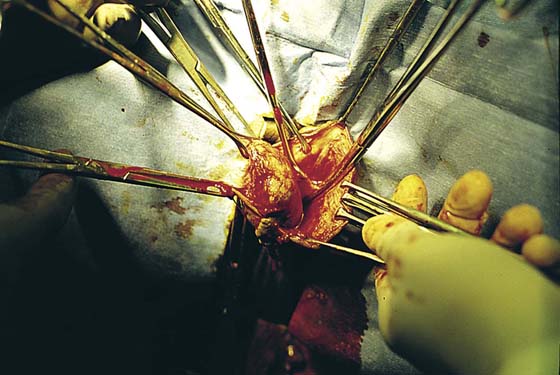
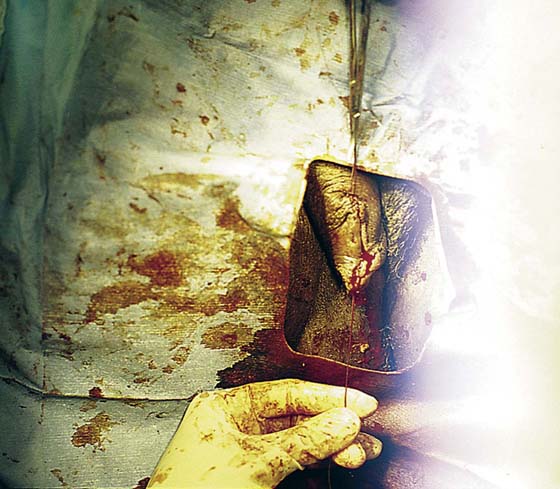
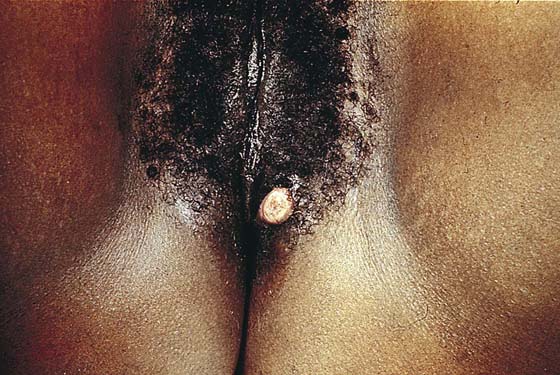
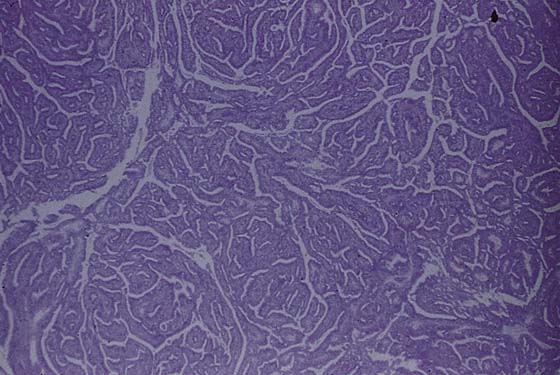
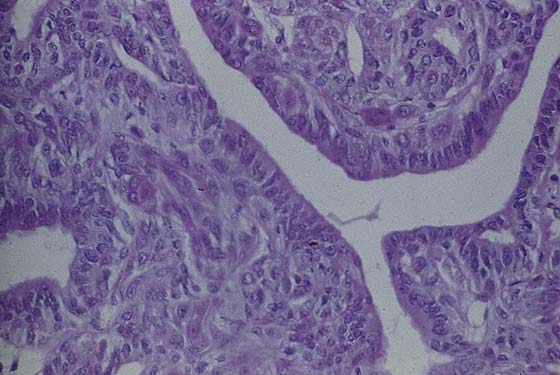
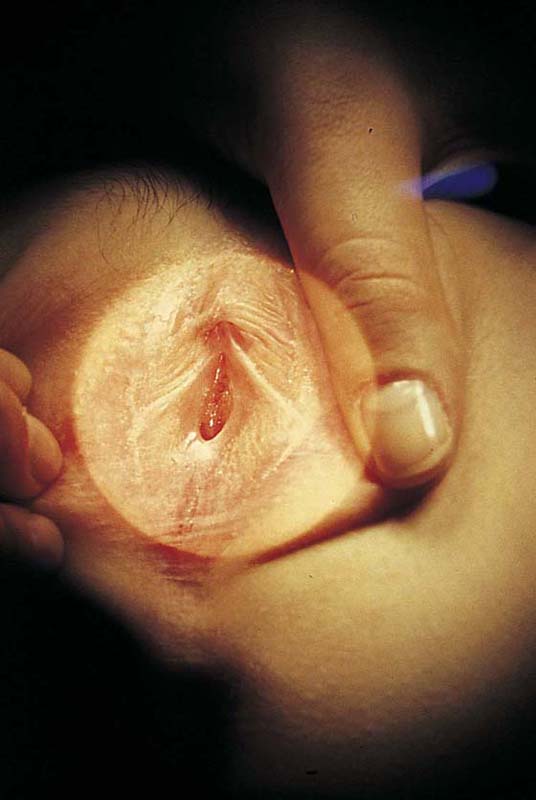
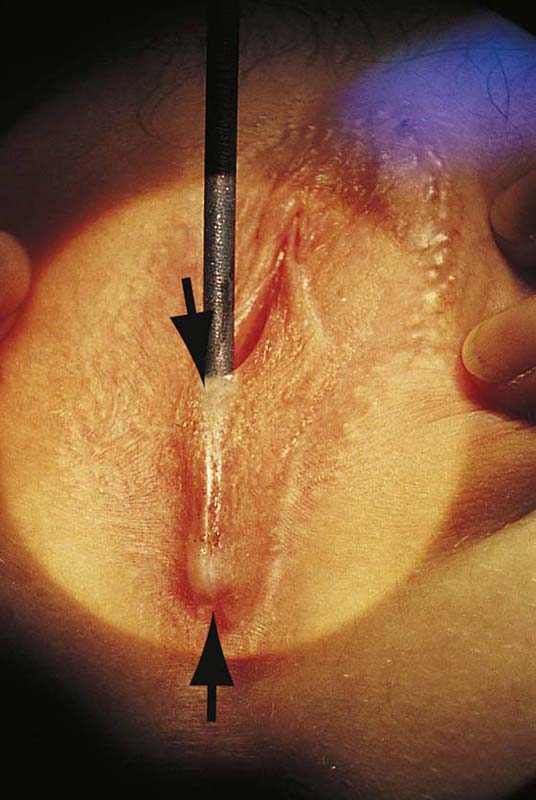
CHAPTER 78 An epidermal inclusion cyst is another name for a sebaceous cyst. They are common wherever hair and sebaceous glands are present (Fig. 78–1). They create a swelling and may be painful to the touch. If they become secondarily infected, they will be associated with cellulitis and may form an actual abscess. The cysts form as a result of blockage of the duct exiting the skin surface from the underlying sebaceous gland or hair follicle. When the duct is obstructed, the fatty secretion of the gland and shed-off squamous cells distend the duct and create the cyst (Fig. 78–2). Initial treatment for an inclusion cyst is the application of hot, wet compresses to the lesion to liquefy the secretion and drain the obstructed duct, with subsequent elimination of the cyst. For recurrent, persistent, or enlarging cysts, the treatment is surgical excision. For cysts 1 cm or smaller, an elliptical incision is made in the skin encompassing the cyst. The incision is carried deeply to circumscribe the cyst and is wedged inward to meet below the cyst. The entire section, including skin, subcutaneous tissue, cyst wall, and contents, is removed en masse. Cysts larger than 1 cm are removed by making a straight-line incision over the mass to the level of the cyst wall beneath the epithelium (Fig. 78–3). The edge of the skin is elevated with Adson-Brown forceps, and the skin margins are dissected away from the cyst wall with Stevens tenotomy scissors. The margins of the skin flaps are then held with Allis clamps for traction, and the cyst wall is completely circumscribed by sharp dissection with the Stevens scissors (Fig. 78–4). The cyst wall should not be grabbed with clamps because this will result in rupture, leakage of contents, and difficulty in extracting the entire cyst (Fig. 78–5). When the entire cyst is freed, it is removed. Excess skin is trimmed, and the wound is closed in layers with 3-0 Vicryl (Fig. 78–6). FIGURE 78–1 Three sebaceous cysts are seen in the hair-bearing area (right labium majus) of the vulva. These common cysts can be simply excised by making an elliptical incision at the base of the cyst and wedging the incision into the subcutaneous tissue. The wound is closed with two or three interrupted 3-0 Vicryl sutures. FIGURE 78–2 This large cyst was very painful and was rapidly increasing in size. The differential diagnosis included a cyst of the canal of Nuck with herniated intestine or fat, as well as a large sebaceous (inclusion) cyst. FIGURE 78–3 An incision is made directly over the mass and is extended to just superior to the mass and to the lower pole of the labium majus. FIGURE 78–4 With Stevens scissors, the mass is separated from the skin margins and flaps are developed. Allis clamps are applied to the skin margins of the flap for traction. The base of the cyst is separated from the connective tissue. The latter is clamped with tonsil clamps for hemostasis. FIGURE 78–5 The cyst is completely excised. From the leaking foul-smelling material, it is identified grossly as a sebaceous cyst. The cyst is placed in fixative and sent to pathology. This usually benign sweat gland tumor creates a smooth, elevated, firm nodularity on the vulvar skin surface (Fig. 78–7). It looks like a firm sebaceous cyst. The tumor is small (i.e., <1 cm). The lesion should be excised by circumscribing an ellipse of skin with a margin of 2 to 3 mm around the mass and extending the incision deeper into the subcutaneous tissue. The skin and tumor are grasped with an Allis clamp, and traction is applied with the use of Stevens scissors. The deep subcutaneous fat is dissected free from the base of the tumor, and the entire small mass of tissue containing the lesion is removed. Histopathologically, the appearance of the tumor under the low-power lens of the microscope is ominous because of the glandular complexity (Fig. 78–8). However, higher-power lens inspection reveals the cells and nuclei to be clearly benign (Fig. 78–9). FIGURE 78–6 The wound is closed in layers with interrupted 3-0 Vicryl sutures. FIGURE 78–7 The hidradenoma is a solid, raised tumor originating in the sweat glands of the vulva. The lesion is fleshy and well circumscribed. It is also painless. The lesion may be excised in a manner identical to that described for sebaceous cysts. FIGURE 78–8 This low-power microscopic section shows a complex glandular proliferation; it appears to be atypical at least and at worst, malignant. FIGURE 78–9 High-power microscopic study reveals well-organized glands and normal cytology. The diagnosis is benign hidradenoma. This problem occurs most commonly in the very young (preadolescent girls) (Fig. 78–10) or the elderly. Once firm fusion has occurred, it is unlikely that the application of topical estrogen will relieve the disorder. Surgical separation is usually required. The line of fusion must be accurately identified. This is accomplished with the aid of a magnifying loupe or an operating microscope. A small probe may be placed in the artificial pouch created by the fusion (i.e., the probe is placed behind [deep to] the fused labia). Pressure is exerted outward to stretch the surface of the labia; this in turn helps to identify the points of original fusion. A knife (No. 15 blade) cuts the stretched skin over the probe and down to the probe (Fig. 78–11). After the labia are separated, the edges are closed with a continuous 4-0 polydioxanone (PDS) suture on either side (Fig. 78–12). The suture line is covered with a topical estrogen cream, which is reapplied 2 or 3 times per day during the postoperative and recovery periods. FIGURE 78–10 This adolescent girl demonstrates fusion of the labia minora. FIGURE 78–11 A probe has been placed within the pocket created by the fusion. The arrows show the direction of the incision that will be made over the probe (i.e., with the probe used as a backstop). FIGURE 78–12 An incision is made with a carbon dioxide (CO2) laser; however, the same cut may be made with a scalpel. The edges are closed with a running 4-0 polydioxanone (PDS) suture. The wound is covered with topical estrogen to keep the respective edges from agglutinating. Draining vulvar lesions cause a variety of pathologies, including venereal lesions and sinus tracts (Fig. 78–13). Although the first, nonsurgical approach consists of culture of the drainage for a variety of microorganisms (including fungi), diagnosis may be difficult. Drainage points should be explored with the use of lachrymal probes to determine whether a tract exists and where it goes. If a tract is identified, radiologic examination may be helpful in identifying a possible fistula. In this case, the patient should be scheduled for fluoroscopy. A small-gauge vascular catheter is engaged into the sinus opening and is manipulated through the tract. Water-soluble dye is injected during real-time fluoroscopic examination to determine whether a connection with the intestine or another structure exists. If no fistulous tract is demonstrated and no diagnosis has been made on the culture, then a wide and deep excision of the lesion should be performed (Fig. 78–14). The patient is given a general anesthetic and is placed in the lithotomy position, the skin is prepared, and the operative field is draped. A skin pen is used to mark the boundaries for the excision. The traced area is shallowly circumscribed with a knife (No. 15 scalpel). The cut is extended more deeply into the fat, and the wound edges are grasped with Allis clamps for traction. A wedge-shaped incision is completed on all sides of the lesion margins, and the mass is removed. Tissue samples are placed in sterile containers to be cultured. Special stains are ordered for the pathologic specimen, including Giemsa, silver, acid-fast, and fungal stains. Draining wounds occurring in immigrants from developing countries should carry a high index of suspicion for tuberculosis (Fig. 78–15 through 78–17). If initial probing reveals a sinus tract to the gastrointestinal tract (e.g., to the anus), then before excision, the patient must undergo a bowel prep (Fig. 78–18). The author recommends the following: 1. Three days before surgery: Begin a low-residue diet. 2. Two days before surgery: Begin a full liquid diet. 3. The day before surgery: Start a clear liquid diet, and take the following medications: neomycin 1 g by mouth at 11 AM, 12 PM, and 6 PM; metronidazole 500 mg by mouth at 11 AM, 12 PM, and 6 PM; Fleets Phospho-Soda 2.5 oz mixed with 4 oz of clear liquid (7-Up, lemonade, or water), followed by eight glasses of water to be completed by 1 PM; and metoclopramide (Reglan) 10 mg, one by mouth every 6 hours starting at 8 AM
Surgery for Other Benign Lesions of the Vulva
Inclusion Cyst
Hidradenoma
Labial Fusion
Draining Vulvar Lesions
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree