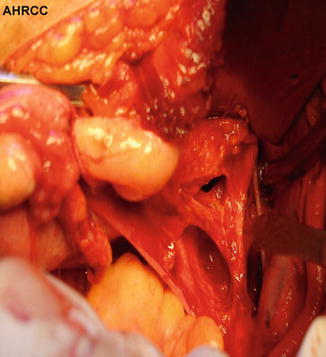
Fig. 13.1
Uterosacral ligaments (AHRCC)
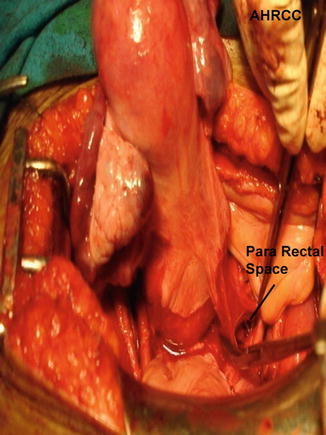
Fig. 13.2
Uterosacral ligaments removed from attachment
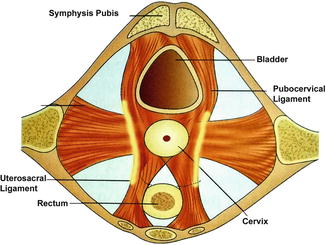
Transverse Cervical (Cardinal/Mackenrodt’s) Ligaments
This serves as the main uterine support. They attach the lateral margins of the cervix and vagina to the pelvic wall. It is important that at the end of hysterectomy, the vault is fixed to these ligaments to prevent future descent of the vault. The cardinal and uterosacral ligaments are simply two parts of a single body of suspensory tissue. It consists mainly of perivascular connective tissue and pelvic vessels.
Though described as extending laterally, these ligaments assume vertical position in erect posture. Each ligament is well defined near the uterine attachment but fans out symmetrically with a broad area of attachment on the second, third, and fourth sacral vertebrae (Figs. 13.3 and 13.4). They help hold the uterus above the levator plate.
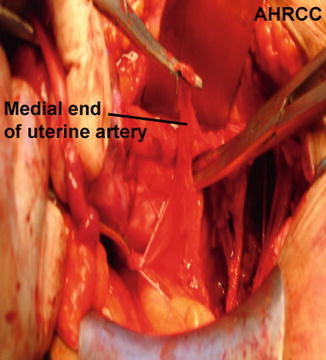
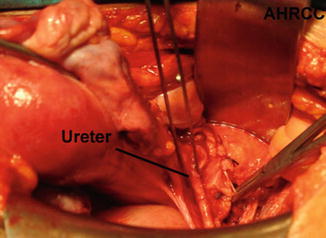
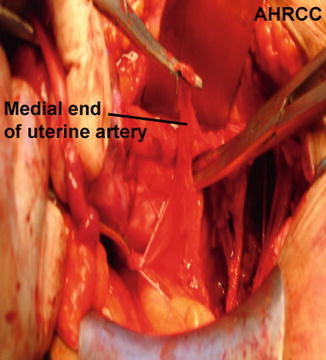
Fig. 13.3
Ureteric tunnel dissection
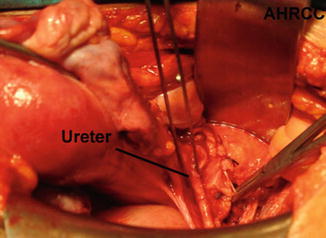
Fig. 13.4
Mackenrodt’s ligament (AHRCC)
The uterosacral and cardinal ligaments provide the greatest support within the pelvis. Fortunately, they are infrequently involved in uterine cancer contrary to cervical cancer where they are frequently involved.
Rectal Pillars
The fibrovascular bundles running from the anterolateral aspects of the rectum to the posterolateral aspect of the vagina are the rectal pillars. They are very vascular and contain the middle rectal arteries, and division may cause unexpected heavy bleeding from the uterine margin. Applying clamps on either side of the division is more esthetic in open surgery.
Bladder Pillars
They are paired fibrovascular bundles that form the lateral limit of the vesicovaginal space. They sometimes are continuous with paracolpos and paravaginal tissue. Condensation of tissue in this area forms the vesicouterine ligament. This houses the ureteric tunnel and is divided into anterior and posterior leaves by the ureter. These two layers have to be dissected off the ureter to visualize its entry into the posterolateral aspect of the bladder [4]. The vesicouterine ligament harbors the cervicovesical veins. Division of these ligaments allows de-roofing of the ureters, and it can be completely mobilized from its attachment to the posterior layer of broad ligament and ureteric tunnel. It is important to know the anatomy of the ureter so that mobilization without ureteric injury is achieved and at the same time preserving its mesentery and vascular supply. The secret to maintaining vascularity of the ureters is to dissect parallel to it and also along the big vessels. The whole purpose of mobilizing the ureter is to place clamps as lateral as required.
Microstructure
Endometrium (Mucosa)
Inside the uterus is a potential triangular cavity lined by endometrium. Endometrium is a unique mucosa. The epithelium is a single-layered columnar and is continuous with tubular uterine glands. The stroma consists of highly cellular connective tissue between endometrial glands and contains blood and lymph vessels. The superficial portion of this layer undergoes cyclic change with the menstrual cycle. Spasm of hormonally sensitive spiral arterioles causes shedding of this layer after each episode of menstruation. A deeper basal layer remains to regenerate a new lining. Separate arteries supply the basal endometrium which explains the preservation of this layer even after shedding.
Myometrium (Smooth Muscle Layer)
The myometrium is fibromuscular in character and makes up most of the uterine corpus. The arrangement of fibers in this layer is complex. This is because the uterus originates from paired paramesonephric primordia, with the fibers from each half crisscrossing diagonally with those of the opposite side. It is composed largely of smooth muscle fascicles mingled with loose connective tissue, blood, and lymph vessels and nerves.
They are arranged in four layers (inner to outer):
1.
Submucosal layer (innermost), composed mostly of longitudinal muscles
2.
Vascular layer, zone rich in blood vessels and longitudinal muscles
3.
Circular muscle layer
4.
Thin longitudinal muscle layer
Serosa
It is composed of peritoneum and covers the uterine body and supravaginal cervix posteriorly and only the uterine body anteriorly.
Microstructure of Cervix
Epithelium
The endocervical canal is lined by columnar secretory epithelium and the ectocervix by stratified squamous nonkeratinizing epithelium. The usual prepubertal location of the squamocolumnar junction is at the external os.
At puberty, the endocervical columnar epithelium responds to estrogenic stimulation and extends distally on the ectocervix. This area of columnar cells on the ectocervix is red and raw in appearance and called ectopy. It is then exposed to acidic environment of the vagina, and through a process of squamous metaplasia, a stratified squamous ectocervical epithelium effectively grows over the exposed area resulting in the transformation zone. Other hyperestrogenic states such as pregnancy and use of oral contraceptive pills can also result in ectopy. This area is the site of epithelial abnormalities that may progress to malignancy. In postmenopausal women, the squamocolumnar junction recedes into the endocervical canal.
Spaces Around the Uterus
Knowledge of spaces around the uterus is an absolute necessity to proceed with any kind of uterine surgery and more importantly radical surgery. Pelvic spaces have been created to help us, surgeons, accomplish adequate surgery without blood loss and injury to vital structures. These spaces have loose areolar tissue and are essentially avascular.
The anterior cul-de-sac separates the bladder from the uterus and the posterior cul-de-sac from the rectum. The loose peritoneum of the anterior cul-de-sac helps in filling the bladder without tension. It is this loose peritoneum that helps to create the space between the bladder and uterus during hysterectomy (Fig. 13.5). Posterior cul-de-sac extends lower as the peritoneum covers the upper part of the vagina, unlike anteriorly, where the vagina is bereft of peritoneum. This has to be kept in mind while opening the peritoneal cavity from below in a vaginal hysterectomy. Specialized dense connective tissue between the rectum and the posterior vaginal wall is called the fascia of Denonvilliers and serves as an important landmark while dissecting the rectovaginal space. While dissecting the rectovaginal space, it is also important to remember that the rectovaginal pad of fat should be kept along with the rectum to prevent inadvertent injury to the rectum.
Fig. 13.5
Division of vesicocervical ligament (AHRCC)
Paravesical Space
These are potential spaces on either side of the bladder. The anterior boundary is the pubic arch that is continuous with the lateral pelvic wall as a lateral boundary. It is bounded medially by the bladder and obliterated umbilical artery and posteriorly by the cardinal ligament (Fig. 13.6).
Pararectal Space
The cardinal ligament forms the anterior border of this space, the medial border is the rectum, and the lateral limit is the pelvic wall. Posteriorly, it is bound by the presacral fascia. The pararectal space is created easily by dissecting in between the ureter medially and the internal iliac artery laterally (Figs. 13.6 and 13.7).
Peritoneal Folds
These ligaments provide no support to the uterus and only consist of folds of peritoneum.
Uterovesical fold.
Rectovaginal fold.
Broad ligament (mesometrium, mesosalpinx, mesovarium). These folds of peritoneum extend laterally from the uterus and cover the adnexal structures.
Infundibulopelvic ligament contains ovarian vessels.
Artery Supply
The uterus is abundantly supplied with blood vessels. Uterine artery, a branch of anterior division of the internal iliac artery, supplies the uterus. It usually arises independently or may rarely have a common origin along with the internal pudendal or vaginal artery. It joins the uterus near the junction of the corpus and cervix but may be variable at times. On reaching the uterus, it divides into an ascending and a descending branch. Using injection micrographic and histologic technique to study the vascular anatomy of the uterus, Farrer-Brown et al. [5] showed that the uterine arteries run a tortuous course between the two layers of the broad ligament along the lateral side of the uterus (Fig. 13.8). They turn laterally at the junction of the uterus and fallopian tube, run toward the hilum of the ovary, and terminate by joining the ovarian arteries. At this point, the artery is closely related to the insertion of the uterosacral ligaments to the uterus. Brisk bleeding ensues on inadvertent injury to the vessels while dividing the uterosacrals from the uterus in a Type I hysterectomy. The ascending branch ascends with a tortuous course in the broad ligament and ends by anastomosing with a branch of ovarian artery. A continuous arterial arcade connects the ovarian, uterine, and vaginal arteries. This is a source of collateral circulation after uterine artery ligation done for postpartum hemorrhage. Accompanying each uterine artery are several large uterine veins. But uterine veins may not accompany the uterine artery always. Bleeding from uterine veins is low in pressure but high in volume. Attempts to take stitches may result in larger avulsions as uterine veins are very thin walled. Vascular clips would be a better alternative.