Chapter 439 Systemic Hypertension
Definition of Hypertension
The definition of hypertension in adults is BP ≥140/90 mm Hg, regardless of body size, sex, or age. This is a functional definition relating level of BP elevation with the likelihood of subsequent cardiovascular events. Since hypertension-associated cardiovascular events such as myocardial infarction or stroke usually do not occur in childhood, the definition of hypertension in children is statistical rather than functional. The National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents published the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents (Fourth Report) in 2004. This report established normal values based on the normative distribution of BP in healthy children and included tables with systolic and diastolic values for the 50th, 90th, 95th, and 99th percentile by age, sex, and height percentile. These normative tables can be obtained free online at www.nhlbi.nih.gov/guidelines/hypertension/child_tbl.htm. The Fourth Report defined hypertension as average systolic blood pressure (SBP) and/or diastolic blood pressure (DBP) that is ≥95th percentile for age, sex, and height on ≥3 occasions. Prehypertension was defined as average SBP or DBP that are ≥90th percentile but <95th percentile. In adolescents beginning at age 12 yr, prehypertension is defined as BP between 120/80 mm Hg and the 95th percentile. A child with BP levels ≥95th percentile in a medical setting but normal BP outside of the office has white coat hypertension.
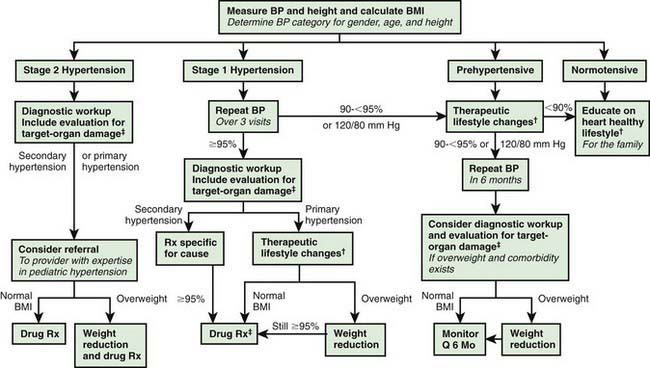
The Fourth Report further recommended that if BP is ≥95th percentile, then the hypertension should be staged. Children with BP between the 95th and 99th percentile plus 5 mm Hg are categorized as stage 1 hypertension, and children with BP above the 99th percentile plus 5 mm Hg have stage 2 hypertension. Stage 1 hypertension, if asymptomatic and without target organ damage, allows time for evaluation before starting treatment; whereas stage 2 hypertension calls for more prompt evaluation and pharmacologic therapy (Fig. 439-1).
Etiology and Pathophysiology
BP is the product of cardiac output and peripheral vascular resistance. An increase in either cardiac output or peripheral resistance results in an increase in BP; if one of these factors increases while the other decreases, BP may not increase. When hypertension is the result of another disease process, it is referred to as secondary hypertension. When no identifiable cause can be found, it is referred to as primary (essential) hypertension. Many factors, including heredity, diet, stress, and obesity, may play a role in the development of primary hypertension. Secondary hypertension is most common in infants and younger children. In general, the younger the child, the higher the BP and the presence of symptoms related to hypertension, the more likely there will be an underlying secondary cause of hypertension. Many childhood diseases can be responsible for chronic hypertension (Table 439-1) or acute/intermittent hypertension (Table 439-2). The most likely cause varies with age. Hypertension in the premature infant is most often associated with umbilical artery catheterization and renal artery thrombosis. Hypertension during early childhood may be due to renal disease, coarctation of the aorta, endocrine disorders, or medications. In older school-aged children and adolescents, primary hypertension becomes increasingly common.
Table 439-1 CONDITIONS ASSOCIATED WITH CHRONIC HYPERTENSION IN CHILDREN
RENAL
VASCULAR
ENDOCRINE
CENTRAL NERVOUS SYSTEM
Table 439-2 CONDITIONS ASSOCIATED WITH TRANSIENT OR INTERMITTENT HYPERTENSION IN CHILDREN
RENAL
DRUGS AND POISONS
CENTRAL AND AUTONOMIC NERVOUS SYSTEM
MISCELLANEOUS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree