Suprarenal Mass
Alexander J. Towbin, MD
DIFFERENTIAL DIAGNOSIS
Common
Normal Adrenal Hypertrophy of Neonate
Neuroblastoma
Less Common
Adrenal Hemorrhage
Pulmonary Sequestration
Ganglioneuroma
Ganglioneuroblastoma
Rare but Important
Adrenal Carcinoma
Adrenal Adenoma
Congenital Adrenal Hyperplasia
Pheochromocytoma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Adrenal masses are usually malignant
DDx for suprarenal mass in fetus or neonate
Neuroblastoma, adrenal hemorrhage, or pulmonary sequestration
Helpful Clues for Common Diagnoses
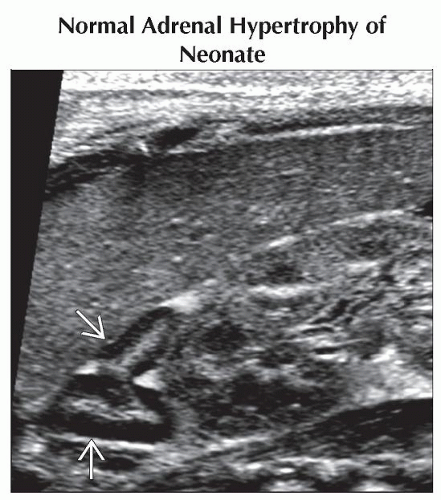
Normal Adrenal Hypertrophy of Neonate
At birth, normal adrenal is 10-20x larger than adult gland relative to body weight
˜ 1/3 size of neonatal kidney
Consists mostly of cortical tissue
Gland decreases in size over 1st 2 weeks
Thick hypoechoic outer layer and echogenic core on US
Neuroblastoma
Most common solid extracranial malignancy
6-10% of all childhood cancers
15% of pediatric cancer deaths
4th most common pediatric malignancy after leukemia, CNS tumors, and lymphoma
2nd most common abdominal neoplasm after Wilms tumor
> 90% of patients diagnosed before age 5
Median age at diagnosis is 22 months
Peak incidence in 1st year of life (30%)
Most common malignancy in 1st month of life
Almost always adrenal in origin (90%)
Metastases to liver, bone marrow, and skin present at diagnosis (50%)
Good prognosis: > 90% survival rate
Can arise anywhere along sympathetic chain
˜ 70% originate in retroperitoneum
35% in adrenal medulla
30-35% in extraadrenal paraspinal ganglia
Mediastinum is 3rd most common location (20%)
Patients < 1 year have better prognosis
Abdominal mass is most common presentation
Can present with bruising around eyes
Paraneoplastic syndromes in ˜ 2%
50% have metastases at diagnosis
Most common to liver, bone, and bone marrow
Hepatic metastases can be diffuse or nodular
Calcifications present in ˜ 85% of tumors
I-123 MIBG uptake in 90-95% of patients
MR is useful to see intraspinal involvement
Prognosis varies depending on stage
Staged by International Neuroblastoma Staging System
Helpful Clues for Less Common Diagnoses
Adrenal Hemorrhage
Multiple causes, including neonatal asphyxia, perinatal stress, trauma, septicemia, coagulopathies, and Henoch-Schönlein purpura
Bilateral hemorrhage in 10%
When unilateral, R > L
Can be asymptomatic or life-threatening
US: Initially appears as hyperechoic mass
Liquefies by 2-3 days; becomes anechoic
CT: Usually seen in setting of trauma
Associated with ipsilateral abdominal and thoracic injuries
Can eventually calcify
Pulmonary Sequestration
Congenital anomaly
Nonfunctioning pulmonary tissue
No connection to tracheobronchial tree
Systemic arterial supply
Intralobar: Sequestered lung adjacent to normal lung
Extralobar: Sequestered lung with separate pleural covering
Ganglioneuroma
Well-differentiated, benign form of neuroblastoma
Neuroblastoma or ganglioneuroblastoma can mature to ganglioneuroma
Most common in stage 4S tumors
Median age at diagnosis is 7 years
Most common in mediastinum, retroperitoneum, and adrenal gland
Ganglioneuroblastoma
Intermediate-grade tumor between ganglioneuroma and neuroblastoma
Seen in similar locations as neuroblastoma
Has malignant potential
Helpful Clues for Rare Diagnoses
Adrenal Carcinoma
< 1% of pediatric malignancies
More common in females
Usually occurs before age 6
Most are hormonally active
Usually present with virilization in girls and pseudoprecocious puberty in boys
Associated with hemihypertrophy, brain neoplasms, and hamartomas
Tumors are usually large at presentation
Difficult to differentiate from adenoma
Helpful criteria include size > 5 cm, invasion of inferior vena cava, and metastases
Metastasizes to lung, liver, lymph nodes, and inferior vena cava
Adrenal Adenoma
Rare in children
3x less common than adrenal carcinomas
Most are hormonally active
Cushing syndrome most common
Often have high lipid content and lose signal on out-of-phase MR imaging
Congenital Adrenal Hyperplasia
Autosomal recessive error of metabolism
Infants present with salt-wasting
Can be virilization of females
On US, adrenal measures > 20 mm in length or 4 mm in width
Adrenals may have wrinkled or cerebriform contour
Pheochromocytoma
10-20% of pheochromocytomas occur in children
Presents with sustained hypertension
Accounts for ˜ 1% of hypertension in children
Associated with von Hippel-Lindau, MEN type 2, and neurofibromatosis type 1
50-85% arise in adrenal medulla
Bilateral pheochromocytomas in 18-38%
Appear extremely hyperintense on T2
Malignant pheochromocytomas are less common than in adults
Metastasize to bone, liver, lymph nodes, and lungs
I-123 MIBG is sensitive and specific
Image Gallery
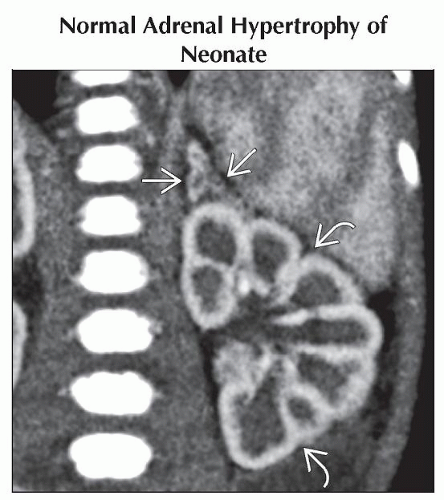 Coronal CECT shows a prominent left adrenal gland
 with an enhancing cortex and hypodense core. There is fetal lobulation of the left kidney with an enhancing cortex and hypodense core. There is fetal lobulation of the left kidney  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|