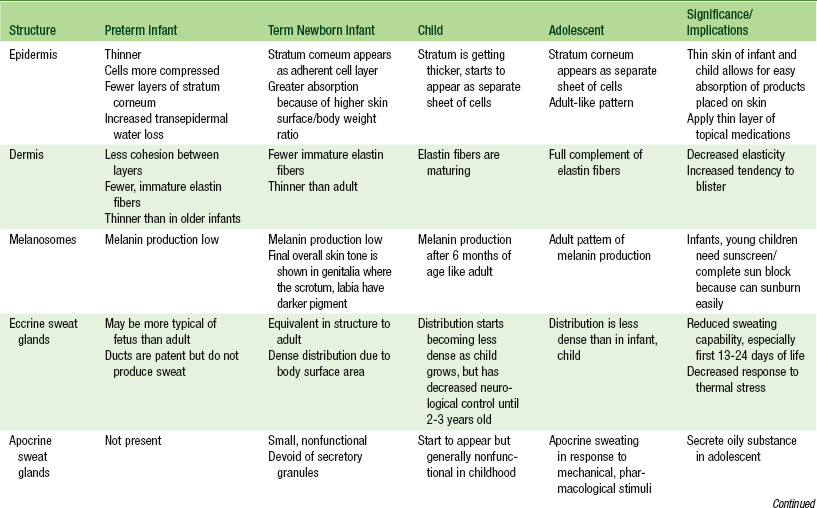
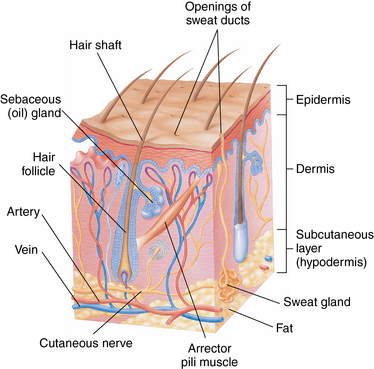
CHAPTER 6 It is easy to underestimate the importance of a thorough examination of the skin. Careful inspection of the skin gives the examiner clear insight into the overall health of the child. Examination of the skin, hair, and nails provides clues to oxygenation, tissue perfusion, nutritional and hydration status of the child, and any underlying disease pathology or injury.1 The skin of an infant, child, and adult share similarities in structure and function, but a child’s skin reacts differently to environmental demands because of the unique skin properties of each age group. All skin, regardless of age, is affected by seasonal factors such as the heat and humidity of summer or the dryness and low humidity of winter; but the differences in an infant’s skin and ability to sweat compared with an adult’s skin can create many more problems associated with these seasonal changes. Therefore, the manifestations of a skin disorder observed in an infant or child may vary widely from what may be seen in an adult.2 The skin is the largest organ in the body and has five distinct functions. The skin controls fluids, regulates temperature, protects against invasion from microbial and foreign bodies, and protects against damage from the ultraviolet (UV) rays of the sun. Finally, the skin is an organ of communication. Touch and skin-to-skin contact is one of the ways we bond with our mothers and families at birth and later bond with our sexual partners. Research conducted over the past 50 years has proven that touch is more important to humans than food in regard to optimal development.3–6 Having a disease of the skin, hair, or nails that prevents or decreases human touch can be devastating to a child’s self-esteem. The skin consists of three layers: the epidermis, the dermis, and the subcutaneous layer (Figure 6-1). The epidermis is the outermost layer of the skin and consists of two main layers: the stratum corneum, and the cellular stratum. The stratum corneum is the very top layer of the skin and is composed of stacked, overlapping nonnucleated keratinized cells called corneocytes. The thickness of this layer depends on the region of the body, being thinnest on the face and thickest over the soles of the feet.2 This layer forms the protective barrier of the skin and contains the waterproofing protein keratin, which restricts water loss and penetration of a variety of substances through the skin. The innermost layer of the epidermis consists of a single row of columnar cells called basal cells, which reside in the stratum basale. These cells divide to form the keratinocytes that move to the surface through the stratum spinosum, stratum granulosum, and stratum lucidum to replace the cells that are sloughed off every day in the stratum corneum.2,7 The stratum basale also contains melanocytes, which synthesize melanin to provide color and protect the skin from damage by the UV rays of the sun. The dermal-epidermal junction lies beneath the stratum basale and is an important site of attachment in the skin. This junction allows nutrients to pass through the dermis to the avascular epidermis. FIGURE 6-1 Anatomy of the skin. (From Thibodeau GA, Patton KT: Anatomy and physiology, ed 5, St. Louis, 2003, Mosby.) The sweat glands in the dermis control thermoregulation by releasing water through the skin. The eccrine sweat glands are distributed throughout the body except for the lip margins, eardrums, nail beds, inner surface of the prepuce, and the glans penis.8 The apocrine sweat glands are larger and deeper than the eccrine glands and secrete an odorless white fluid (sweat) in response to emotional or physical stimuli. They are located in the axillae, around the nipples, areolae, anogenital area, eyelids, and external ears. Body odor in adolescence comes from bacterial decomposition of the sweat produced by these glands; activation of these glands earlier than adolescence should be investigated. Neonates have the ability to respond to thermal stress by sweating, though it requires a greater thermal stimulus. This response is less developed in premature infants and increases with postnatal age.9 Full-term infants are also able to respond to emotional stress by sweating, though this is not developed in the premature infant. This has clinical implications related to increased insensible water loss and thermoregulation in infants at risk.9 The sebaceous glands arise from the hair follicles deep within the dermis. The oil produced by these glands is called sebum, a lipid-rich substance that helps lubricate the skin and hair. The level of oil produced is related to hormonal levels in the bloodstream (primarily testosterone) and therefore varies throughout the life span. In the newborn, the production of sebum is accelerated while still under the influence of maternal hormones, and the glands themselves become hyperplastic until maternal hormones wane in the infant’s body. This stimulated activity results in skin conditions in the newborn such as neonatal acne. Overactive sebaceous glands appear again in adolescence and contribute to the common skin conditions acne vulgaris and tinea versicolor.2 The subcutaneous layer of the skin is composed of adipose tissue. This layer connects the dermis to underlying organs, provides insulation and shock absorption, and generates heat for the body. It also provides a reserve of calories for use by the body.9 Premature and small for gestational age infants often lack this critical layer of insulation, which causes difficulty with thermoregulation. The stratum corneum does not develop until between 23 and 25 weeks of gestation. Extremely premature infants are born without this critical top layer of skin and therefore have no protective barrier and are not able to control water loss. They need protection from the environment and can tolerate only the least amount of touching. The term newborn has a fully functional stratum corneum, but it is only about 60% of the thickness of adult skin depending on the location. A thin stratum corneum with the larger body surface area/weight ratio of the newborn may allow substances placed on the skin to pass more easily through to the bloodstream.9,10 The blood vessels continue to mature into a more adult pattern until 3 months after birth. The nerves in the skin are small and poorly myelinated at birth. The growth and myelination of the nerve fibers continue on into puberty (Table 6-1). Recent research has shown skin pigmentation or melanin should be considered as a factor for understanding some underlying skin properties and characteristics, particularly in children of multiracial ancestry. Understanding how underlying skin color and pigmentation may affect the examination and diagnosis of skin conditions allows the clinician to adjust assessment techniques and interventions using the child or adolescent’s physiological characteristics rather than racial or ethnic categorization to guide care.1 Postinflammatory hypopigmentation, absence of normal melanin, and hyperpigmentation, increased melanin, occur more frequently in darker skinned individuals, and conditions such as acne or eczema can produce significant skin color changes from postinflammatory hyperpigmentation. African-Americans, Asians, and Hispanic children are also at higher risk of keloid scarring. A keloid is a type of scar at the site of a healed skin injury resulting from an overgrowth of granular tissue composed of collagen (see Table 6-4). Lighter skinned individuals may have more recognizable signs of skin breakdown, sun exposure, and tissue perfusion than darker skinned individuals. Looking at the sclerae, conjunctivae, buccal mucosa, lips, tongue, and nail beds will assist the health care provider in assessing children and adolescents with significant clinical variations in pigmentation and skin color. Variations of skin pigmentation with darker skinned individuals normally occur on the palms, soles of feet, nail beds, and the genital area. Freckling of the buccal cavity, gums, and tongue is also common. Areas that get regular exposure to the sun may have much darker pigmentation. Other variations related to skin pigmentation or melanin may exist in the barrier properties of the skin and in the distribution of hair follicles. Variations in barrier properties and hair follicle distribution are significant because skin in darker pigmented individuals may provide more of a barrier against absorption of topically applied drugs and cosmetics. The barrier function may also prevent the penetration of some toxins.10–12 The variation in barrier properties of the skin contributes to darker skinned individuals having an increased incidence of xerosis, abnormal dryness of the skin with a loss of natural skin shine, which presents as a whitish visual appearance in darkly pigmented skin.11,12 Hair follicle distribution and hair quality differ greatly with racial and ethnic background. African-Americans have hair that is often coated in natural oils, and the frequent use of oils, hair products, and braiding may make it more challenging to assess lesions on the scalp. African-Americans are more prone to scalp infections such as tinea capitis and require more prolonged medical management. Some of these hair qualities are present in multiracial children, and it may be confusing to a mother or parent who does not have similar hair qualities. Hair, skin, and nail care practices vary widely among cultures and within cultures. Timing of a child’s first haircut is one such cultural variation. In many Asian and Latino cultures, it is common to shave the infant’s head between 3 and 9 months of age in the belief the hair will grow in thick and long. In some cultures, shaving of the head is part of a religious ceremony. Some African-American communities believe an infant’s hair should not be cut until he or she begins walking.
Skin
Anatomy and physiology
Physiological variations
Family, cultural, racial, and ethnic considerations
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree