Small Bowel Obstruction
Eva Ilse Rubio, MD
DIFFERENTIAL DIAGNOSIS
Common
Appendicitis
Adhesions
Ileocolic Intussusception
Midgut Volvulus
Inflammatory Bowel Disease (Crohn Disease)
Incarcerated Inguinal Hernia
Less Common
Hirschsprung Disease
Meconium Plug Syndrome (Small Left Colon Syndrome)
Meckel Diverticulum
Jejunoileal Atresia
Meconium Ileus
Gastrointestinal Duplication Cysts
Rare but Important
Distal Intestinal Obstructive Syndrome
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
In neonates, differentiate between high (proximal) and low (distal) obstruction
Common causes of proximal obstruction
Malrotation/midgut volvulus
Duodenal atresia
Duodenal stenosis/web
Diagnostic work-up starts with upper GI
Common causes of mid-bowel obstruction
Jejunal atresia/web
Volvulus ± malrotation
Diagnostic work-up usually involves upper GI and contrast enema
Low (distal) obstruction
Hirschsprung disease
Meconium plug syndrome (small left colon syndrome)
Ileal atresia
Meconium ileus
Work-up starts with contrast enema
Common differential considerations for obstruction in older children
Appendicitis
Adhesions
Intussusception
Incarcerated inguinal hernia
Inflammatory bowel disease
Meckel diverticulum
Helpful Clues for Common Diagnoses
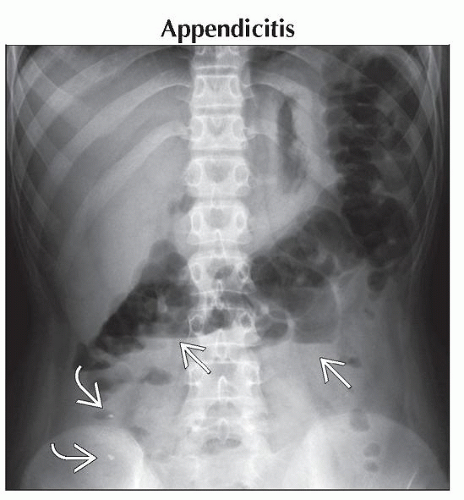
Appendicitis
Radiograph
Appendicitis should be considered with appendicolith on plain film
Classic small bowel obstruction is common presentation: Dilated loops, multiple air-fluid levels on upright or decubitus views
Early appendicitis may be subtle with distal bowel gas and stool, scattered air in small bowel
Ultrasound
Iliac artery/vein useful landmark for locating appendix, which often lies near/over vessels
Noncompressible blind-ending tube, ≥ 7 mm diameter, echogenic periappendiceal fat
If significant amount of free intraperitoneal fluid, suspect perforation
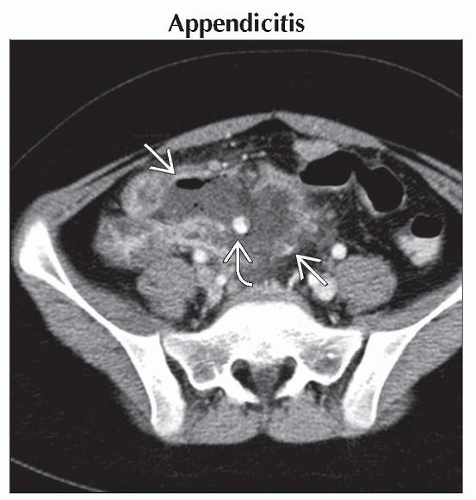
CT
Inflamed, hyperemic tubular structure; does not fill with oral contrast
Look for signs of longstanding/perforated appendicitis: Free fluid, free air, inflammatory phlegmon
Adhesions
Almost never directly visualized; diagnosis made intraoperatively
Wide range of severity on any modality (radiograph, CT, US)
Nonspecific increased small bowel air with fluid levels, distal bowel gas if mild/partial/intermittent obstruction
Dilated small bowel loops, absent distal gas, air-fluid levels if high-grade or complete obstruction
Ileocolic Intussusception
Majority of cases occur between age 3 months to 3 years
If well outside this age range or recurrent, consider pathologic lead point
Radiograph
Bowel gas pattern ranges from nonspecific to frank obstruction
Intussusceptum may be identifiable as right lower quadrant soft tissue density
Ultrasound is sensitive and specific tool to confirm or exclude intussusception
Alternating hypo-/hyperechoic rings
Midgut Volvulus
Must be excluded in patients with bilious emesis
Bowel gas pattern ranges from nonspecific/normal to ominously dilated loops of proximal bowel with paucity of distal bowel gas
Inflammatory Bowel Disease (Crohn Disease)
Findings may manifest anywhere from mouth to anus
CT
Segmental, circumferentially thickened bowel wall with luminal narrowing
Fatty proliferation, engorged vessels, inflammatory stranding around bowel
Abscesses, especially perirectal
Fluoroscopic
“String” sign of narrowed lumen
Fistulae to skin or adjacent bowel loops
Thickened mucosal folds
Cobblestone pattern: Longitudinal and transverse ulcers
Incarcerated Inguinal Hernia
Diagnosed with loops of bowel in scrotum
Detected clinically, easily confirmed by ultrasound
Helpful Clues for Less Common Diagnoses
Hirschsprung Disease
Abnormal rectosigmoid ratio (R/S diameter < 1) on contrast enema may be clue
Meconium Plug Syndrome (Small Left Colon Syndrome)
Contrast enema: Transition point between dilated proximal and narrow distal colon
Meckel Diverticulum
Mimics appendicitis: Thickened, blind-ending tubular structure in abdomen/pelvis
Rule of 2s: 2% of population, within 2 feet of ileocecal valve, symptoms before age 2
Tc-99m pertechnetate scan demonstrates focus of activity in lower abdomen
Jejunoileal Atresia
Ileal atresia contrast enema: Microcolon
Jejunal atresia contrast enema: Normal caliber colon
If microcolon on contrast enema, expect presence of other distal atresias
Meconium Ileus
Radiograph: Distal bowel obstruction
Fluoroscopy: Microcolon, meconium pellets in terminal ileum
Meconium ileus not excluded until contrast refluxes into terminal ileum
Gastrointestinal Duplication Cysts
Most common location is terminal ileum
Ultrasound: Round, hypoechoic structure with bowel wall signature
Helpful Clues for Rare Diagnoses
Distal Intestinal Obstructive Syndrome
Meconium ileus equivalent
Must be suspected with small bowel obstruction in cystic fibrosis population
Image Gallery
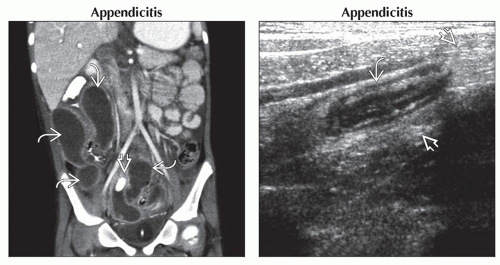 (Left) Coronal CECT shows numerous, rim-enhancing, loculated fluid collections
 interspersed among the loops of bowel, consistent with intraperitoneal abscesses resulting from a ruptured appendicitis. Note the sizable appendicolith interspersed among the loops of bowel, consistent with intraperitoneal abscesses resulting from a ruptured appendicitis. Note the sizable appendicolith  . (Right) Longitudinal ultrasound shows a dilated, noncompressible, tubular structure . (Right) Longitudinal ultrasound shows a dilated, noncompressible, tubular structure  in the RLQ, surgically confirmed to be an appendicitis. Note the surrounding echogenic and inflamed periappendiceal fat in the RLQ, surgically confirmed to be an appendicitis. Note the surrounding echogenic and inflamed periappendiceal fat  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|