19.3 The child of uncertain sex
• bilateral non-palpable testes
• perineal hypospadias with a bifid scrotum
• hypospadias and unilateral non-palpable gonad
• a phenotypical female with a palpable gonad
Normal sexual differentiation
1. Establishment of chromosomal sex at fertilization, with XY as male and XX as female
2. Determination of gonadal sex, when the bipotential gonad develops into a testis or an ovary
3. Development of phenotypic sex, as a result of gonadal differentiation and gonadal hormone production.
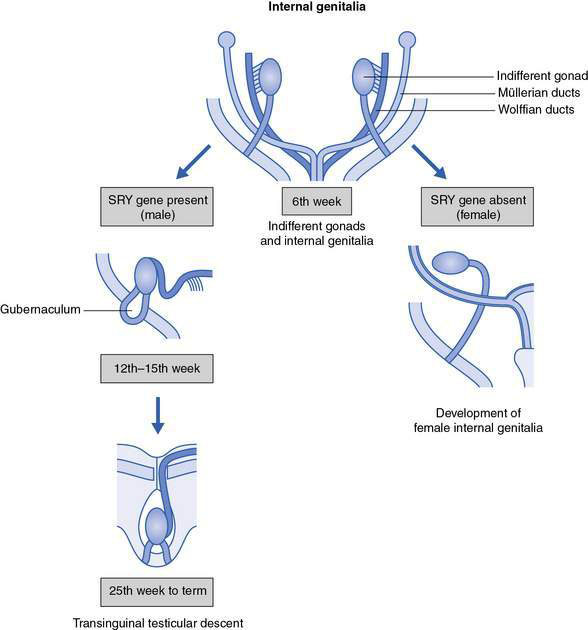
Internal genitalia
Up until about 7 weeks, male and female embryos develop in an identical fashion, with bipotential gonads and both wolffian and müllerian internal genital ducts present (Fig. 19.3.1).