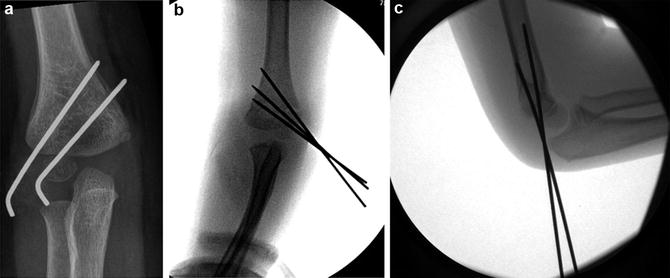
Fig. 1
Lateral view of the distal humerus. Note the thin bone separating the coronoid fossa (anterior) from the olecranon fossa (posterior) (Courtesy of Shriners Hospital for Children, Philadelphia)
Depending on the direction of displacement of the distal humerus fragment, supracondylar fractures can be classified into extension and flexion types. Extension-type fractures account for 97–99 % of all supracondylar humerus fractures (Mahan et al. 2007) and are usually due to a fall on an outstretched hand with the elbow in full extension. A typical injury mechanism is a fall from playground equipment onto the non-dominant hand (usually the left) with the elbow in hyperextension to brace the fall. In this type of injury, the distal fragment is displaced posteriorly, thus leading to an extension-type fracture. In contrast, flexion-type supracondylar fractures are most commonly caused by a direct blow to the elbow with the arm in flexion. In this scenario, the distal fragment is displaced anteriorly. Flexion-type supracondylar fractures are rare and therefore have not been as extensively characterized as extension-type fractures.
In extension-type supracondylar fractures, the elbow is locked in hyperextension, which engages the olecranon in the olecranon fossa of the posterior humerus. Linear forces transmitted to the anterior capsule provide bending forces against the olecranon, which now serves as a fulcrum. In this type of supracondylar fracture, the proximal segment is often displaced anteriorly, and the anterior periosteum is almost always torn (Skaggs and Flynn 2010). The distal fragment can be either displaced posteromedially (in 75 % of cases) or posterolaterally. This distinction of direction has implications for whether the arm should be pronated during reduction. In posteromedially displaced fractures, the medial periosteum remains intact. Applying tension on medial periosteum with the forearm pronated closes this hinge corrects valgus malalignment and stabilizes the fracture.


Fig. 2
An anterior pucker sign may be present if proximal fracture segment penetrates the brachialis muscle and other soft tissues
In contrast, posterolaterally displaced fractures have a torn medial periosteum. Pronation will further destabilize these fractures; thus, supination is better at aiding in reduction. The key take home point is that not all extension-type supracondylar fractures should be reduced with the forearm pronated.
In Gartland type IV fractures, both the anterior and posterior periosteum are disrupted. These fractures are unstable in both extension and flexion and require a different management.
Assessment of Supracondylar Humerus Fracture
Signs and Symptoms of Supracondylar Humerus Fracture
The child with a supracondylar fracture typically complains of elbow pain, swelling, and restricted range of motion at the elbow following a traumatic event, most often a fall onto the outstretched arm (Baratz et al. 2006). When evaluating the patient, the entire upper extremity should be examined thoroughly and assessed for concomitant fractures, such as forearm fractures, as they can occur in association with supracondylar fractures and greatly increase the risk of compartment syndrome (Blakemore et al. 2000). Soft-tissue swelling, ecchymosis and skin puckering (Fig. 2) suggest a more severe fracture pattern with the associated possibility of a neurovascular injury (Omid 2008).


Fig. 3
A posterior fat pad sign may be the only evidence of a nondisplaced supracondylar fracture
A thorough neurologic exam must be performed because of the high prevalence of neurologic injury in association with supracondylar fractures. Sensation should be tested in children old enough to comply with the exam, typically 8 years of age or older. The sensory distribution of the radial nerve (first dorsal digital space), median nerve (palm of the first three digits) and ulnar nerve (ulnar side of little finger) should be assessed. The motor exam should assess function of the radial nerve (finger metacarpophalangeal (MP) extension and wrist extension), anterior interosseous nerve (distal interphalangeal (DIP) joint of the index/long finger and thumb interphalangeal joint flexion), median nerve (proximal interphalangeal (PIP) joint finger flexion), and ulnar nerve (abduction and adduction of the digits).
It is essential to assess the vascular status as the prevalence of displaced supracondylar fractures presenting with vascular compromise has been reported to be as high as 20 % (Pirone et al. 1988; Campbell et al. 1995). The vascular status is categorized as present pulses with a warm hand, pulseless with a warm hand, and pulseless with a cold hand (Skaggs and Flynn 2010).
Supracondylar Humerus Fracture Imaging and Other Diagnostic Studies
Standard radiographs for supracondylar humerus fracture evaluation should include anteroposterior (AP) of the distal humerus (not an AP of the elbow) and a true lateral of the elbow in anatomic position. Oblique views are not routinely required but can be obtained for comparison to the uninvolved elbow in order to detect minimally displaced fractures. Computed tomography (CT) scan and magnetic resonance imaging (MRI) are not routinely used.
In radiographic evaluation of supracondylar humeral fractures, three key parameters should be assessed: (a) presence of a posterior fat pad sign (which may be the only sign of a supracondylar humerus fracture and thus should not be missed) (Skaggs and Mirzayan 1999); (b) location of the anterior humeral line (AHL) in relation to the capitellum; and (c) measurement of Baumann’s angle. The AHL is drawn down along the anterior humeral cortex (Herman et al. 2009) and should intersect through the middle third of the capitellum except in children younger than 4 years of age, where it may intersect the anterior third (Herman et al. 2009; see Figs. 3, 4, 5, and 6).
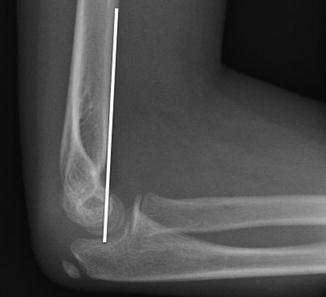

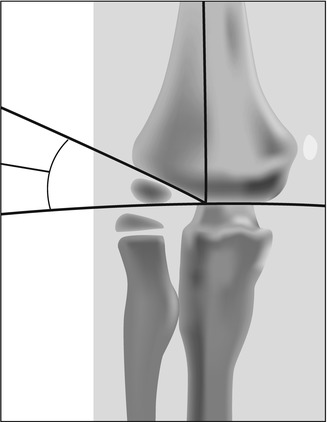

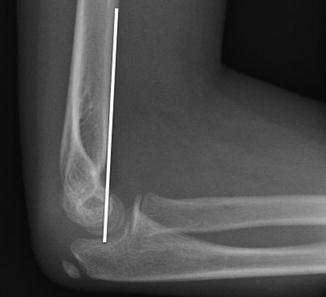
Fig. 4
The anterior humeral line (AHL) should intersect the capitellum in a normal elbow

Fig. 5
In a displaced supracondylar humerus fracture, the AHL is anterior to the capitellum
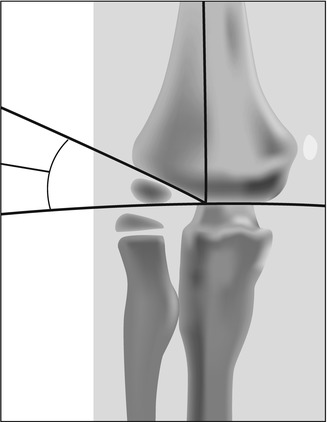
Fig. 6
The Baumann’s angle is usually >10°

Fig. 7
Gartland type I fracture with posterior fat pad sign and subtle cortical irregularity
In displaced extension-type fractures, the AHL is usually anterior to the capitellum. The Baumann’s angle, which is the angle between the long axis of the humeral shaft and the physeal line of the lateral condyle, should be ≥10°. Baumann’s angle <9° signifies a fracture in varus angulation.
Supracondylar Humerus Fracture Classification
Several classification systems exist for supracondylar fractures; however, the modified Gartland system is the most widely used (Omid 2008; Abzug and Herman 2012; Howard et al. 2012; Gartland 1959). The Gartland system categorizes extension-type supracondylar fractures into three types: Type I is a nondisplaced or minimally displaced (<2 mm) supracondylar fracture with an intact AHL. In Gartland type I supracondylar fractures, often a posterior fat pad sign is the only evidence of fracture (Fig. 7).


Fig. 8
Gartland type II supracondylar fracture. Note that the capitellum is posterior to the AHL, indicating that closed reduction and pinning is indicated
Gartland type II supracondylar fractures are displaced (>2 mm) with an intact, hinged, posterior periosteum (Fig. 8). In this fracture type, the AHL is often anterior to the capitellum, but in some mildly displaced cases, it just abuts it. Modifications by Wilkins (1984) further subdivide type II fractures into subtypes A and B. Type IIA fractures are angulated posteriorly but lack rotational deformity. These fractures are often stable after flexion reduction and in some rare cases can be managed with nonoperatively with casting, as long as the fracture is completely stable and remains reduced while casted at 80–90°. Type IIB fractures still retain an intact posterior hinge but have some degree of rotational displacement. These fractures are generally unstable after reduction and require fixation with Kirschner wires (K-wires). In, Gartland type III, there is complete displacement without any hinge and there is usually a rotational deformity in the frontal and transverse planes (Fig. 9). A fourth type has been recently classified by Leitch et al. for fractures that are unstable in both flexion and extension (Table 1).



Fig. 9
In Gartland type III, there is complete displacement without any meaningful cortical contact
Table 1
Gartland classification | AHL relationship to capitellum | Cortex intact? | Recommended treatment |
|---|---|---|---|
Stability? | |||
Type I | AHL intersects center of capitellum | Cortex intact circumferentially | Long arm cast immobilization 3 weeks |
Type IIa | AHL anterior to capitellum | Posterior cortex intact, stable | Generally closed reduction and pinning, but some can be treated with cast immobilization for 3 weeks |
Type IIb | AHL anterior to capitellum | Posterior cortex intact, rotational instability | Closed reduction with pin fixation |
Type III | AHL anterior to capitellum | No intact cortex, unstable in extension | Closed reduction with pin fixation |
Type IV | AHL anterior or posterior to capitellum | No intact cortex | Closed reduction with pin fixation |
Unstable in extension and flexion |

Fig. 10
Patient is supine on the operating table and fluoroscopy unit monitor is on the opposite side of the surgeon
Supracondylar Humerus Fracture Outcome Tools
No outcome tools exist specifically for supracondylar humerus fractures.
Supracondylar Humerus Fracture Treatment Options
Initial management of displaced supracondylar fractures involves elbow splinting at approximately 20–40° of flexion with avoidance of tight bandaging. This position prevents vascular compromise that may occur with excessive flexion (Mapes and Hennrikus 1998; Battaglia et al. 2002). Upon arrival in the emergency department, a careful and thorough physical exam should be undertaken, followed by definitive fracture treatment, most commonly with closed reduction and percutaneous pin fixation. Other treatment options include simple immobilization for nondisplaced/minimally displaced Gartland type I fractures and open reduction and pin fixation in cases of failed closed reduction and open fractures.
Nonoperative Management of Supracondylar Humerus Fracture
The nonoperative treatment of type I fractures involves short-term simple immobilization followed by range of motion exercises. The indication for nonoperative treatment of supracondylar fractures is a Gartland type I (nondisplaced or minimally displaced <2 mm) supracondylar fracture without evidence of nerve injury or instability. The decision regarding nonoperative treatment is greatly enhanced by assessment of the AHL. If, on the initial presentation film, the AHL intersects the capitellum ossification center, then the fracture is defined as minimally displaced, and cast immobilization alone is the recommended treatment (Skaggs and Flynn 2010). The orthopedic surgeon should also assure that on the AP x-ray, there is not excessive medial impaction that could cause cubitus varus. Baumann’s angle should be assessed and be in the acceptable range.
Indications/Contraindications
The indication for nonoperative treatment of supracondylar humerus fractures is a Gartland type I supracondylar fracture.
Supracondylar humerus fracture | |
|---|---|
Nonoperative management | |
Indications | Contraindications |
Gartland type I fracture – AHL transects the capitellum on lateral radiograph | Displaced fractures in which the AHL is anterior to capitellum |
The Baumann angle is >10° on affected side | Open fractures |
Techniques
The patient is initially treated with a long arm cast with the elbow flexed 80–90° for 3 weeks, followed by range of motion exercises (Williamson and Cole 1993; Charnley 1961; Cuomo et al. 2012). At the completion of immobilization, patients can begin active range of motion exercises and will often not require physical therapy. A return visit for a range of motion check at 4–6 weeks post immobilization is typically offered.
Supracondylar humerus fracture | |
|---|---|
Nonoperative management | |
Elbow is casted for approximately 3 weeks at 80–90° of flexion followed by an active range of motion program. Return to all activities is allowed when the patient is asymptomatic |
Outcomes
Nondisplaced/minimally displaced supracondylar fractures treated with simple immobilization have universally excellent outcomes. In a recent study, Cuomo and associates reviewed 53 patients with Gartland type I fractures and found intact AHL and Baumann’s angle >9° at 3 weeks follow-up after treatment with only splint immobilization (Cuomo et al. 2012). Ballal et al. (2008) also reported excellent outcomes in all subjects in their series of 40 patients.
Operative Treatment of Supracondylar Humerus Fracture
Operative treatment consists of either closed reduction with pin fixation or, in rare circumstances, open reduction with pin fixation.
Closed Reduction and Percutaneous Pinning of Supracondylar Humerus Fracture
Indications/Contraindications
Closed reduction with pin fixation (CRPF) is the preferred treatment for Gartland type II, III, and IV supracondylar fractures. Indications for CRPF are (1) a displaced fragment in which the capitellum is posterior to the anterior humeral line and (2) minimally displaced fragments with medial column comminution or any malalignment in the coronal plane, making Baumann’s angle in the unacceptable range. Contraindications for closed reduction with fixation are (1) open fractures, (2) failed closed reduction, and (3) a limb that remains dysvascular after CRPF. These patients should undergo an immediate open reduction (Table 1).
Supracondylar humerus fracture | |
|---|---|
Closed reduction and pin fixation | |
Indications | Contraindications |
Displaced (Gartland type II–IV) fractures | Nondisplaced or minimally displaced fractures |
Fractures with medial column comminution | Open fractures requiring debridement |
Fractures with coronal plane malalignment | |
Surgical Procedure: Closed Reduction
Preoperative Planning
Reduction and fixation of a supracondylar fracture is generally an urgent issue, with treatment in the first 24 h after injury. In circumstances when there is either poor perfusion to the hand or in severe fractures with median nerve injury, these fractures are reduced and fixed emergently (Abzug and Herman 2012).
Closed reduction and percutaneous for supracondylar humerus fracture |
|---|
Preoperative planning |
OR Table: standard |
Position/positioning aids: Supine/radiolucent arm board |
Fluoroscopy location: On same side as the surgeon; place monitor on opposite side for easy viewing |
Equipment: Basic orthopedic set, K-wires, K-wire driver |
Positioning
Supine with the C arm parallel to the table and on the same side as the injured arm. For ease of viewing by the surgeon, the fluoroscopy unit monitor should be placed on the other side of the bed, opposite the surgeon (Fig. 10).


Fig. 11
(a) Jones view of the elbow after closed reduction; (b) to obtain this view, the elbow is maximally flexed with the forearm pronated. The image is obtained by directing the radiographic tube perpendicular to the distal elbow in an anterior to posterior direction
In children less than 3 years of age, a radiolucent hand table is valuable because the upper arm is not long enough to bring the elbow to the center of the image intensifier. Additionally, in very unstable fractures, such as Gartland type IV fractures, the radiolucent hand table is also valuable so that the image intensifier can be rotated to get a lateral x-ray.
Surgical Approach
After prophylactic antibiotics and endotracheal intubation, the injured hand, forearm, elbow, and arm are prepped and draped up to the shoulder. In type II fractures or moderate type III fractures, reduction is performed by gentle longitudinal realignment and then flexion. In severe type III fractures, gentle massaging of the brachialis and biceps is performed first, in order to free the metaphyseal fragment. This “brachialis milking” technique should be done with patience, and if done skillfully will avoid many unnecessary open reductions. Next, reduction in the sagittal plane should be attempted by slowly flexing the elbow with the non-dominant hand and at the same time pushing forward on the olecranon with the thumb of the dominant hand. Satisfactory reduction can be assessed by flexing the child’s elbow to see if the fingers can touch the shoulder. If the reduction is unsuccessful, the patient will be unable to do so.