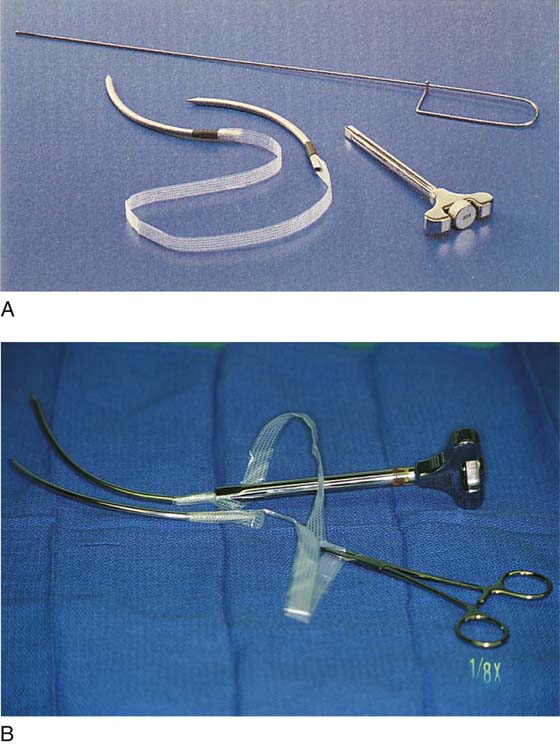
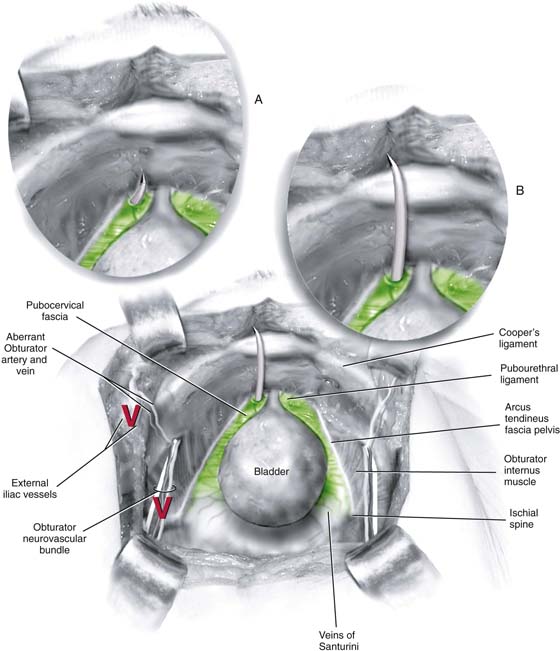
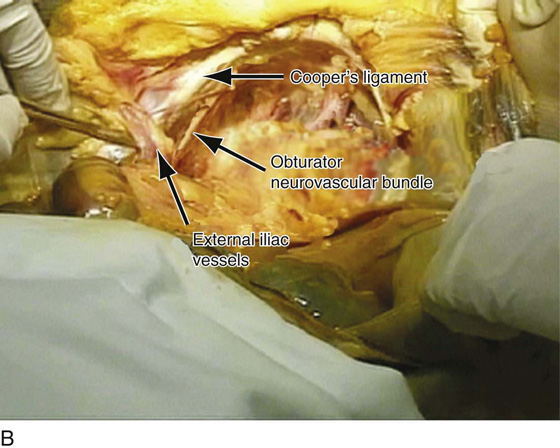
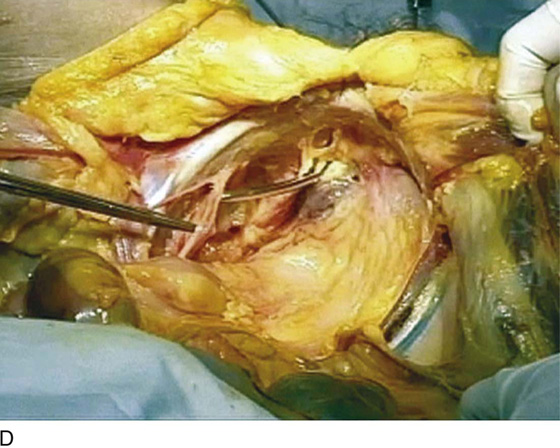
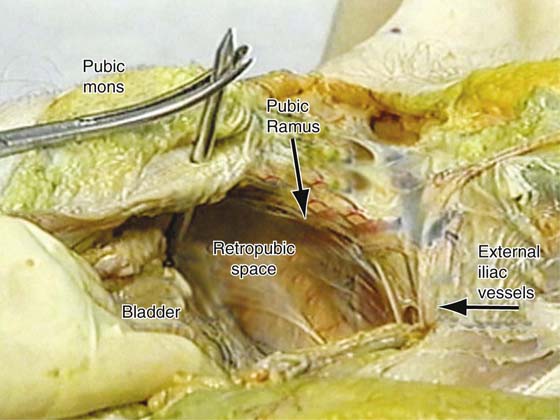
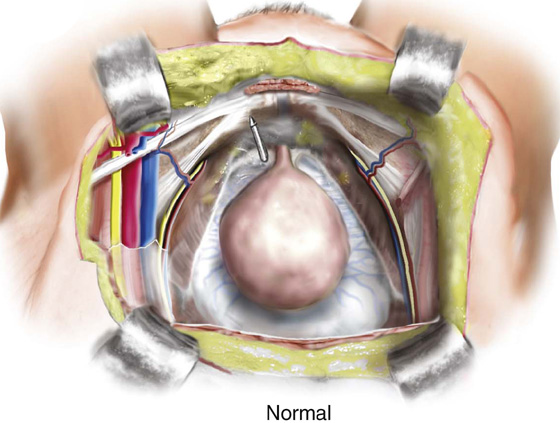
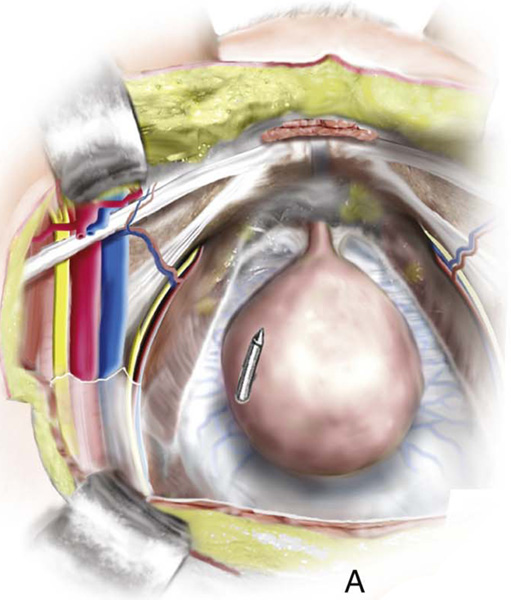
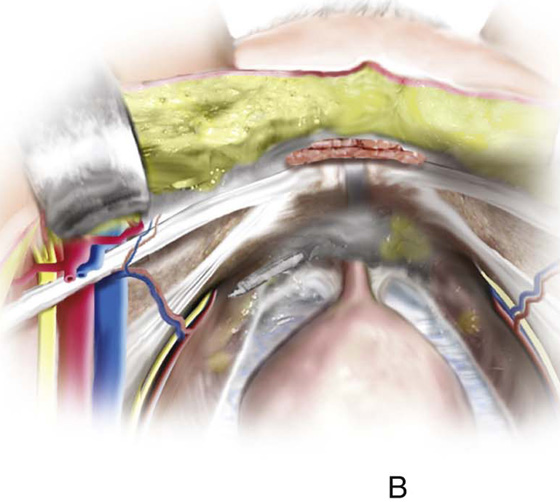
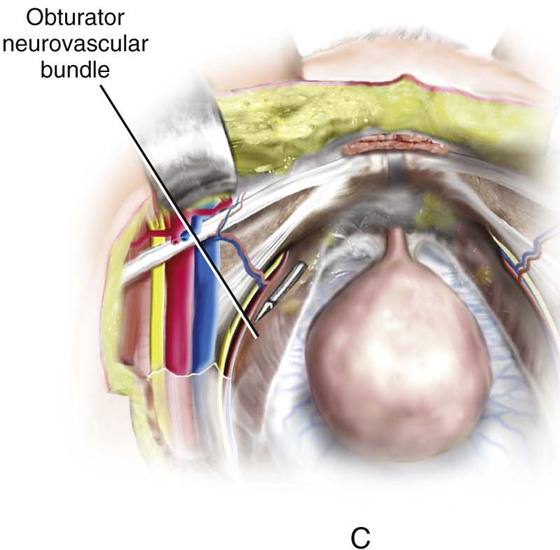
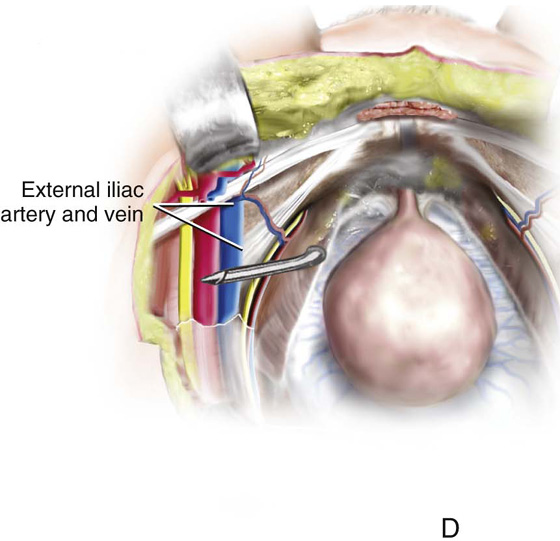
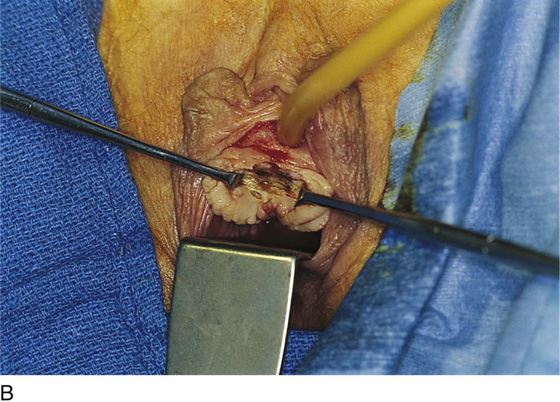
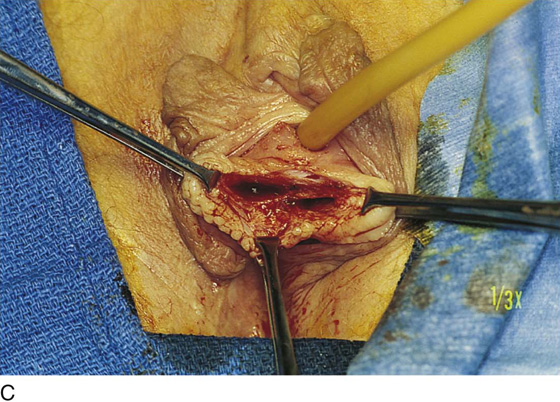
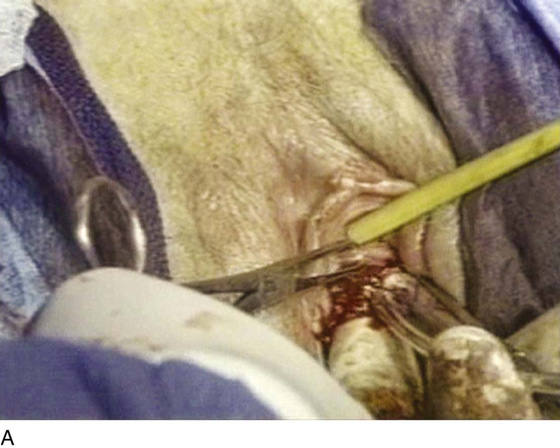
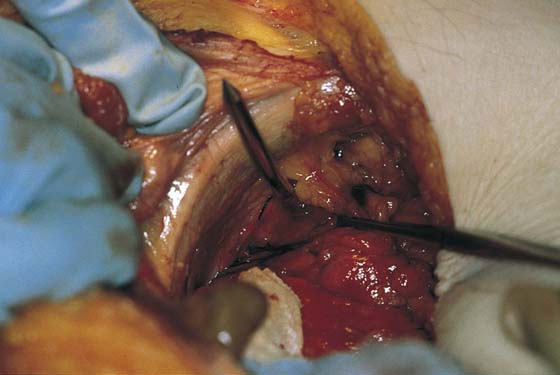
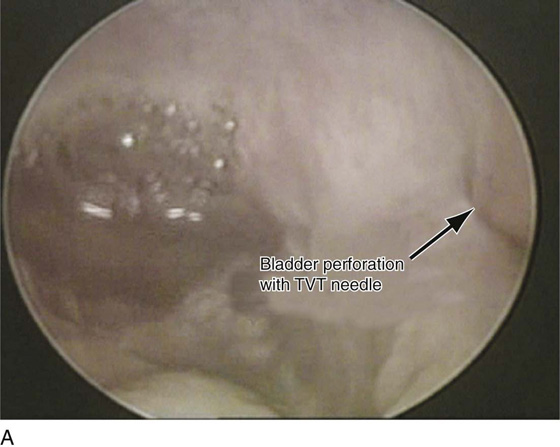
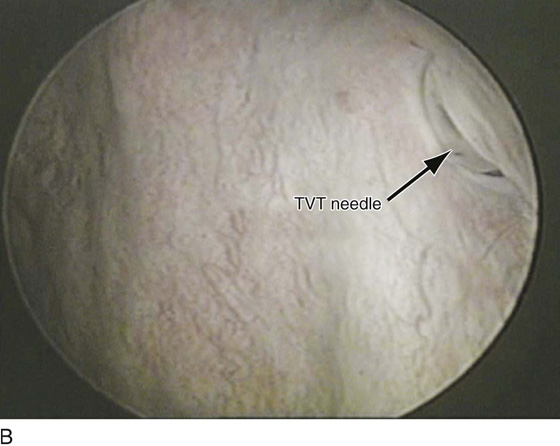
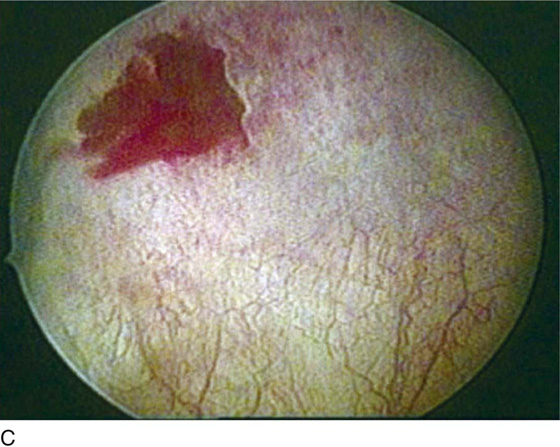
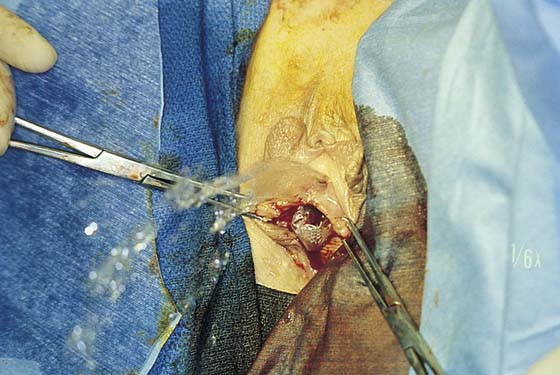
CHAPTER 58 In 1996, Ulmsten et al introduced the first synthetic midurethral sling, which they named the tension-free vaginal tape (TVT) procedure. This procedure introduced the concept of placing a synthetic material (polypropylene) under the midportion of the urethra in a tension-free fashion. The technique quickly gained popularity because it involved minimal vaginal dissection, was easy to learn, and could be performed with the patient under local anesthesia on an outpatient basis. To date several studies have compared the TVT procedure with more traditional retropubic procedures such as the Burch colposuspension and have shown equal to superior cure rates with less morbidity. The success of the original TVT midurethral sling has led to the development of other midurethral slings in an effort to decrease morbidity while maintaining efficacy. In 2001, Delorme described the first transobturator synthetic midurethral sling. The motivation behind the development of this approach was to reduce the risk of bladder perforation and eliminate the risk of bowel or major blood vessel injury, which had been reported with the TVT procedure. Subsequent studies have shown that a transobturator midurethral sling is as efficacious as a retropubic synthetic midurethral sling, if the patient does not have intrinsic sphincter deficiency. More recently, single-incision midurethral slings have been described. The newest version of a polypropylene sling requires only one incision in the vagina because the sling has no exit points. This chapter discusses anatomy and currently recommended techniques for the placement of these various synthetic midurethral slings. The tension-free vaginal tape procedure was the first retropubic synthetic midurethral sling. This ambulatory procedure aims to restore the pubourethral ligament and suburethral vaginal hammock by using specially designed needles attached to a synthetic sling material (Fig. 58–1). The synthetic sling material is made of polypropylene and is approximately 1 cm wide × 40 cm in length. This sling material is attached to two stainless steel needles, which are passed on each side of the urethra blindly through the retropubic space. The needles exit through a previously created stab wound in the suprapubic area. Because this type of sling requires blind passage of a needle through the retropubic space, it is imperative that the surgeon have a clear understanding of the important anatomic structures of the retropubic space, to avoid potential complications (Figs. 58–2 through 58–5). Besides the potential for damaging the urethra or the bladder, there is also potential for injuring important vascular structures, including the obturator neurovascular bundle and the external iliac vessels as they exit the pelvis (see Figs. 58–2 through 58–5). The technique for placement of a retropubic synthetic midurethral sling is as follows: 1. The procedure can be performed with the patient under local, regional, or general anesthesia. If local anesthesia is used, a combination of an anesthetic and a vasoconstrictive agent is usually injected into the abdominal skin just above the pubic symphysis and downward along the back of the pubic bone into the space of Retzius. A small suprapubic incision is made on each side medial to the pubic tubercle at the superior pubic ramus of the pubic bone (Fig. 58–6). 2. Even if the procedure is performed with the patient under general or regional anesthesia, the anterior vaginal wall is always hydrodissected with an anesthetic solution before the incision is made. A midline anterior vaginal wall incision is made at the level of the mid to distal urethra. It should be noted that this area of the vagina is fused to the posterior urethra. This vaginal wall must be sharply separated from the underlying urethra (Fig. 58–7). 3. With Metzenbaum or Mayo scissors, two tunnels are created through the tissue to the level of the inferior pubic ramus on each side. The direction of the tips of the scissors should be toward the ipsilateral shoulder. The tunnel needs to be only large enough to admit the 5-mm TVT needle (see Fig 58–7). 4. The needle is then brought into the field and is attached to a nondisposable handle. The tip of the needle is placed in the tunnel so it is pointing toward the ipsilateral shoulder. The dominant hand holds the handle, and the index finger of the nondominant hand is placed in the anterior vaginal wall with the thumb placed on the back of the disposable needle (Fig. 58–8). In this way, the appropriate tension required to penetrate the urogenital diaphragm with the needle is best appreciated. Once the tip of the needle has penetrated the urogenital diaphragm, the handle should be dropped in an inferior direction, and the tip of the needle moved medially and superiorly so that it hugs the back of the pubic bone (Fig. 58–9). The needle is then advanced to the posterior aspect of the rectus muscle and penetrates up through the anterior abdominal fascia to exit from the previously created suprapubic stab wound. 5. With the needle in place, cystoscopy is performed with a 70° cystoscope to ensure that no inadvertent penetration of the needle through the bladder occurs. During cystoscopy, it is important to aggressively distend the bladder so that any subtle indentations or penetrations from the needle will be visualized (Fig. 58–10). The needle is then withdrawn through the stab incision, and the same procedure is repeated exactly on the opposite side. In this way, the Prolene tape covered by a plastic sheath is placed in a U shape around the urethra (Figs. 58–11 and 58–12). The technique utilized to determine the appropriate tension of the TVT sling is done at the discretion of the surgeon. If local anesthesia is used, a cough stress test can be attempted to create the sign of stress incontinence (see Fig. 58–11). If general anesthesia is used, suprapubic pressure can be used to create urinary leakage. The sling material is adjusted until only a slight amount of leakage is visualized with these provocative maneuvers. The plastic sheath is then removed while the tape is stabilized with a right-angle clamp or Metzenbaum scissors (Figs. 58–13 and 58–14). The tape can be further adjusted after the plastic sheath is removed by stretching with a right-angle clamp. Ultimately, in most patients, the tape should sit very loosely at the level of the midurethra, easily allowing placement of an instrument between the tape and the urethra (Fig. 58–15). The sling material is not fixed or sutured to the endopelvic fascia or the rectus fascia, but is simply cut on each side at the level of the skin. The vaginal and abdominal incisions are closed. FIGURE 58–1 A. Tension-free vaginal tape (TVT) instrumentation, including (clockwise from top) a Foley catheter guide, a needle introducer/handle, and specially designed needles attached to a synthetic suburethral sling tape. B. Needles have been attached to the handle. A hemostat has been placed on the overlapping plastic sheath. FIGURE 58–2 The retropubic space is visualized. The urethra and the bladder sit on the muscular lining of the vagina (green). A. The needle should penetrate the urogenital diaphragm and enter the retropubic space just medial to the arcus tendineus fascia pelvis and lateral to the urethra. B. It should then maintain direct contact with the back of the pubic bone as it passes toward the anterior abdominal stab wound. Marked with a red “V” are the obturator neurovascular bundle and the external iliac vessels, which should be well away from the tip of the tension-free vaginal tape (TVT) needle. FIGURE 58–3 A. View of the retropubic space of a fresh cadaver. B. Cooper’s ligament, the obturator neurovascular bundle as it exits the pelvis through the obturator foramen, and the external iliac vessels as they exit the pelvis under the inguinal ligament are marked. C. A tension-free vaginal tape (TVT) needle has been passed in an appropriate fashion on the left side of this cadaver. D. The TVT needle is intentionally continued in a cephalad-lateral direction, and one can see how it can easily come into contact with the obturator neurovascular bundle in the retropubic space. E. The TVT needle is intentionally continued in this direction, and one can see how it could potentially come in contact with the external iliac vessels. FIGURE 58–4 Retropubic view of an embalmed cadaver. Note the appropriate passage of the tension-free vaginal tape (TVT) needle on the right side and the normal anatomy of other structures in the retropubic space. FIGURE 58–5 Retropubic view of appropriate safe passage of a retropubic tension-free vaginal tape (TVT) needle (Normal). A. Cephalad migration of the needle away from the back of the pubic bone is the most common cause of bladder perforation. B. External rotation of the handle will initially result in penetration of the obturator internus muscle by the needle tip, with the potential to injure aberrant vessels along the lateral pelvic sidewall. C. Continued external rotation of the handle with cephalad migration of the needle may result in injury to the obturator neurovascular bundle or (D) the external iliac vessels. FIGURE 58–6 Site of suprapubic incisions for the tension-free vaginal tape (TVT) procedure. FIGURE 58–7 A. The external urethral meatus is grasped with an Allis clamp at 6 o’clock. B. A small midline incision is made at the level of the midurethra. C. Mayo or Metzenbaum scissors are utilized to create a tunnel to the inferior pubic ramus. The urogenital diaphragm is not penetrated. FIGURE 58–8 Proper technique for passing a tension-free vaginal tape (TVT) needle. A. The tip of the needle is placed in the small tunnel that has been created and should come into direct contact with the inferior pubic ramus, pointing toward the ipsilateral shoulder. B. With the index finger of the nondominant hand in the vagina and the thumb on the shaft of the needle, the tip is pushed through the urogenital diaphragm. C. Once the resistance of the urogenital diaphragm is overcome, the handle is dropped and the needle is moved in a medial and superior direction, while direct contact with the back of the pubic bone is maintained. Cephalad migration must be avoided. The tip of the needle is then palpated suprapubically and is guided to exit through the previously created stab incision. FIGURE 58–9 The direction of the needle along the back of the pubic bone is demonstrated in a cadaver. FIGURE 58–10 A. Bladder perforation with a tension-free vaginal tape (TVT) on the patient’s left side. B. The shaft of the needle is now visible as it is withdrawn back into the vagina. C. The defect that is left in the bladder. FIGURE 58–11 The tape has been passed suprapubically on both sides. Leakage of urine during a coughing stress test indicates the need for adjustment of the sling material. FIGURE 58–12 Tension-free vaginal tape (TVT) needles and a plastic sheath containing Prolene tape have been passed up through suprapubic stab wounds. FIGURE 58–13 A right-angle clamp stabilizes the Prolene while the plastic sheath is being withdrawn suprapubically. FIGURE 58–14 Prolene tape after the plastic sheath has been removed.
Synthetic Midurethral Slings for the Correction of Stress Incontinence
Retropubic Synthetic Midurethral Slings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Apurva B. Pancholy
Apurva B. Pancholy