Shoulder Dystocia
Shoulder dystocia is one of the most dreaded and dramatic complications encountered in obstetrics. It is a true emergency, and when it occurs, it can result in high rates of maternal morbidity as well as neonatal morbidity and mortality (Calder, 2000). Resnik (1980) defines shoulder dystocia as a condition requiring special maneuvers in order to deliver the shoulders following an unsuccessful attempt to apply downward traction; Benedetti (1989) more specifically defines this condition as arrest of spontaneous delivery due to impaction of the anterior shoulder against the symphysis pubis (Fig. 11-1). Proper management of shoulder dystocia requires prior consideration of risk factors, a well-conceived plan of action, and rapid execution (Dignam, 1976; Calder, 2000). The basic clinical tenets of shoulder dystocia management are prompt recognition, specific maneuvers to deliver the impacted shoulders, and avoidance of excessive forces to the fetal and maternal tissues, all during a relatively brief time.
FIGURE 11-1. Shoulder dystocia. The shoulders are in an anteroposterior diameter, with the anterior shoulder impacted behind the symphysis pubis, and the posterior shoulder behind the sacral promontory.
HISTORY
Shoulder dystocia has been described in the medical literature for at least two centuries. Swartz (1960) quoted Smellie, in 1730: “A sudden call to a gentlewoman in labor. The child’s head delivered for a long time—but even with hard pulling from the midwife, the remarkably large shoulder prevented delivery. I have been called by midwives to many cases of this kind, in which the child was frequently lost.” Even as late as 1966, shoulder dystocia received relatively little attention; in the thirteenth edition of Williams Obstetrics (Eastman and Hellman, 1966), only one page is devoted to the subject.
Morris (1955) described the clinical phenomenon of “broad shoulder dystocia” graphically:
The delivery of the head with or without forceps may have been quite easy, but more commonly there has been a little difficulty in completing the extension of the head. The hairy scalp slides out with reluctance. When the forehead has appeared it is necessary to press back the perineum to deliver the face. Fat cheeks eventually emerge. A double chin has to be hooked over the posterior vulval commissure, to which it remains tightly opposed. Restitution seldom occurs spontaneously, for the head seems incapable of movement as a result of friction with the girdle of contact at the vulva. On the other hand, gentle manipulation of the head sometimes results in a sudden 90-degree restitution as the head adjusts itself without descent to the antero-posterior position of the shoulders. Time passes. The child’s face becomes suffused. It endeavors unsuccessfully to breathe. Abdominal efforts by the mother or by her attendants produce no advance, gentle head traction is equally unavailing. Usually equanimity forsakes the attendants—they push, they pull. Alarm increases. Eventually, “by greater strength of muscle or by some infernal juggle,” the difficulty appears to be overcome, and the shoulder and trunk of a goodly child are delivered. The pallor of its body contrasts with the plum-coloured cyanosis of the face, and the small quantity of freshly expelled meconium about the buttocks. It dawns upon the attendants that their anxiety was not ill founded, the baby lies limp and voiceless, and only too often remains so despite all efforts at resuscitation.
INCIDENCE
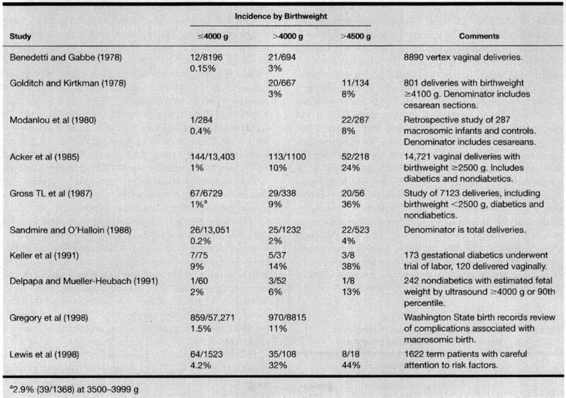
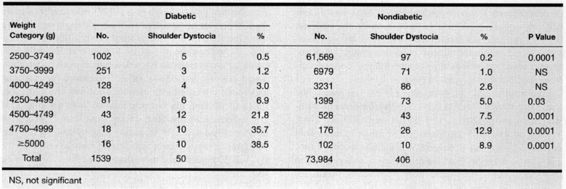
The incidence of shoulder dystocia is difficult to determine because of variations in definition and methods of reporting. Sandmire and O’Halloin (1988) report an overall incidence of approximately 0.2–0.5 percent of deliveries. Hopwood (1982) described an increasing incidence of shoulder dystocia, which was reported to have occurred in 0.2 percent of deliveries between 1966 and 1976, but increased to 1.1 percent between 1976 and 1981. He attributed this increase to the general trend toward larger birthweight, a finding confirmed by Modanlou and coworkers in 1982. On the other hand, Sandmire and O’Halloin (1988) reviewed the literature and concluded that there was no evidence of an increased incidence in shoulder dystocia reported during the twentieth century. Table 11-1 summarizes the incidence of shoulder dystocia with respect to birthweight in several series. The incidence of this complication varies depending upon the methods of reporting, the specific patient population, and the subgroups of patients reported (total population, diabetics vs. nondiabetics, etc).
TABLE 11-1. Birthweight and Shoulder Dystocia
In an attempt to make reporting of shoulder dystocia more reproducible, Spong and associates (1995) proposed an objective definition that depends on (a) the time interval between delivery of the fetal head and the fetal body; and (b) the use of obstetric maneuvers that have been proposed to alleviate shoulder dystocia. Beall and associates (1998) then attempted to validate the definition by prospective evaluation of 722 patients assessing the head to body time (>60 seconds consistent with shoulder dystocia) and/or use of ancillary maneuvers to effect delivery. Of the 99 cases of shoulder dystocia using this definition, the practitioner subjectively identified only 25 percent. Those deliveries requiring special maneuvers were more likely to be identified by the practitioner. The patients meeting this definition of shoulder dystocia had increased birthweights and contained all the fetal injuries in the group studied.
Beall and associates (1998) showed that 50 percent of those deliveries that required special maneuvers to effect delivery did not have documentation in the medical record of shoulder dystocia. Hypothetical reasons for such include poor record keeping, a desire to avoid additional documentation requirements, and the fear of litigation.
DIFFERENTIAL DIAGNOSIS
Swartz (1960) listed the differential diagnosis of difficulty in completing vaginal delivery of the fetus (Table 11-2). When the fetal shoulders fail to spontaneously follow delivery of the head, and other rare causes of such delay are ruled out by examination, shoulder dystocia is most likely the underlying problem.
TABLE 11-2. Differential Diagnosis of Difficulty in Completing Delivery
Short umbilical cord (absolute or relative)
Thoracic or abdominal enlargement of the infant (tumor, anasarca, anomaly)
Locked twins
Conjoined twins
Contraction ring
Shoulder dystocia
Reprinted with permission from Swartz, 1960.
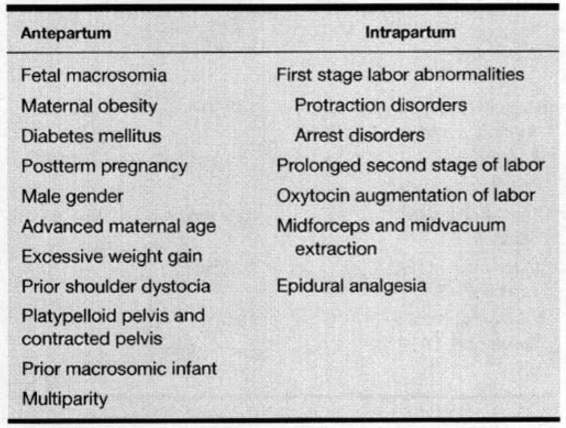
RISK FACTORS
Risk factors for shoulder dystocia may be identified during the antepartum period or during the intrapartum period (Table 11-3). Unfortunately, such risk factors are so common that they lack both sensitivity and specificity, and are of limited clinical utility (American College of Obstetricians and Gynecologists, 2000).
TABLE 11-3. Risk Factors for Shoulder Dystocia
ANTEPARTUM RISK FACTORS
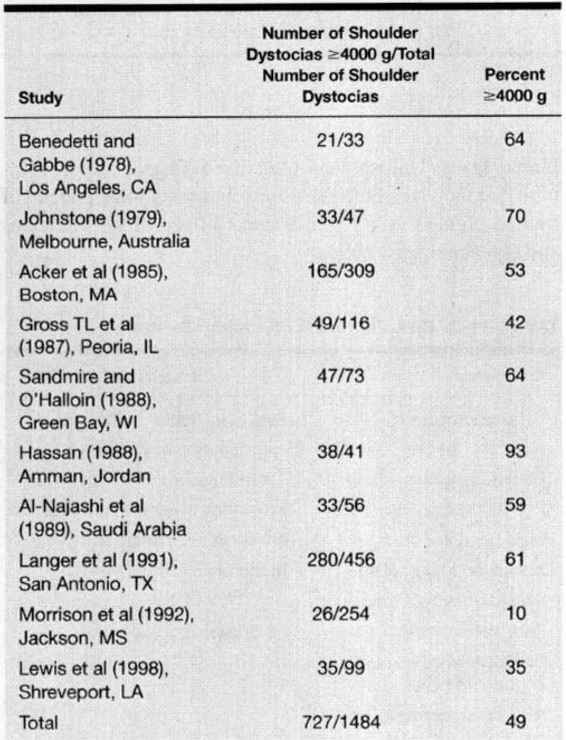
FETAL MACROSOMIA. Fetal macrosomia is a major risk for shoulder dystocia. The degree of risk is dependent upon the weight used to define macrosomia. The American College of Obstetricians and Gynecologists (2000) has stated that the diagnosis of fetal macrosomia is imprecise, but that the term “implies growth beyond a specific weight, usually 4000 g or 4500 g, regardless of gestational age.” Different populations manifest different prevalences of macrosomia. Based on the available data on Erb palsy (Acker, 1985; Lazer, 1986; McFarland, 1986; and their associates) and the vagaries of antepartum estimation of fetal weight, the American College of Obstetricians and Gynecologists (2000) suggest 4500 g “as an appropriate estimated weight beyond which the fetus should be considered macrosomic.” Adoption of a lower estimated weight would result in the identification of many infants as “at risk” despite only a relatively small increase in the risk of morbidity as a consequence of their size. Although there is general agreement with this definition for macrosomia, many studies utilize 4000 g or greater to define macrosomia. The incidence of macrosomia in reported series of shoulder dystocia is listed in Tables 11-1 and 11-4.
TABLE 11-4. Incidence of Macrosomia (≥4000 g) in Reported Series of Shoulder Dystocia
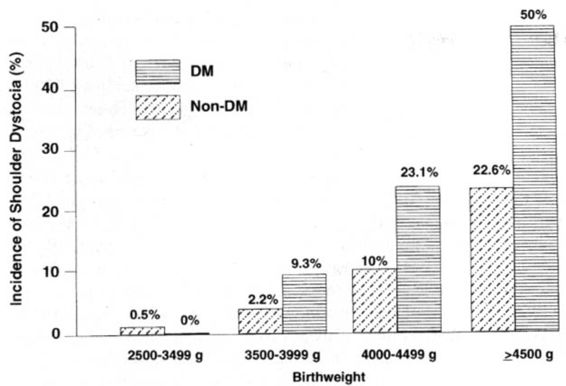
Acker and colleagues (1985) demonstrated that the incidence of shoulder dystocia increased as birthweight increased both for nondiabetics and diabetics (Fig. 11-2). They described a 10 percent incidence of shoulder dystocia in non-diabetic women delivering babies between 4000 and 4499 g as compared to a 22.6 percent incidence in nondiabetic women delivering babies weighing above 4500 g. Nesbitt and colleagues (1998) reported a similar increase in incidence of shoulder dystocia with escalating birthweights in the non-diabetic and diabetic population. Among nondiabetics with spontaneous vaginal delivery, the incidence of shoulder dystocia was 5.2 percent between 4000 and 4250 g, 9.1 percent between 4250 and 4500 g, 14.3 percent between 4500 and 4750 g, and 21.1 percent between 4750 and 5000 g.
One approach that has been suggested to minimize the risk of shoulder dystocia is a more liberal cesarean section policy for suspected macrosomia. Gross and coworkers (1987) used multiple discriminant analysis to find a model that could predict three outcome categories: no shoulder dystocia, shoulder dystocia without trauma, and shoulder dystocia with trauma. In pregnancies with an infant weighing ≥4000 g, the occurrence of shoulder dystocia could not be consistently predicted from clinical characteristics of pregnancy or labor abnormalities. These investigators calculated that if cesarean sections were performed on all infants weighing 4000 g or more, six cesarean sections would be required to prevent one case of shoulder dystocia.
In contrast, Rouse and coworkers (1996) constructed a decision analytic model to compare three policies: (a) management without ultrasound; (b) ultrasound and elective cesarean section for estimated fetal weight ≥4000 g; and (c) ultrasound and elective cesarean section for estimated fetal weight ≥4500 g. For nondiabetic women, the ultrasound policies increased cesarean section rate and costs, but lowered shoulder dystocia rate and brachial plexus injury. However, the cost for each permanent brachial plexus injury prevented by each ultrasound policy was significant (2345 cesarean sections at an additional cost of $4.9 million with 4000 g policy; 3695 cesarean sections and $8.7 million with 4500 g policy) with cesarean rates of 19.1 percent, 30.6 percent, and 27.6 percent respectively. Their conclusion was that elective cesarean delivery for ultrasound-diagnosed macrosomia was medically and financially unsound for the nondiabetic population.
Kolderup et al (1997) evaluated a cohort of 2924 macrosomic infants and likewise showed a sixfold increase in significant brachial plexus injuries, but the overall incidence of persistent cases remained low (0.3 percent). If all infants >4000 g were offered cesarean section, 258 additional cesarean sections would need to be performed to prevent one persistent injury. Therefore they suggested a trial of labor rather than elective abdominal delivery for this population. In a recent retrospective study of over 16,000 deliveries (133 infants weighing 4500 g or greater), Gonen and associates (2000) concluded that, “a policy of elective caesarean delivery in cases of suspected fetal macrosomia had an insignificant effect on the incidence of brachial plexus injury.”
An alternative strategy to cesarean delivery for management of macrosomia is labor induction. Combs and coinvestigators (1993) retrospectively evaluated induction, versus expectant management for pregnancies identified with suspected fetal macrosomia, defined as estimated fetal weight greater than the ninetieth percentile for gestational age. Unfortunately, they found a significantly higher cesarean section rate with elective induction (57 percent) versus expectant management (31 percent), without a significant reduction in shoulder dystocia. Gonen et al (1997) randomized 273 patients with estimated fetal weights of 4000–4500 g to induction of labor versus expectant management. There were no differences in cesarean section rates (19.4 percent vs. 21.6 percent), shoulder dystocia (3.7 percent vs. 4.3 percent) or brachial plexus injury. Leaphart and colleagues (1997) showed a significant increase in cesarean section rate with labor induction for suspected macrosomia compared to expectant management (36 percent vs. 17 percent). In a recent review of the Cochrane Database on elective delivery in diabetic women, Boulvain and associates (2000) could identify only one available trial. In this one study, the cesarean delivery rate was not significantly increased, but macrosomia was reduced in the elective induction group. These authors concluded that the data were too limited to support either expectant management or elective delivery.
Rydhstrom and Ingemarsson (1989) reviewed the Swedish National Medical Birth Registry for cases of birthweight exceeding 5700 g (12.5 lb) between 1973 and 1984. There were 110 newborns identified, of which 78 underwent vaginal delivery, and 40 percent (31/78) had shoulder dystocia. Four of the eight deaths in this group were secondary to shoulder dystocia, and there were 11 brachial plexus injuries. It would be most unusual not to consider the merits of cesarean delivery when the expected birthweight exceeds 5700 g.
One of the difficulties in the institution of any intervention based on antepartum ultrasound estimated weight is the inaccuracy of the estimates. Moreover, as shown in a recent review of the literature, 26 to 58 percent of shoulder dystocias, and up to 44 percent of brachial plexus injuries, occur in babies weighing less than 4000 g (Sacks and Chen, 2000). Several studies suggest that clinical estimates are more accurate than ultrasound-determined estimates using the biparietal diameter, abdominal circumference, and femur in term pregnancies (Chauhan, 1998; Sherman, 1998). Conway and Langer (1998) showed that 87 percent of cases appropriately characterized the fetus as macrosomic or not macrosomic utilizing three biometric measures. Jazayeri and colleagues (1999) showed that macrosomia is best predicted by abdominal circumference measurement alone, as compared to multiple biometric parameters. Ninety-three percent of the macrosomic infants and 100 percent of the macrosomic infants experiencing shoulder dystocia were detected by an abdominal circumference greater than 35 cm. These findings corroborate those of Smith et al (1997) who identified more than 90 percent of newborns with a birthweight of ≥4000 g using the abdominal circumference alone. Gilby and associates (2000) reviewed almost 1996 women at 36 weeks gestation or greater who delivered within 1 week of an ultrasound examination. These authors concluded that the fetal abdominal circumference measurement was clinically useful in identifying macrosomic infants. With an abdominal circumference of less than 35 cm, less than 1 percent of newborns had a weight of greater than 4500 g. If this circumference measurement was greater than 38 cm, then the risk was 37 percent, and more than half of these infants were identified.
In view of these inaccuracies of antepartum ultrasound-estimated fetal weight, and the fact that no proven benefit exists from early vaginal delivery versus cesarean section in preventing brachial plexus injuries, management solely based on ultrasound estimation of weight is not warranted (Leaphart et al, 1997).
MATERNAL OBESITY. Johnson and associates (1987) reported a 5.1 percent incidence of shoulder dystocia if the maternal weight was over 250 pounds versus a 0.6 percent incidence in women who weighed less than 200 pounds at delivery. Spellacy and coworkers (1985) found that obesity was a risk factor for macrosomia, which, in turn, was a risk factor for shoulder dystocia. Schwartz and Dixon (1958) showed that the overall incidence of shoulder dystocia was 0.2 percent in the general population, but 1.5 percent in women weighing over 180 pounds; 32 percent of all cases of shoulder dystocia occurred in women who weighed over 180 pounds. These studies and others certainly suggest an association between obesity and shoulder dystocia, but it is unclear whether obesity is an independent risk factor or is related to the common co-occurrence of macrosomia and/or diabetes mellitus. In a more recent study, Lewis et al (1998) showed no increased risk of shoulder dystocia or birth trauma with a maternal weight of greater than 90 kg.
DIABETES MELLITUS. Neonates of diabetics have increased shoulder-to-head and chest-to-head size differences relative to comparable-weight neonates of nondiabetic mothers (Modanlou and colleagues, 1982). Acker and coworkers (1985) found a relative risk of 5.2 for shoulder dystocia in diabetics when compared to nondiabetics. Cousins and associates (1985) reported that maternal carbohydrate intolerance was associated with increased birthweight, depressed 5-minute Apgar scores, increased incidence of shoulder dystocia, and increased perinatal mortality. Figure 11-2 illustrates the relationship between birthweight, maternal diabetes, and shoulder dystocia. One study of gestational diabetics found a 9 percent incidence of shoulder dystocia with birthweight between 3500 and 3999 g, an incidence that increased to 14 percent with birthweight of 4000–4499 g, and to 38 percent with birthweight greater than 4500 g (Keller and coworkers, 1991). Langer and co-investigators (1991) found that birthweight and diabetes ranked highest as risk factors for shoulder dystocia in their population (Table 11-5). In a prospective study, Conway and Langer (1998) showed that elective cesarean section for an estimated fetal weight ≥4250 g and elective induction for estimated fetal weight equal to or greater than the ninetieth percentile but <4250 g decreased the rate of shoulder dystocia significantly (2.4 percent vs. 1.1 percent, odds ratio 2.2).
FIGURE 11-2. The incidence of shoulder dystocia among 14,721 vaginal deliveries with birthweight ≥2500 g, according to birthweight and diabetic status. (Data from Acker and associates, 1985.)
TABLE 11-5. Shoulder Dystocia as Related to Birthweight in Diabetic and Nondiabetic Pregnant Women
Pederson (1954) found a trend of lower birthweight of infants of those diabetics receiving long-term insulin therapy as compared to those undergoing short-term therapy. Coustan and Imarah (1984) also found that insulin therapy decreased the incidence of macrosomia, operative delivery, and birth trauma in gestational diabetics. Berne and associates (1985) confirmed these observations and proposed the use of prophylactic insulin for this purpose.
POSTTERM PREGNANCY. Postterm pregnancies also have been associated with shoulder dystocia (Johnson, 1987; Eden, 1987; and their colleagues). Several studies found that nearly half of shoulder dystocia cases were associated with a pregnancy extending beyond 41 weeks of gestation (Johnstone, 1979; Hopwood, 1982). Spellacy and associates (1985) suggested that postterm pregnancy is a risk factor for macrosomia, itself a risk factor for shoulder dystocia. Excluding postterm pregnancies with birthweight greater than 4000 g, Acker and colleagues (1985) found that the overwhelming majority of postterm pregnancies were not associated with shoulder dystocia.
MALE GENDER. Several studies associate male gender with shoulder dystocia. Parks and Ziel (1978) found that 72 percent of 110 macrosomic (≥4500 g) neonates were males. Spellacy and associates (1985) found that 67 percent of 574 macrosomic (>4500 g) infants were males. In a series of 41 cases of shoulder dystocia reported by Hassan (1988), 28 (68 percent) were male.
ADVANCED MATERNAL AGE. Advanced maternal age as a risk factor for shoulder dystocia depends upon the coexistence of diabetes mellitus and obesity; thus, it is not an independent risk factor for shoulder dystocia. Using logistic regression analysis, Langer and coworkers (1991) and Lewis and coworkers (1998) found that maternal age did not contribute to the risk of shoulder dystocia.
EXCESSIVE MATERNAL WEIGHT GAIN. Schwartz and Dixon (1958) studied 50 cases of shoulder dystocia; 14 percent of the mothers gained over 30 pounds, and 32 percent of shoulder dystocia cases occurred in women weighing more than 180 pounds. In 80 percent of these cases, the fetus weighed more than 4000 g. Lewis and coworkers (1998) found a positive relationship between maternal weight gain ≥20 kg and shoulder dystocia (25 percent vs. 16 percent, P = 0.02). It is unclear whether this represents an independent risk factor for shoulder dystocia or simply an association of excessive weight gain with macrosomia. Existing data certainly corroborates the linear relationship between maternal weight gain during pregnancy and birthweight (Niswander et al, 1969; Boyd et al, 1983).
PRIOR SHOULDER DYSTOCIA. Lewis and coworkers (1995) reviewed their shoulder dystocia cases over a 10-year period with an overall incidence of 2 percent. Of the 747 cases with shoulder dystocia, 101 patients had 123 subsequent vaginal deliveries with shoulder dystocia recurrence complicating 14 percent of those pregnancies. Eighty-two percent of the recurrent cases had larger birthweights than the previous pregnancy complicated by shoulder dystocia. Smith et al (1997) also suggested a significantly increased recurrence risk. Whether patients with a history of shoulder dystocia should be offered an elective abdominal delivery is unclear and requires further investigation.
CONTRACTED PELVIS AND PLATYPELLOID PELVIS. In one study, a contracted pelvis did not contribute to shoulder dystocia except in cases where birthweight was less than 4000 g; among 10 cases of shoulder dystocia with birthweight under 4000 g, 5 cases were noted to have borderline maternal pelvis measurements (Schwartz and Dixon, 1958). Seigworth (1966) reported a series of 51 cases of shoulder dystocia; x-ray pelvimetry was available in 9 cases. A platypelloid pelvis was found in two cases, and reduced anteroposterior and posterior sagittal diameters of the outlet were evident in a third case. Six cases showed no evidence of contraction of the bony pelvis by x-ray. Clinical pelvimetry indicated that 47 cases were normal and 4 were contracted; a J-shaped coccyx with forward projection was suggested in 10 cases. Although these retrospective observations are interesting, the data are of limited clinical utility.
PRIOR MACROSOMIC INFANT. From the previous discussion of macrosomia, it is apparent that interpretation of data is made difficult by varying definitions of the weight that defines macrosomia. Some studies suggest that delivery of a prior macrosomic infant increases the risk of shoulder dystocia; 8 of 31 women who experienced shoulder dystocia in one series had delivered 4082 g (9 lbs) or larger infants in previous pregnancies without difficulty (Swartz, 1960). Seigworth (1966) noted that 35 percent of women experiencing a shoulder dystocia had given birth previously to an infant weighing at least 4000 g. Lewis and coworkers (1998) revealed an increased incidence of prior macrosomic infants (11 percent) among patients experiencing shoulder dystocia as compared to controls (5 percent). In a retrospective analysis of 185 shoulder dystocia patients, 1 of 79 with birthweight <4000 g and 31 of 106 with birthweight >4000 g had had a previous infant weighing >4000 g (Nocon and associates, 1993). In contrast, Lazer and colleagues (1986) found a relative decrease in shoulder dystocia, Erb palsy, and clavicular fracture in women who had previously given birth to an infant weighing >4500 g. These data would, in composite, seem to best justify an approach of individualized management.
INTRAPARTUM RISK FACTORS
PROLONGED SECOND STAGE OF LABOR. Prolonged second stage of labor has been associated with increased risk of shoulder dystocia (Beneditti and Gabbe, 1978; Acker, 1985, 1986; SJ Gross, 1987; TL Gross, 1987; and their coworkers). Benedetti and Gabbe (1978) noted that the overall incidence of shoulder dystocia was 0.37 percent of 8890 vertex vaginal deliveries. With a prolonged second stage and midpelvic delivery, the incidence of shoulder dystocia was 4.6 percent. If the birthweight exceeded 4000 g, the second stage was prolonged, and midpelvic delivery was performed, the incidence of shoulder dystocia was 23 percent. TL Gross and associates (1987) reported midforceps delivery in 50 percent and prolonged second stage in 25 percent of their cases of shoulder dystocia, with a combination of prolonged second stage and midforceps delivery in 21 percent of their cases of shoulder dystocia. Acker and coworkers (1985) found that 22 percent of patients with a shoulder dystocia had protraction disorders and 8 percent had arrest disorders; however, 70 percent of patients with shoulder dystocia had a normal labor pattern.
OXYTOCIN ADMINISTRATION. The association of oxytocin administration may be a secondary factor in the development of shoulder dystocia, but there is no evidence of a direct causal link. The apparent connection between shoulder dystocia and oxytocin administration may be related to the compounds used to augment or induce labor in cases of labor disorders or fetal macrosomia.
FORCEPS AND VACUUM EXTRACTION. Operative vaginal delivery is associated with shoulder dystocia.
Broekhuizen and associates (1987) reported a 3.1 percent incidence of shoulder dystocia in women delivered by vacuum extraction as compared to a 0.3 percent incidence in a group delivered by forceps. However, the vacuum group had a higher incidence of midpelvic delivery, an increase in mean birthweight, and an increase in birthweights greater than 4000 g. McFarland (1986) also found a higher incidence of Erb palsy with midforceps delivery and vacuum extraction as compared to deliveries accomplished with low forceps, spontaneous vaginal delivery, and cesarean section. In a prospective randomized trial comparing forceps and vacuum extraction with 637 patients, Bofill and colleagues (1997) showed an increase in shoulder dystocia with the use of vacuum extraction for delivery versus forceps (4.7 percent vs. 1.9 percent). Other associated factors with shoulder dystocia were longer time to delivery (operative delivery time exceeding 6 minutes) and excessive fetal weight. Pelvic station and rotational maneuvers were not associated with an increased risk. Nesbitt and colleagues (1998) examined all births >3500 g in the California database for the year 1992. Assisted vaginal delivery with forceps or vacuum in the diabetic and nondiabetic patients was associated with a significant increase in shoulder dystocia risk (35–45 percent increase).
PREDICTING SHOULDER DYSTOCIA: ULTRASOUND EVALUTION OF THE MACROSOMIC FETUS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree