Fig. 1
(a and b) Simple or cutaneous syndactyly. This is a complete syndactyly, best demonstrated from the palmar surface (Copyright Charles A. Goldfarb, MD)
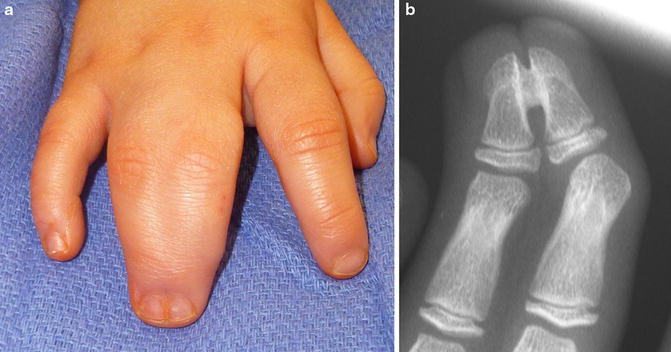
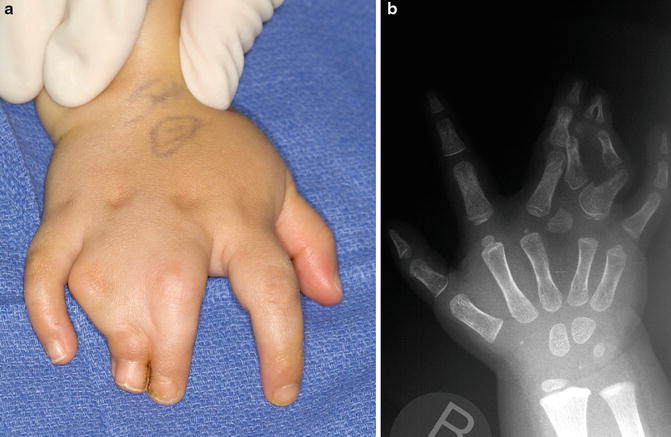
Fig. 2
(a) Clinical appearance of complex syndactyly demonstrating synonychia and tight approximation of distal phalanges (copyright Charles A. Goldfarb, MD). (b) Radiographs show connection between distal phalanges (Copyright Charles A. Goldfarb, MD)

Fig. 3
Incomplete syndactyly of the ring and small fingers (Copyright Charles A. Goldfarb, MD)
Kozin proposed a modification of this classification scheme to include the digits involved and the severity of the interconnection (Kozin 2001). Kozin’s classification system provides guidance into the timing and optimal technique for operative intervention. Simple syndactyly (SS) was divided into standard (s), complicated (c), and urgent (u) subtypes. Complex syndactyly (CS) also was further subdivided into standard (s), complicated (c), and unachievable (u) subtypes.


Simple Syndactyly (SS)
Standard (SSs): Straightforward syndactyly on a non-border digit. Surgery can be delayed until 18 months of age or later.
Complicated (SSc): Simple syndactyly associated with additional soft tissue interconnections, syndromes (e.g., Poland syndrome, central deficiency), or additional bony elements (e.g., hypoplasia). Treatment is individualized and neurovascular anomalies may exist.
Urgent (SSu): Soft tissue syndactyly of border digits or digits of unequal length, girth, or joint level. It requires early separation to prevent angular and rotational deformity of the tethered digit.
Complex Syndactyly (CS)
Standard (CSs): Complex syndactyly of adjacent phalanges without additional bony abnormalities (e.g., without delta phalanx, symphalangism).
Complicated (CSc): Complex syndactyly associated with bony interconnections (e.g., transverse phalanges, symphalangism, polysyndactyly) or syndromes (to include amniotic constriction band). Treatment is individualized with the consideration that digits may function better as a unit (Figs. 4 and 5).
Unachievable (CSu): Complex syndactyly with severe abnormalities of the underlying bony structure that often prohibits formation of a five-digit hand.

Fig. 4
A three-year-old with ulnar deficiency and syndactyly. Distal phalangeal tufts are fused and a common fingernail or synonychia crosses the bony mass (Courtesy of Shriners Hospital for Children, Philadelphia)

Fig. 5
A three-year-old with amniotic band disruption sequence and complicated syndactyly (Courtesy of Shriners Hospital for Children, Philadelphia)
Tentamy and McKusick classified isolated, non-syndromic syndactyly to include five different types (Flatt 2005; Tentamy and McKusick 1978; Tonkin 2009).
Syndactyly type I (SD I, zygodactyly) is the most common type, affecting the long-ring web space with possible involvement of the second and third toes. It may be complete or incomplete and bilateral or unilateral and usually autosomal dominant with variable penetrance.
Syndactyly type II (SD II, synpolydactyly) also involves the long-ring web space and possibly the fourth and fifth toes, but includes a duplication of the ring finger within the syndactylous web (Fig. 6).
Syndactyly type III (SD III) is characterized by syndactyly at the ring-small finger web space. It may occur as an isolated syndactyly but is also seen in oculodentodigital syndrome.
Syndactyly type IV (SD IV, Haas type) is extremely rare and involves complete syndactyly of all digits.
Syndactyly type V (SD V) involves fusion of the metacarpals and metatarsals, most commonly of the ring and small fingers and third and fourth toes.
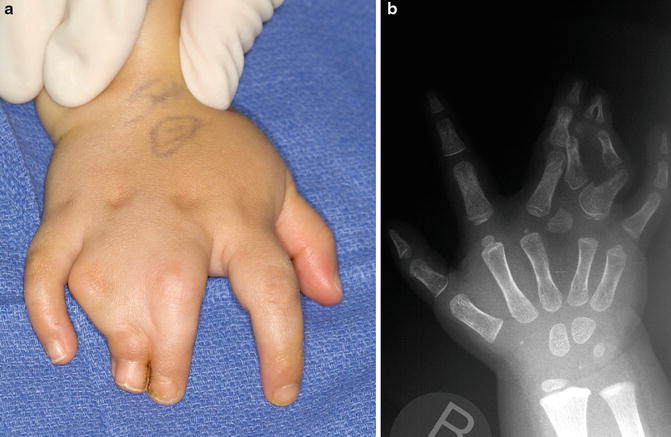
Fig. 6
A two-year-old with syndactyly combined with duplication of the ring finger (synpolydactyly) (Courtesy of Shriners Hospital for Children, Philadelphia). (a): Dorsal view of hand with syndactyly. (b): X-ray reveals ring finger duplication with awkward interconnections
Since their original description, four additional types have been added to the Tentamy and McKusick classification (Jordan et al. 2012).
Syndactyly type VI (SD VI, Mitten Hand)
Syndactyly type VII (SD VII, Cenani-Lenz)
Syndactyly type VIII (SD VIII)
Syndactyly type IX (SD IX, Mesoaxial)
Within complex syndactyly, Apert acrosyndactyly has been further classified. The three types of (Fig. 7) syndactyly all involve complex syndactyly of the second through fifth digits with increasing involvement of the thumb: type 1 (spade hand) has a free thumb with a narrow first web space, type 2 (spoon hand) has a simple syndactyly of the thumb to the index finger, and type 3 has a complex syndactyly of the thumb to the index finger (Upton 1991). This classification has been further modified by Van Heest, based on angular deformity of the metacarpophalangeal joint and rotation deformity of the digits. Treatment goals and procedure recommendations are based on this classification system.
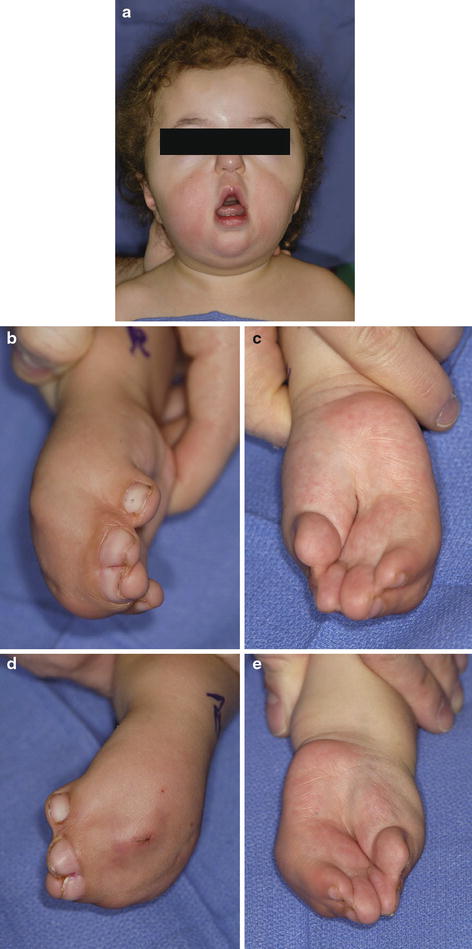
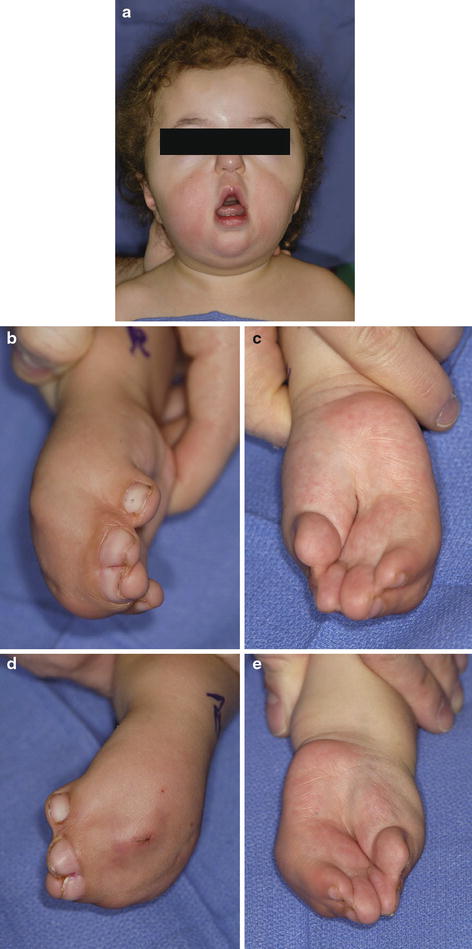
Fig. 7
A two-year-old with Apert syndrome (Courtesy of Shriners Hospital for Children, Philadelphia). (a): Typical facies. (b): Dorsal view right hand with severe syndactyly including thumb-index web space. (c): Palmar view right hand with deep crevasses. (d): Dorsal view of left hand. (e): Palmar view of left hand
Outcome Assessment
Although there is no outcome scale or tool designed specifically to assess the results of syndactyly treatment, there is general consensus on important outcome measures. Range of motion, digit deformity (angulation and rotation), scar quality (Vancouver Scar Scale), and web creep are all utilized in assessing outcomes.
Range of motion can be assessed via measurement of the individual joints, but total active motion, as described by Strickland and Glogovac, is commonly utilized. Total active motion is the sum of active flexion of the PIP and DIP joint minus composite extension deficits; normal is 175° (Strickland and Glogovac 1980).
Digit deformity is an assessment of both the rotation and angulation of the digit. Rotation (supination or pronation) describes the plane of the distal phalanx relative to the plane of the proximal phalanx; a goniometer placed on the dorsal surface of the distal phalanx is to measure the degree of difference in these planes (Goldfarb et al. 2012). To determine digital angulation, the deviation of the longitudinal axis of the distal phalanx from the longitudinal axis of the proximal phalanx is measured with a goniometer.
Additional assessment measures may be utilized to evaluate the outcomes of syndactyly reconstruction. Although originally designed for assessment of scars in burn patients, the Vancouver scar scale (VSS) has been applied to the assessment of syndactyly to provide an objective measure of scar quality compared to normal skin (Goldfarb et al. 2012; Lumenta et al. 2010). This scale incorporates four variables including vascularity, height/thickness, pliability, and pigmentation and assigns points to each parameter to generate a composite score (Sullivan et al. 1990).
Web creep is the distal migration of the commissure after syndactyly reconstruction. The most commonly used scale to assess creep is a five-point scale described by Withey that grades creep based on the location of the distal commissure relative to the proximal interphalangeal (PIP) joint (Withey et al. 2001). Zero points are awarded to a normal web with soft skin, 1 point for thickening of the web without advancement, 2 points for web creep one-third of the distance from the palmar metacarpophalangeal (MCP) joint to the PIP joint crease, 3 points for web creep two-thirds of the distance from the palmar MCP to the PIP joint crease, and 4 points for web creep from the palmar MCP to PIP joint crease.
Treatment
Nonoperative Management
Indications/Contraindications
The goal of syndactyly management is to create a more functional and aesthetically normal hand. As such, operative intervention is often indicated; however, in certain situations surgery is either contraindicated or not warranted.
An absolute contraindication to surgical intervention is the presence of medical comorbidities that render the patient unable to undergo anesthesia. A relative contraindication is the presence of digits that lack the requisite anatomic structures, including muscles, tendons, and ligaments, to function as stable, independent, mobile digits when separated. This can occur in symbrachydactyly, synpolydactyly, or other complex syndactylies, in which the digits may be more functional as a unit. While surgery may improve hand appearance, it would not improve, and may impair, function. The presence of a super digit, in which two metacarpals support a single oversized digit (type I super digit) or a single metacarpal supports multiple digits (type II super digit), is also a relative contraindication (Wood 1990). If one of the digits becomes stiff, atrophic, and aesthetically displeasing, surgical separation may be warranted. Finally, surgery may not be warranted in patients who experience minimal functional impairment. This is most often the case for simple, incomplete syndactylies as surgical intervention may improve the aesthetic appearance of the hand, but it would not substantially alter function. Careful discussion with patients and families regarding the benefits and risks of surgical intervention in these cases is undertaken before proceeding (Table 1).
Table 1
Syndactyly nonoperative management
Indications |
|---|
Simple, incomplete syndactyly without functional impairment |
Medical comorbidities prohibiting surgery |
Digits lacking anatomic structures to enable independent digital function |
Super digit |
There are no recognized nonoperative treatment modalities for the management of syndactyly.
Operative Treatment
Indication/Contraindications
Syndactyly of any type can be an indication for surgery, most importantly if it impairs function. Numerous techniques have been described to reconstruct syndactylized digits; these techniques vary based on the digits involved and the complexity of deformity. There are three basic objectives in syndactyly reconstruction: separation of the digital skin, reconstruction of the web space, and soft tissue coverage of the released digits. In complex syndactyly, a fourth objective, separation of the nail and osseous connection with nail wall reconstruction must also be achieved (Table 2).
Table 2
Syndactyly operative management
Indications | Contraindications |
|---|---|
Syndactyly causing functional impairment | Simple, incomplete syndactyly without functional impairment |
Medical comorbidities prohibiting surgery | |
Digits lacking anatomic structures to enable independent digital function | |
Super digit |
Surgical Procedure: Simple and Complex Release (Incomplete and Complete)
Preoperative Planning
Prior to operative intervention, several factors are considered, including the timing of surgery and the order in which the web spaces will be addressed when multiple digits are involved.
Although the precise age at which surgery should be performed remains an open question that is influenced by a number of factors, consensus is emerging. Most surgeons advocate performing syndactyly reconstruction prior to 2 years of age, as patterns of hand function develop between 6 and 24 months (Hutchinson and Frenzen 2010). Additionally, performing surgery before school age, 5 years in most cases, may avoid social stigma and lessen psychological concerns (Vekris et al. 2010). For most syndactylies, surgery is considered after 6 months of age to minimize anesthetic risk and allow sufficient growth to facilitate operative intervention. When syndactyly involves border digits (i.e., thumb-index or ring-small finger syndactyly), earlier surgical intervention, between 3 and 6 months old, is considered as the differential digital lengths may result in angular and/or rotational deformity as the shorter digit tethers the longer one (Fig. 8).


Fig. 8
Syndactyly between digits of unequal length leads to tethering of the longer digit, which results in a flexion contracture and rotational deformity (Courtesy of Shriners Hospitals for Children, Philadelphia)
Syndactyly involving multiple digits is typically performed in a staged fashion to minimize the risk of vascular compromise to digits supplied by a single artery. When all digits are involved, reconstruction of the first and third web spaces, followed by release of the second and fourth web spaces 3–4 months later, has been recommended (Hutchinson and Frenzen 2010).
Prior to the procedure, the patient’s clinical history, physical exam, and radiographs are reviewed. The pediatrician and anesthesia team clears syndromic patients for surgery. The operating room setup requires a standard operating bed and hand table. Fluoroscopy is not required for simple syndactyly release. Standard operating equipment is utilized (Table 3).
Table 3
Simple syndactyly release preoperative planning
Preoperative planning |
|---|
OR table: standard operating table with hand table on the patient’s affected side |
Position/positioning aids: the patient is resting supine on the OR table with the affected upper extremity supinated on the hand table |
Fluoroscopy location: not required for simple syndactyly release |
Equipment: 15c scalpel blades, bipolar electrocautery, tenotomy scissors, absorbable suture |
Tourniquet (sterile/non-sterile): non-sterile or tourniquet applied to affected upper extremity. Tourniquet position should not preclude access to the antecubital fossa for harvesting of full-thickness skin graft |
Positioning
Positioning is identical for all syndactyly releases and reconstructions. The patient is positioned supine on a standard operating table fitted with a hand table. The patient is close to the edge of the operating table on the affected side, to allow the entire involved upper extremity to be positioned on the hand table. The skin graft donor site is sterilely prepared and draped.
Surgical Approach
Technique: Simple Complete Syndactyly
The key to a successful syndactyly reconstruction depends on the recreation of the commissure. Optimally, the commissure slopes 45–50° from dorsal to palmar and extends one half the length of the proximal phalanx (Kozin 2001). Numerous flap designs for the reconstruction of the commissure have been described, including dorsal rectangular flaps, palmar rectangular flaps, and interdigitating V-flaps (Upton 2006). Many favor the dorsal rectangular flap, as originally described by Flatt, as it is thought to best recreate the natural dorsal to palmar inclination of the web space (Tonkin 2009).
The commissural reconstruction may be altered in an attempt to avoid the need for skin grafts (Fig. 9). In this case, rather than use the typical dorsal rectangular flap or dorsal/volar V-flaps, additional skin is brought into the field to resurface the commissure. The dorsal-metacarpal island flap described by Sherif (Hutchinson and Frenzen 2010; Sherif 1998) includes a dorsal flap centered 0.5–1 cm proximal to the metacarpophalangeal joint that is mobilized on its pedicle and advanced into the commissure. Modifications of this flap design include a rotation of the transposition flap 180° (Aydin and Ozden 2004) or a hexagonal shaped flap (Hsu et al. 2010). The local advancement flap described by Ekerot is a rectangular flap with triangle-shaped wings that form the base and the sides of the commissure, respectively (Ekerot 1996). The triangular wings from the dorsal fingers obviate the need for skin grafting of the proximal fingers adjacent to the commissure.




