Fig. 25.1
“One stop uterine diagnosis”. (a) 2D ultrasound; (b) Hysteroscopy with the Trophy hysteroscope; (c) Contrast sonography showing cavity of less than 2 cm in sagital plane
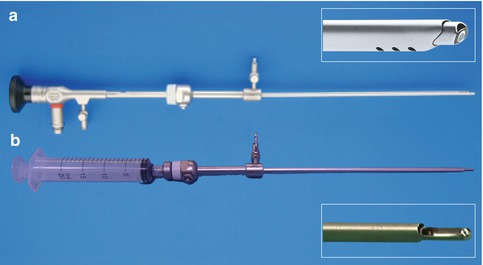
Fig. 25.2
Trophy hysteroscope. (a) Trophy hysteroscope with the diagnostic sheath in active position; (b) Replacement of the scope by the Trophy suction curette
Indication and Contraindication for TsU Correction
There are no standardized criteria for reconstructive surgery of a TsU, because many of these patients do not have obvious symptoms and can carry a pregnancy to term [13]. The published results support that the surgery could be beneficial in patients with long term primary infertility, history of implantation failure, repeated miscarriage and preterm delivery [15, 17, 33]. Patients before start of an in-vitro fertilization (IVF) treatment may also benefit from surgery, but prospective randomized controlled trials are lacking to give a firm recommendation.
Patients with a dysmorphic uterus U1b, also referred to as an infantile uterus, we currently do not see an indication for reconstructive surgery.
Ambulatory Setting
In general, the surgery should be performed in an outpatient hysteroscopy service by an experienced surgeon. The surgery is performed under conscious sedation and the patient can leave the facilities after one hour. Surgery is facilitated in case of a thin endometrium and for this reason most of the authors agree to perform the procedure during the early follicular phase of the menstrual cycle or under oral contraception treatment [11].
No cervical preparation is needed before the metroplasty as it is advised to use a small diameter operative hysteroscope. In contrast, dilation of the cervix to allow the insertion of larger instruments, like the 26 Fr resectoscope, increases the risk of cervical lacerations, perforations and the risk of subsequent cervical incompetence [10, 14].
Special cases, as patient with decompensated disease (American Society of Anesthesiologists class III-IV) or coagulation disorders, should be planned in the conventional operating room, due to the higher risk of complication secondary to their base pathology [12].
Different modalities of sedation/anaesthesia have been proposed to perform the surgery. Our group combines propofol with alfetanil to achieve a grade 3 sedation, according to the Observer’s Assessment of Alertness/Sedation scale [12]. The scheme is safe and the recovery time is short with low side effect [24]. Other authors perform the surgery under general, regional or local-regional anaesthesia, but here the patient compliance is lower and the recovery time longer [40].
Surgical Strategy
The aim of the surgery is to create the normal pear shape anatomy of the uterine cavity through incisions in the redundant myometrium of the lateral wall and if necessary of the fundus (Fig. 25.3).
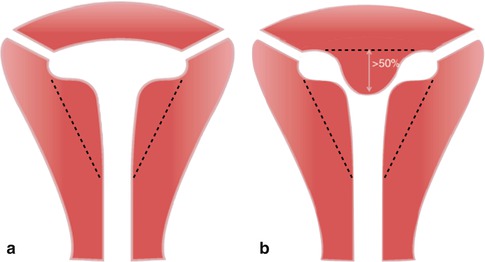
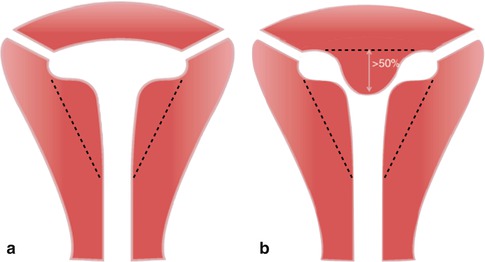
Fig. 25.3
Diagram of the incisions in dysmorphic uterus surgery. (a) Lateral incision in subtype U1a; (b) Lateral and fundal incisions in subtype U1c
The first description of the technique used the hysteroscopic scissors, but since then different reports have been published on the use of the mono or bipolar resectoscope, mini-hysteroscopes with 5 Fr needles or micro-scissors to enlarge the uterine cavity. Mini-Hysteroscopy has brought diagnostic and therapeutic hysteroscopy as a mainstay of modern gynaecological practice. Nowadays, both procedures can be performed in a one-stop sessions at optimal patient comfort. Furthermore, the use of a small diameter hysteroscope and the vaginoscopic approach that follows the anatomical pathway avoids blind cervical dilatation and therefore reduces the risk of cervical trauma, uterine perforations, and postoperative analgesia requirements [9, 19]. It also facilitates working in very small cavities like the dysmorphic uterus.
Instruments
Every hysteroscope with a total diameter less than 5 mm, double flow function and an operative channel for 5 Fr instruments is advised for this kind of surgery.
Especially the new Trophy hysteroscope is appropriate for this kind of minimal invasive surgery. It is a new compact 30° rigid 2.9 mm scope with a special designed instrument tip for atraumatic passage through the cervical canal. The innovative feature is that it can be loaded with accessory sheaths in an active and passive position providing a visually controlled dilatation to a maximal diameter of 4.4 mm.
Preferentially the surgery is performed with the 5 Fr sharp scissors, but also bipolar or unipolar needles are used (Fig. 25.4). If a resectoscope is used, the smaller 22 Fr is loaded with the needle to perform the sidewall incisions.
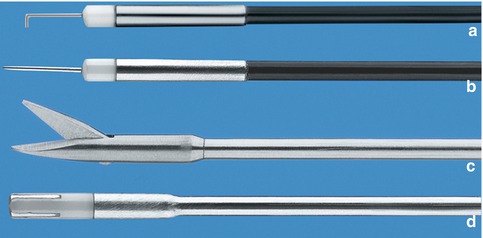
Fig. 25.4
5 Fr instruments possible to use in TsU surgery. (a) Bipolar dissection electrode, angled 90°; (b) Bipolar needle; (c) Sharp scissors; (d) Gordts-Campo Bipolar ball electrode
In an ambulatory setting we recommend only to work with bipolar energy and ionic fluid as distension medium, using a flow and pressure controlled pump unit at the lowest required pressure.
Surgical Technique
The surgery starts with a transvaginal ultrasound to measure the fundal myometrium thickness, in order to confirm the diagnosis and evaluate possible additional fundal incision. If the thickness of the fundus is more than 11 mm, the surgery should include an incision of the fundal myometrium as is done in the surgery for a uterine septum.
The hysteroscope is introduced in the uterine cavity and the T shaped form is confirmed. In case of using the Trophy hysteroscope, gentle activation of the operative sheath is performed and a progressive visual dilatation of the cervical canal up to a diameter of 4.4 cm is performed (Fig. 25.5). Using the 5 Fr sharp scissors, an incision line is made from the tubal ostium to the isthmus uteri. Then successive incisions along the line are made from the isthmus to the cornua, keeping the scissors in parallel with the anterior and posterior wall (Fig. 25.6). The incisions are performed to align the internal tubal ostium with the isthmic point of reference achieving a normal pear shape like cavity (Fig. 25.7). The depth of incision is like for the septum incision determined by the anatomical reference, the myometrial vascularisation and a security zone of approx. 10 mm of myometrium measured by transvaginal ultrasound. Myometrial bleeding can be controlled with the use of the bipolar needle or coagulation probe.

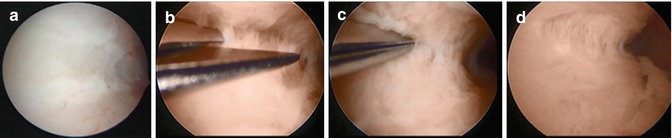
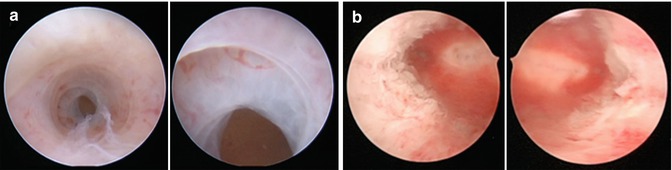

Fig. 25.5
Trophy hysteroscope with the operative sheath. (a) Operative sheath in passive position; (b) Operative sheath in active position
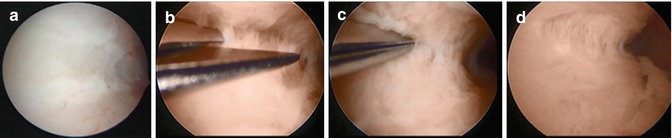
Fig. 25.6
Metroplasty with Trophy hysteroscope and 5 Fr scissors in TsU. (a) Demarcation line from the tubal ostium towards the isthmus; (b) and (c) Lateral incisions with the sharp scissors; (d) Alignment of the two referential marks
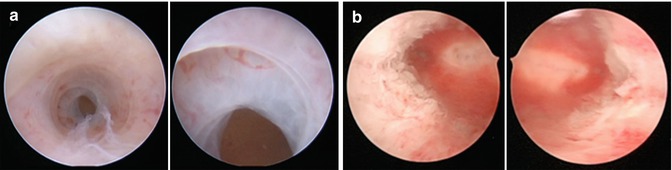
Fig. 25.7
Hysteroscopic view before and after the surgery in U1c malformation. (a) Cylindrical cavity of the TsU during the diagnostic phase; (b) Normal pear shape like cavity after incisions in the fundus and lateral walls
In case the surgeon makes the incision with the bipolar needle, the rules of bipolar surgery for good cutting should be met, firm tissue contact before activating the cutting modus. For this reason, we recommend to insert the needle in the uterine sidewall mechanically only then activate the cutting current with a medial movement, taking care to minimize the thermal injury to the sidewall myometrium (Fig. 25.8).
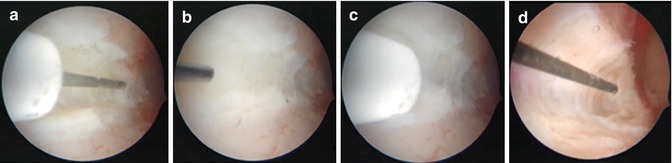
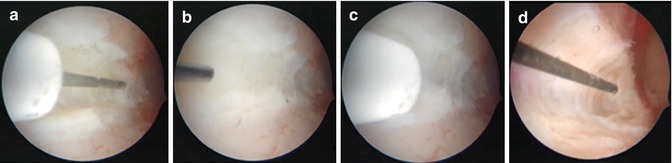
Fig. 25.8
Metroplasty with Trophy hysteroscope and bipolar needle. (a) Line from the ostium to the isthmus; and (b) start mechanical perforation (c) position of bipolar needle before activating power. (d) Incision after activating cutting power
For unipolar surgery and vaporizing electrodes, like the Versapoint® (Gynaecare), the sidewall incision is performed in the conventional way with gentle tissue contact in which no mechanical force may be used.
At the end of the surgery, careful control for arterial bleeding is given by lowering the preinstalled pressure by closing the inflow channel. Anti-adhesion gel barrier (Hyalobarrier®, Nordic Pharma), is inserted in the cavity to prevent postoperative adhesions. The use of this modified derivative of hyaluronic acid is based on the principle of keeping the adjacent wound surfaces mechanically separated and by its natural role in modulation the inflammatory phase of wound healing. Its effectiveness in the prevention of intrauterine adhesions after hysteroscopic adhesiolysis was demonstrated by prospective, randomized, controlled studies [1, 18]. Additionally, a recent systematic review and meta-analysis of the literature concludes that the use of APC gel or polyethylene oxide–sodium carboxymethylcellulose gel following operative hysteroscopy decreases the incidence of de novo adhesions at second-look hysteroscopy at 1–3 months [6].
After inserting the barrier a transvaginal ultrasound is performed taking advantage of the contrast to evaluate the results of the surgery with exact measurements of the cavity and myometrial thickness (Fig. 25.9).
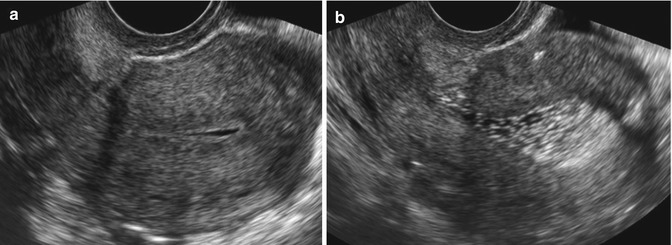
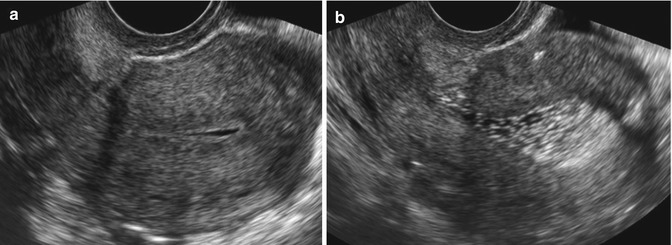
Fig. 25.9
2D Ultrasound in a dysmorphic uterus U1c. (a) Pre-surgery, cavity length 18 mm and fundal thickness 13 mm; (b) Post-surgery US, cavity length 25 mm and fundal thickness 9.8 mm. contrast is due to hyalobarrier®
Postoperative Care
The main postoperative concern is the possible intrauterine adhesion (IUA) formation and it is questioned if any post-operative measurement can contribute to reduce the risk of adhesion formation.
Oestrogen: Use of oestrogen as perioperative adjuvant therapy has been suggested for preventing recurrent adhesions, based on its critical role in stimulating and enhancing endometrial growth via angiogenesis. A recent systematic review concludes that in patient with IUA, hormone therapy is beneficial, however oestrogen therapy needs to be combined with an ancillary treatment to obtain maximal outcomes [23]. Most of the studies used a sequential oestro-progestative combination for 2 months. We recommend to restrict the indication to patient with anovulatory or irregular cycles. In case of normal endocrinological profile with regular menstrual cycles no adjuvant oestrogen therapy is recommended.
Antibiotics: The prevalence of infection following an operative hysteroscopy is low, 1 %. Although antibiotic is still used widely after hysteroscopic surgery recent randomised trials do not find any evidence of benefit and recommend not to implement Antibioprophylaxis routinely as it does not reduce the risk of infection [11, 35].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


