Splenic Mass
Daniel J. Podberesky, MD
DIFFERENTIAL DIAGNOSIS
Common
Perfusion Artifact
Trauma
Granulomatous Disease
Lymphoma
Acquired Cyst
Hematoma
Infarction
Infection and Abscess
Less Common
Congenital Cyst
Metastases
Primary Tumor
Rare but Important
Post-Transplant Lymphoproliferative Disease
Lymphatic Malformation
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Primary and metastatic splenic malignancies are rare in children, except for lymphoma and leukemia
Clinical history is crucial as many splenic lesions have similar imaging characteristics
Is child immunocompromised?
Is there known primary neoplasm?
Does patient have sickle cell disease or other hemoglobinopathy?
Is there history of trauma?
Helpful Clues for Common Diagnoses
Perfusion Artifact
Seen during arterial phase of CT and MR
Patterns include striped, focal, and diffuse heterogeneity
Ultrasound helpful in difficult cases
Hint: Resolves on delayed phase imaging (> 70 sec)
Trauma
Trauma history is helpful
Laceration, fracture, rupture all possible
Splenic injury more common when spleen is enlarged, i.e., with infectious mononucleosis
Active bleeding manifests as foci of high attenuation
American Association for the Surgery of Trauma grading system
Grade 1: Subcapsular hematoma, < 10% surface area OR < 1 cm deep laceration
Grade 2: Subcapsular hematoma, 10-50% surface area OR 1-3 cm laceration not involving parenchymal vessel
Grade 3: Subcapsular hematoma, > 50% surface area or expanding/ruptured, OR parenchymal hematoma > 5 cm OR laceration > 3 cm
Grade 4: Laceration of vessel producing devascularization of > 25% of spleen
Grade 5: Shattered spleen OR hilar vascular injury
Granulomatous Disease
Old granulomatous disease (such as histoplasmosis) frequently demonstrates small calcified splenic lesions
Wegener granulomatosis may involve spleen
Sarcoidosis may involve spleen
Lymphoma
Hodgkin or non-Hodgkin lymphoma can involve spleen
Focal lesions or diffuse involvement
Typically hypoattenuating on CT and hypoechoic on US
Hint: Look for associated lymphadenopathy
Acquired Cyst
Pseudocysts (lack epithelial lining)
Typically result from prior trauma, infarct, or infection
Differentiation by imaging from congenital cyst not reliable
Hematoma
Typically secondary to trauma
May be parenchymal or subcapsular
May lead to acquired splenic cyst
Infarction
Secondary to occlusion of noncommunicating end arteries of spleen
Commonly seen in children with hemoglobinopathies, such as sickle cell disease, and malignancies
Variable appearance depending on stage
Early: Ill-defined mottled changes in density on CT or echogenicity on US
Late: Well-defined peripheral hypoechoic or hypodense wedge-shaped regions
May resolve completely or evolve into acquired cyst
Infection and Abscess
Fungal and bacterial infections occur most frequently in immunocompromised patients
Fungal splenic abscesses are hypodense and typically small
Hint: Look for lesions in liver, kidneys, and lungs as well
Hydatid abscesses are rare
Helpful Clues for Less Common Diagnoses
Congenital Cyst
True cyst (epithelial lining)
Includes epidermoid cysts and mesothelial cysts
Differentiation by imaging from acquired cyst not reliable
Metastases
Splenic metastases are rare
Hint: Look for metastases in other visceral organs
Melanoma
Variable imaging appearance
Typically hypoechoic/hypodense relative to normal spleen
Can see cystic splenic metastases
Primary Tumor
Malignant
Majority lymphoma and leukemia
Benign hamartoma
Nonneoplastic mixture of normal splenic components
Can be seen in tuberous sclerosis patients with hamartomas in other organs
Nonspecific imaging appearance, occasionally with calcifications
Benign hemangioma
Most common primary splenic neoplasm
Can be solitary or multiple
Can cause Kasabach-Merritt syndrome (thrombocytopenia and consumptive coagulopathy)
Variable imaging appearance
Helpful Clues for Rare Diagnoses
Post-Transplant Lymphoproliferative Disease
Complication of solid organ transplant and allogeneic bone marrow transplant
Associated with EBV infection
Spleen involved in ˜ 20% of cases
Similar imaging appearance to lymphoma
Hint: Look for involvement of other organs
Lymph nodes
Liver
Lung
CNS
Lymphatic Malformation
Nonneoplastic endothelial-lined lymph channels
Septate cystic lesions most commonly
May contain debris or fluid-fluid levels
Septa and rim typically enhance
Image Gallery
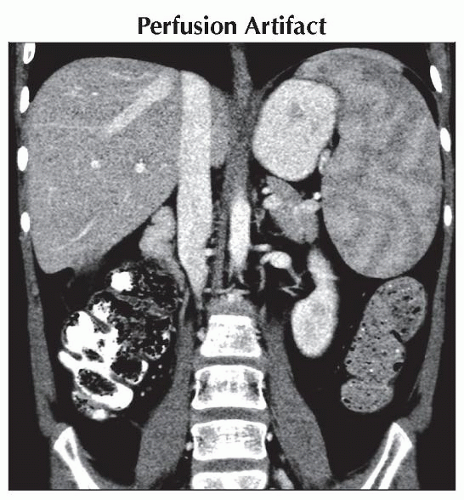 Coronal CECT shows heterogeneous stripes of low attenuation in the spleen, a common normal variant seen during arterial phase imaging. This pattern has been referred to as “tiger” or “zebra” striped. |
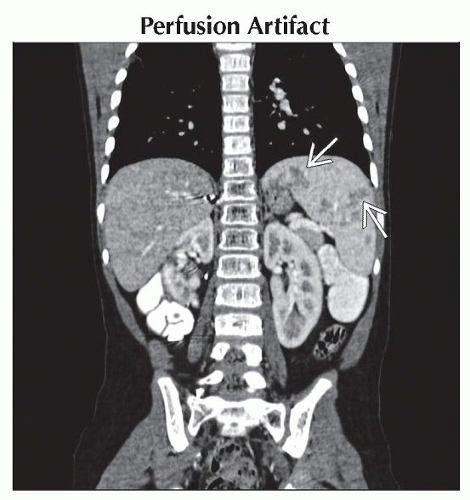 Axial CECT shows multifocal areas of decreased attenuation of the spleen
 that proved to be normal variant heterogeneous enhancement. This appearance resolved on portal venous phase imaging. that proved to be normal variant heterogeneous enhancement. This appearance resolved on portal venous phase imaging.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|