. Briefly, the measurement of CL was performed in the sagittal plane, visualizing the full length of the cervical canal from the internal os to the external cervical os while exerting as little pressure with the transducer as possible. At least 3 measurements were obtained; the shortest measurement was recorded.
Data collection
Data were extracted from the electronic ultrasound reports and the electronic medical charts and included demographic and obstetric characteristics, chorionicity, validation of gestational age by first trimester ultrasound scan, pregnancy complications, presence of cervical cerclage, and neonatal outcome. All ultrasound reports were reviewed in detail for information on CL.
Statistical analysis
The chi-square test was used to compare categoric variables between the triplets and twins groups; the Student t test and Mann-Whitney U -test were used for continuous variables, as appropriate.
The change in CL as a function of gestational age and the relationship between gestational at birth as a function of CL were compared between women in the triplets and twins groups and were described with the use of mixed linear modeling to account for the repeated measurements of CL in each patient. The analysis of covariance procedure was used to compare the regression lines of the triplets and twins groups.
The correlation between CL and gestational age was assessed at different time points during gestation (≤22, 23–24, 25-26, and ≥27 weeks of gestation) with the use of the Spearman’s correlation coefficient and was compared between the triplets and twins groups with the use of the Fisher’s Z-transformation. All probability values were 2-sided. The level for declaring statistical significance was set to .05. Statistical analysis was performed with the SPSS software (version 21.0; IBM Corp., Armonk, NY).
Results
Characteristics of the study population
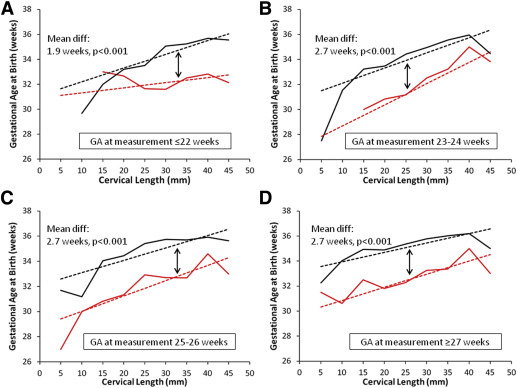
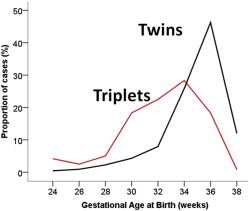
Overall, 86 women with triplet pregnancies who had a total of 431 measurements of CL were identified during the study period, and the data were compared with 441 women with twins who underwent a total of 2826 measurements of CL. The triplets and twins groups were similar with respect to their baseline characteristics, except for a lower gestational age at birth in the triplets group (32.2 ± 3.6 vs 35.4 ± 2.4 weeks of gestation; P < .001; Table 1 ). The distribution of gestational age at birth for the 2 groups is presented in Figure 1 .
| Characteristic | Triplet pregnancies (n = 86) | Twin pregnancies (n = 441) | P value |
|---|---|---|---|
| Mean maternal age, y±SD | 33.2 ± 4.8 | 32.9 ± 4.1 | .5 |
| >35 Y, n (%) | 26 (30.2) | 170 (38.5) | .1 |
| Nulliparity, n (%) | 56 (65.1) | 252 (57.1) | .2 |
| Median cervical length measurements, n (interquartile interval) | 5 (3–9) | 6 (5–8) | .3 |
| Gestational age at birth, wk±SD | 32.2 ± 3.6 | 35.4 ± 2.4 | <.001 |
| <34 Wk, n (%) | 48 (55.8) | 70 (15.9) | <.001 |
| <32 Wk, n (%) | 29 (33.7) | 35 (7.9) | <.001 |
| Cesarean delivery, n (%) | 86 (100.0) | 295 (66.9) | <.001 |
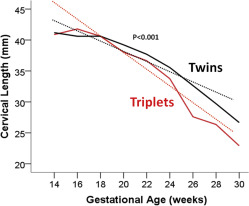
Change in CL during gestation
The change in CL during gestation in the triplets and twins groups is presented in Figure 2 . Starting at 18 weeks of gestation, CL became shorter among triplet pregnancies, and the difference in CL increased with gestation. The slope of regression line that described CL as a function of gestational age in triplet pregnancies was significantly larger than that of the twins group (–1.297 vs –0.907; P < .001), which confirms that cervical shortening during gestation is more rapid in triplet pregnancies compared with twin pregnancies ( Figure 2 ).
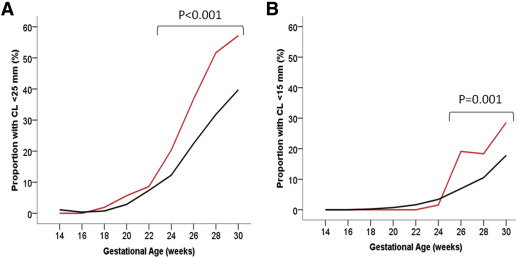
Similar findings were observed when CL was analyzed as a dichotomous variable ( Figure 3 ). The proportion of women with CL <25 and <15 mm was higher in triplet pregnancies starting from 22 weeks of gestation (34.0% vs 21.0%; P < .001; Figure 3 , A) and 24 weeks of gestation (16.7% vs 8.4%; P = .001; Figure 3 , B), respectively.
Relationship between CL and gestational age at birth
We next compared the relationship of gestational age as a function of CL between the triplets and twins groups. Because this relationship is likely to vary with gestational age at the time of measurement of CL, we assessed this relationship at different time points during gestation: ≤22, 23-24, 25-26, and ≥27 weeks of gestation ( Figure 4 ). For any given CL measured at ≤22 weeks of gestation, gestational age at birth for triplets was lower by 1.9 weeks on average compared with twin pregnancies ( P < .001; Figure 4 , A). For any given CL measured at >22 weeks of gestation, gestational age at birth for triplets was lower by 2.7 weeks on average compared with twin pregnancies ( P < .001; Figure 4 , B, C, and D).