Chapter 114 Sexually Transmitted Infections
Etiology
The risk of contracting an STI exists in any adolescent who has had oral, vaginal, or anal sexual intercourse. Physical, behavioral, and social factors contribute to the adolescent’s higher risk (Table 114-1). Adolescents who initiate sex at a younger age are at higher risk for STIs, along with youth residing in detention facilities, youth attending sexually transmitted diseases (STD) clinics, young men having sex with men (YMSM), and youth who are injecting-drug users (IDUs). Adolescence-increased STI risk may in part be attributed to risky behaviors, such as sex with multiple concurrent partners or multiple sequential partners of limited duration, failure to use barrier protection consistently and correctly, and increased biological susceptibility to infection. Although all 50 states and the District of Columbia explicitly allow minors to consent for their own sexual health services, many adolescents encounter multiple obstacles to accessing this care. Adolescents who are victims of sexual assault may not consider themselves “sexually active,” given the context of the encounter, and need reassurance, protection, and appropriate intervention when these circumstances are uncovered.
Table 114-1 CIRCUMSTANCES CONTRIBUTING TO ADOLESCENTS’ SUSCEPTIBILITY TO SEXUALLY TRANSMITTED INFECTIONS
PHYSICAL
Younger age at puberty
Cervical ectopy
Smaller introitus leading to traumatic sex
Asymptomatic nature of sexually transmitted infection
Uncircumcised penis
BEHAVIOR LIMITED BY COGNITIVE STAGE OF DEVELOPMENT
Early adolescence: have not developed ability to think abstractly
Middle adolescence: develop belief of uniqueness and invulnerability
SOCIAL FACTORS
Poverty
Limited access to “adolescent friendly” health care services
Adolescent health-seeking behaviors (forgoing care because of confidentiality concerns or denial of health problem)
Sexual abuse and violence
Homelessness
Young adolescent females with older male partners
From Shafii T, Burstein G: An overview of sexually transmitted infections among adolescents, Adolesc Med Clin 15:207, 2004.
Epidemiology
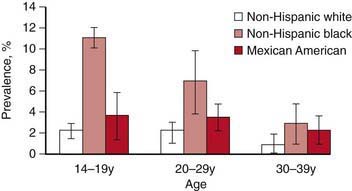
In the USA, STI prevalence varies by age, gender, and race/ethnicity. Adolescents and young adults less than 25 yr of age have the highest reported prevalence of gonorrheal (Chapter 185) and chlamydial (Chapter 218) infection; among females, rates are highest in the 15-19 yr old age group, and among males, rates are highest for 20-24 yr olds. In 2008, females 15-19 yr of age had the highest reported chlamydia rate (3,275.8 per 100,000 population), followed by females 20 to 24 years of age (3,179.9 per 100,000 population) (Fig. 114-1). The reported 2008 chlamydia rate for 15-19 yr old females was almost 5 times higher than for 15-19 yr old males. Chlamydia is common among all races and ethnic groups; however, African-American, Native American/Alaska Native, and Hispanic women are disproportionately affected. In 2008, black females 15-19 yr of age had the highest chlamydia rate of any group (10,513.4), followed by black females 20-24 yr of age (9,373.9). Data from the 1999-2002 National Health and Nutrition Examination Survey estimate the prevalence of chlamydia among the U.S. population was highest among African-Americans across all ages, including adolescents (Fig. 114-2).
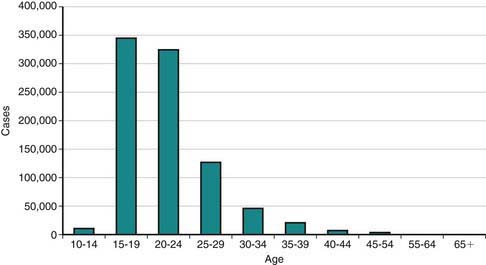
Figure 114-1 Reported Chlamydia trachomatis cases among females by age, USA, 2008.
(Adapted from the Centers for Disease Control and Prevention: Sexually transmitted diseases in the United States, 2008 [website]. www.cdc.gov/std/stats08/trends.htm. Accessed June 22, 2010.)
(Adapted from Centers for Disease Control and Prevention: Chlamydia. Sexually transmitted disease surveillance 2008 (slide presentation). www.cdc.gov/std/stats08/slides/chlamydia.ppt. Accessed June 22, 2010.)
Reported rates of other bacterial STIs are also high among adolescents. In 2008, 15-19 yr old females had the highest (636.8 per 100,000 population) and 20-24 yr old females had the second highest gonorrhea rates (608.6 per 100,000 population) compared to any other age/sex group (Chapter 185). Gonorrhea rates among 15-24 yr old females have increased for the past 5 years. Primary and secondary (P&S) syphilis rates among 15-19 yr old females have increased annually since 2004 from 1.5 cases per 100,000 population to 3.0 per 100,000 population in 2008 (Chapter 210). Rates in women have been the highest each year in the 20-24 yr age group (5.1 cases per 100,000 population in 2008). P&S syphilis rates among 15-19 yr old males are much lower than those in older males. However, these rates have increased since 2002 from 1.3 cases per 100,000 population to 5.3 in 2008. Pelvic inflammatory disease (PID) rates are highest in females aged 15-24 yr when compared to older women.
Adolescents also suffer from a large burden of viral STIs. Young people in the USA are at persistent risk for HIV infection (Chapter 268). This risk is especially notable for youth of minority races and ethnicities. In 2004 in the 35 areas with long-term, confidential name-based HIV reporting, an estimated 4,883 young people aged 13-24 yr received a diagnosis of HIV infection or AIDS, representing about 13% of the persons given a diagnosis during that year. As of April 2008, all 50 states, the District of Columbia, and 5 dependent areas use the same confidential name-based reporting system to collect HIV and AIDS data. Surveillance data on HIV infections provide a more complete picture of the HIV/AIDS epidemic and the need for prevention and care services than does the picture provided by AIDS data alone.
The STI with the highest estimated incidence in the USA is HPV. The 2003-2004 National Health and Nutrition Examination Survey (NHANES) found a third of females aged 14-24 yr were actively infected with HPV. The highest HPV infection prevalence was among females aged 20-24 yr (44.8%; 95% CI, 36.3-55.3%) (Chapter 258). Among sexually active females, half of 20-24 yr olds were HPV-infected. Although HPV infection is common, studies suggest approximately 90% of infections clear within 2 years.
Herpes simplex virus-2 (HSV-2) is the most prevalent viral STI (Chapter 244). HSV-2 prevalence rates among adolescents in the USA and young adults appear to be decreasing. The 2005-2008 NHANES estimates that 1.4% (95% CI, 1.0-2.0) of adolescents age 14-19 yr are infected with HSV-2, which is about a 76% decrease observed from the 1988-1994 NHANES and 10.5% (95% CI, 9.0-12.3) of 20-29 yr olds are HSV-2 seropositive, which is about a 39% decrease compared to the 1988-1994 NHANES (Fig. 114-3).
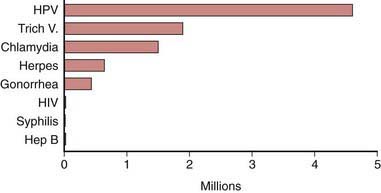
Figure 114-3 Estimated incidence of sexually transmitted infections among American youth ages 15 to 24 years, 2000.
(Adapted from Weinstock H, Berman S, Cates W: Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000, Perspect Sex Reprod Health 36:6–10, 2004.)
Pathogenesis
During puberty, increasing levels of estrogen cause the vaginal epithelium to thicken and cornify and the cellular glycogen content to rise, the latter causing the vaginal pH to fall. These changes increase the resistance of the vaginal epithelium to penetration by certain organisms (including Neisseria gonorrhoeae) and increase the susceptibility to others (Candida albicans and Trichomonas, Chapter 276). The transformation of the vaginal cells leaves columnar cells on the ectocervix, forming a border of the 2 cell types on the ectocervix, known as the squamocolumnar junction. The appearance is referred to as ectopy (Fig. 114-4). With maturation, this tissue involutes. Prior to involution, it represents a unique vulnerability to infection for adolescent females. A 15 yr old sexually active girl with endocervical colonization has a 1:8 chance of developing PID compared to the 1:80 chance for a 24 yr old. As a result of these physiologic changes, gonococcal infection becomes primarily cervical and susceptibility to ascending infection is greatest during menses, when the pH is 6.8-7.0. The association of early sexual debut and younger gynecologic age with increased risk of sexually transmitted infections supports this explanation of the pathogenesis of infection in young adolescents.
STI Screening
Early detection and treatment are the primary STI control strategies. Some of the most common STIs in adolescents, including HPV, HSV, chlamydia, and gonorrhea, are usually asymptomatic and if undetected can be spread inadvertently by the infected host. Screening initiatives for chlamydial infections have demonstrated reductions in PID cases by up to 40%. Although federal and professional medical organizations recommend annual chlamydia screening for sexually active females 24 yr and younger, in 2007, less than half (42%) of the sexually active females enrolled in commercial and Medicaid health plans were screened. The lack of a dialogue about STIs or the provision of STI services at annual preventive service visits to adolescents who are sexually experienced are missed opportunities for screening and education. Comprehensive, confidential, reproductive health services including STI screening should be offered to all sexually experienced adolescents (Table 114-2).
Table 114-2 ROUTINE LABORATORY SCREENING RECOMMENDATIONS FOR SEXUALLY TRANSMITTED INFECTIONS IN SEXUALLY ACTIVE ADOLESCENTS AND YOUNG ADULTS
Chlamydia trachomatis AND Neisseria gonorrhoeae
HIV
SYPHILIS
HEPATITIS C VIRUS
NO RECOMMENDATIONS
STD, sexually transmitted diseases; HIV, human immunodeficiency virus; YMSM, young men who have sex with men; HPV, human papillomavirus; HAV, hepatitis A virus; HBV, hepatitis B virus.
From Centers for Disease Control and Prevention: Sexually transmitted diseases treatment guidelines, 2010, MMWR 59(No. RR-12):1-110, 2010.
Definitions, Etiology, and Clinical Manifestations
Urethritis
Urethritis is an STI syndrome characterized by inflammation of the urethra, usually due to an infectious etiology. Urethritis may present with urethral discharge, urethral itching, dysuria, or urinary frequency. Urgency, frequency of urination, erythema of the urethral meatus, and scrotal pain are less common clinical presentations. Many patients are completely asymptomatic at the time of diagnosis. On examination, the classic finding is mucoid or purulent discharge from the urethral meatus (Fig. 114-5). If no discharge is evident on exam, providers may attempt to express discharge by applying gentle pressure to the urethra from the base distally to the meatus 3-4 times. Chlamydia trachomatis and N. gonorrhoeae are the most commonly identified pathogens. Mycoplasma genitalium and Ureaplasma urealyticum are considered potential pathogens in nongonococcal urethritis (NGU) when chlamydia is not confirmed. NGU caused by these pathogens may be less responsive to usual NGU therapy. Trichomonas vaginalis and HSV should also be considered in the NGU differential diagnosis. Sensitive diagnostic tests for these NGU pathogens are not available but should be considered when NGU is not responsive to treatment. Noninfectious causes of urethritis include urethral trauma or foreign body. Unlike in females, urinary tract infections are fairly rare in males who have no past genitourinary medical history. In the typical sexually active adolescent male, dysuria and urethral discharge suggest the presence of an STI unless proven otherwise. Laboratory evaluation is essential to identify the involved pathogens to determine treatment, partner notification, and disease control.
Epididymitis
The inflammation of the epididymis in adolescent males is most often associated with an STI, most frequently C. trachomatis or N. gonorrhoeae. The presentation of unilateral scrotal swelling and tenderness, often accompanied by a hydrocele and palpable swelling of the epididymis, associated with the history of urethral discharge, constitute the presumptive diagnosis of epididymitis. Testicular torsion, a surgical emergency usually presenting with sudden onset of severe testicular pain, should be considered in the differential diagnosis (Chapter 539). Males who practice insertive anal intercourse are also vulnerable to Escherichia coli infection.
Vaginitis
Vaginitis is a superficial infection of the vaginal mucosa frequently presenting as a vaginal discharge, with or without vulvar involvement (Chapter 543). Bacterial vaginosis, vulvovaginal candidiasis (VVC), and trichomoniasis are the predominant infections associated with vaginal discharge. Bacterial vaginosis is replacement of the normal H2O2–producing Lactobacillus sp. vaginal flora by an overgrowth of anaerobic microorganisms as well as Gardnerella vaginalis, Ureaplasma, and Mycoplasma. Although bacterial vaginosis is not categorized as a STI, sexual activity is associated with increased frequency of vaginosis. VVC, usually caused by C. albicans, can trigger vulvar pruritus, pain, swelling, and redness and dysuria. Findings on vaginal exam include vulvar edema, fissures, excoriations, or thick curdy vaginal discharge. Trichomoniasis is caused by the protozoan T. vaginalis. Infected females may present with symptoms characterized by a diffuse, malodorous, yellow-green vaginal discharge with vulvar irritation or may be diagnosed by screening an asymptomatic patient. Cervicitis can sometimes cause a vaginal discharge. Laboratory confirmation is recommended because clinical presentations may vary and patients may be infected with more than 1 pathogen.
Cervicitis
The inflammatory process in cervicitis involves the deeper structures in the mucous membrane of the cervix uteri. Vaginal discharge can be a manifestation of cervicitis, if the cervical discharge is profuse. Less subtle clinical manifestations of cervicitis are irregular or postcoital bleeding, mucopurulent discharge from the os, and a friable cervix. The cervical changes associated with cervicitis must be distinguished from cervical ectopy in the younger adolescent to avoid the over diagnosis of inflammation (Fig. 114-6; see Fig. 114-4). The pathogens identified most commonly with cervicitis are C. trachomatis and N. gonorrhoeae, although no pathogen is identified in the majority of cases. HSV is a less common pathogen associated with ulcerative and necrotic lesions on the cervix.
Pelvic Inflammatory Disease
PID encompasses a spectrum of inflammatory disorders of the female upper genital tract, including endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis, usually in combination rather than as separate entities. N. gonorrhoeae and C. trachomatis predominate as the involved pathogenic organisms in younger adolescents, although PID should be approached as multiorganism etiology, including pathogens such as anaerobes, G. vaginalis, Haemophilus influenzae, enteric gram-negative rods, and Streptococcus agalactiae. In addition, cytomegalovirus (CMV) (Chapter 247), Mycoplasma hominis, U. urealyticum, and Mycoplasma genitalium (Chapter 216), may be associated with PID.






