Simple Vulvectomy—Partial
Robert E. Bristow
INTRODUCTION
The variations of simple (or superficial) vulvectomy can be classified as partial or total, depending on the extent of tissue excised. The purpose of partial simple vulvectomy is to remove the skin and subcutaneous tissues of the vulva affected by disease. Contemporary surgical treatment strives to preserve as much normal tissue as can be done safely without compromising the efficacy of therapy and to achieve a cosmetic result, restoring the vulva to as close to a normal appearance as possible.
The indications for and surgical principles of partial simple vulvectomy are similar to those for total simple vulvectomy described in Chapter 14. Partial simple vulvectomy is indicated for the treatment of 1) extensive vulvar intraepithelial neoplasia that is not amenable to ablative (e.g., CO2 laser and cavitational ultrasonic surgical aspirator) therapy or for lesions that require complete pathological evaluation due to concern for an underlying invasive cancer, 2) Paget disease of the vulva with no evidence of an underlying adenocarcinoma, 3) selected cases of lichen sclerosis unresponsive to medical management, and 4) specific benign lesions such as extensive condyloma acuminata and hidradenitis suppurativa. As partial simple vulvectomy is performed for preinvasive disease, concomitant inguinofemoral lymphadenectomy is not indicated. Lower genital tract dysplasia may be multifocal; therefore, a thorough examination of the vulva, vagina, and cervix for preinvasive and invasive disease is a prerequisite.
Surgical principles for partial simple vulvectomy dictate only that a visibly disease-free margin of tissue be excised, usually 3 to 5 mm, and that the full thickness of the involved skin or mucosa is removed. Additional subcutaneous tissue may be excised to facilitate wound closure as needed. The surgical approach should be individualized and the extent of resection tailored to the extent of disease. Usually, the vulvar lesion will be sharply demarcated and frozen section examination of surgical margins is unnecessary. The exception may be vulvar Paget disease; however, the accuracy and utility of frozen section surgical margins to guide the extent of resection in this setting is debated.
PREOPERATIVE CONSIDERATIONS
In preparation for partial simple vulvectomy, all patients should undergo a comprehensive history and physical examination focusing on those areas that may indicate a reduced capacity to tolerate surgery or disease-related characteristics (e.g., primary lesion clinically suspicious for invasive cancer, inguinal adenopathy) that would contraindicate a conservative surgical approach. Routine laboratory testing should include a complete blood count, serum electrolytes, age-appropriate health screening studies, and electrocardiogram for women aged 50 years and older. Preoperative imaging is unnecessary.
Prophylactic antibiotics (Cephazolin 1, Cefotetan 1 to 2 g, or Clindamycin 800 mg) should be administered 30 minutes prior to incision, and thromboembolic prophylaxis (e.g., pneumatic compression devices and subcutaneous heparin) should be initiated prior to surgery if the procedure is expected to last more than
30 minutes. The instrumentation required includes a basic vaginal surgery set and candy-cane or Allen Universal Stirrups (Allen Medical Systems, Cleveland, OH). Enemas should be administered the evening before surgery, but a full mechanical bowel preparation is unnecessary.
30 minutes. The instrumentation required includes a basic vaginal surgery set and candy-cane or Allen Universal Stirrups (Allen Medical Systems, Cleveland, OH). Enemas should be administered the evening before surgery, but a full mechanical bowel preparation is unnecessary.
SURGICAL TECHNIQUE
Either general or regional anesthesia is acceptable. The patient should be positioned in dorsal lithotomy position using Allen-type or candy-cane stirrups with the buttocks protruding slightly over the edge of the operating table. The vulva and vagina are prepped and a Foley catheter is placed. Examination under anesthesia should pay particular attention to the size and topography of the vulvar lesion, mobility of surrounding tissues, the vagina and cervix (to exclude a synchronous lesion), and the inguinofemoral lymph nodes.
The surgical margins are outlined with a surgical marking pen, allowing a 3- to 5-mm margin of normal-appearing tissue in all directions. The resection is typically limited to the skin of the vulva and mucosa of the vaginal vestibule. Surgical planning at the time of incision should give specific consideration to the plan for wound closure and ensure that the wound can be closed in a tension-free fashion. Primary closure is achieved by raising the surrounding vulvar skin as advancement flaps and suturing it to the mucosa of the vestibule. If a tension-free closure is not achievable, the wound can be left open and covered with a nonadherent dressing to close by secondary intention.
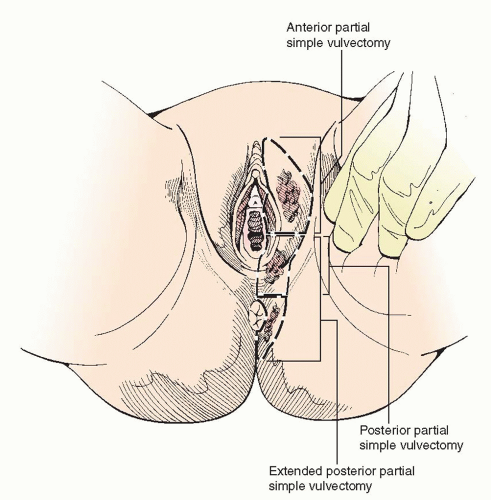 FIGURE 13.1 Delineation of incision lines for total simple vulvectomy and variants of partial simple vulvectomy. |
The typical skin incision for total simple vulvectomy (Chapter 14




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


