Chapter 336 Surgical Conditions of the Anus and Rectum
336.1 Anorectal Malformations
In understanding the spectrum of anorectal anomalies, it is necessary to consider the importance of the sphincter complex, a mass of muscle fibers surrounding the anorectum (Fig. 336-1). This complex is the combination of the puborectalis, levator ani, external and internal sphincters, and the superficial external sphincter muscles, all meeting at the rectum. Anorectal malformations are defined by the relationship of the rectum to this complex and include varying degrees of stenosis to complete atresia. The incidence is 1/3,000 live births. Significant long-term concerns focus on bowel control and urinary and sexual functions.
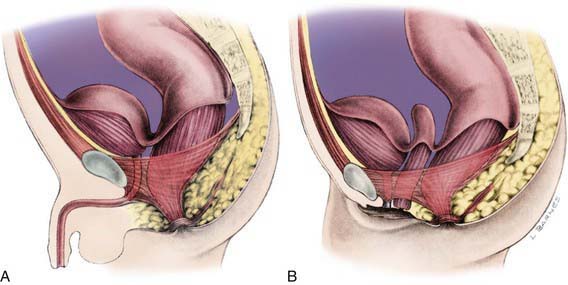
Figure 336-1 Normal anorectal anatomy in relation to pelvic structures. A, Male. B, Female.
(From Peña A: Atlas of surgical management of anorectal malformations, New York, 1989, Springer-Verlag, p 3.)
Embryology
Imperforate anus can be divided into low lesions, where the rectum has descended through the sphincter complex, and high lesions, where it has not. Most patients with imperforate anus have a fistula. There is a spectrum of malformation in boys and girls. In boys, low lesions usually manifest with meconium staining somewhere on the perineum along the median raphe (Fig. 336-2A). Low lesions in girls also manifest as a spectrum from an anus that is only slightly anterior on the perineal body to a fourchette fistula that opens on the moist mucosa of the introitus distal to the hymen (Fig. 336-3A). A high imperforate anus in a boy has no apparent cutaneous opening or fistula, but it usually has a fistula to the urinary tract, either the urethra or the bladder (see Fig. 336-2B). Although there is occasionally a rectovaginal fistula, in girls, high lesions are usually cloacal anomalies in which the rectum, vagina, and urethra all empty into a common channel or cloacal stem of varying length (see Fig. 336-3B). The interesting category of boys with imperforate anus and no fistula occurs mainly in children with trisomy 21.
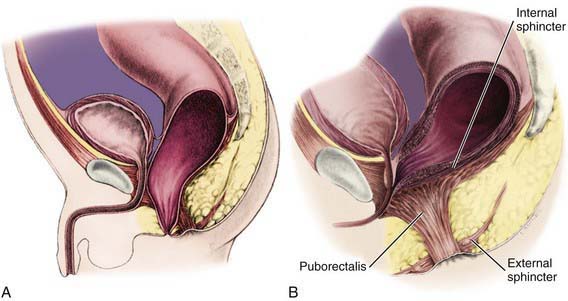
Figure 336-2 Imperforate anus in males. A, Low lesions. B, High lesions.
(From Peña A: Atlas of surgical management of anorectal malformations, New York, 1989, Springer-Verlag, pp 7, 26.)
Associated Anomalies
There are many anomalies associated with anorectal malformations (Table 336-1). The most common are anomalies of the kidneys and urinary tract in conjunction with abnormalities of the sacrum. This complex is often referred to as the caudal regression syndrome. Boys with a rectovesical fistula and patients with a persistent cloaca have a 90% risk of urologic defects. Other common associated anomalies are cardiac anomalies and esophageal atresia with or without tracheoesophageal fistula. These can cluster in any combination in a patient. When combined, they are often accompanied by abnormalities of the radial aspect of the upper extremity and are termed the VATERR (vertebral, anal, tracheal, esophageal, radial, renal) or VACTERL (vertebral, anal, cardiac, tracheal, esophageal, renal, limb) anomalad.
Table 336-1 ASSOCIATED MALFORMATIONS
GENITOURINARY
VERTEBRAL
CARDIOVASCULAR
GASTROINTESTINAL
CENTRAL NERVOUS SYSTEM
Approach to the Patient
Evaluation includes identifying associated anomalies (see Table 336-1). Careful inspection of the perineum is important to determine the presence or absence of a fistula. If the fistula can be seen there, it is a low lesion. The invertogram or upside-down x-ray is of little value, but a prone cross-table lateral plain x-ray at 24 hr of life (to allow time for bowel distention from swallowed air) with a radioopaque marker on the perineum can demonstrate a low lesion by showing the renal gas bubble <1 cm from the perineal skin. A plain x-ray of the entire sacrum, including both iliac wings, is important to identify sacral anomalies and the adequacy of the sacrum. An abdominal-pelvic ultrasound and voiding cystourethrogram (VCUG) must be performed. The clinician should also pass a nasogastric tube to identify esophageal atresia and should obtain an echocardiogram. In boys with a high lesion, the VCUG often identifies the rectourinary fistula. In girls with a high lesion, more invasive evaluation, including vaginogram and endoscopy, is often necessary for careful detailing of the cloacal anomaly.




