Chapter 239 Rubella
Epidemiology
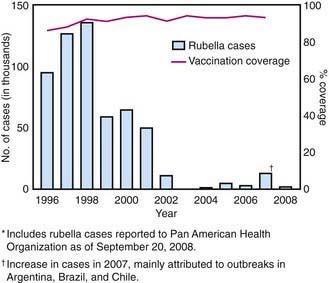
In the prevaccine era, rubella appeared to occur in major epidemics every 6-9 yr, with smaller peaks interspersed every 3-4 yr, and was most common in preschool and school-aged children. Following introduction of the rubella vaccine, the incidence fell by >99%, with a relatively higher percentage of infections reported among persons >19 yr of age. After years of decline, a resurgence of rubella and CRS occurred during 1989-1991 (Fig. 239-1). Subsequently, a 2-dose recommendation for rubella vaccine was implemented and resulted in a decrease in incidence of rubella from 0.45/100,000 in 1990 to 0.1/100,000 in 1999 and a corresponding decrease of CRS, with an average of 6 infants with CRS reported annually from 1992 to 2004. Mothers of these infants tended to be young, Hispanic, or foreign born. The number of reported cases of rubella continued to decline in the early part of this decade.
Pathology
Little information is available on the pathologic findings in rubella occurring postnatally. The few reported studies of biopsy or autopsy material from cases of rubella revealed only nonspecific findings of lymphoreticular inflammation and mononuclear perivascular and meningeal infiltration. The pathologic findings for CRS are often severe and may involve nearly every organ system (Table 239-1).
Table 239-1 PATHOLOGIC FINDINGS IN CONGENITAL RUBELLA SYNDROME
| SYSTEM | PATHOLOGIC FINDINGS |
|---|---|
| Cardiovascular | Patent ductus arteriosus |
| Pulmonary artery stenosis | |
| Ventriculoseptal defect | |
| Myocarditis | |
| Central nervous system | Chronic meningitis |
| Parenchymal necrosis | |
| Vasculitis with calcification | |
| Eye | Microphthalmia |
| Cataract | |
| Iridocyclitis | |
| Ciliary body necrosis | |
| Glaucoma | |
| Retinopathy | |
| Ear | Cochlear hemorrhage |
| Endothelial necrosis | |
| Lung | Chronic mononuclear interstitial pneumonitis |
| Liver | Hepatic giant cell transformation |
| Fibrosis | |
| Lobular disarray | |
| Bile stasis | |
| Kidney | Interstitial nephritis |
| Adrenal gland | Cortical cytomegaly |
| Bone | Malformed osteoid |
| Poor mineralization of osteoid | |
| Thinning cartilage | |
| Spleen, lymph node | Extramedullary hematopoiesis |
| Thymus | Histiocytic reaction |
| Absence of germinal centers | |
| Skin | Erythropoiesis in dermis |
Pathogenesis
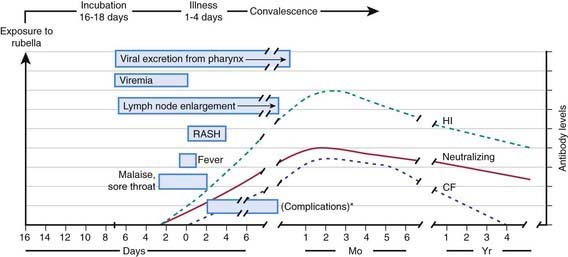
The viral mechanisms for cell injury and death in rubella are not well understood for either postnatal or congenital infection. Following infection, the virus replicates in the respiratory epithelium, then spreads to regional lymph nodes (Fig. 239-2). Viremia ensues and is most intense from 10 to 17 days after infection. Viral shedding from the nasopharynx begins about 10 days after infection and may be detected up to 2 wk following onset of the rash. The period of highest communicability is from 5 days before to 6 days after the appearance of the rash.
Clinical Manifestations
Postnatal infection with rubella is a mild disease not easily discernible from other viral infections, especially in children. Following an incubation period of 14-21 days, a prodrome consisting of low-grade fever, sore throat, red eyes with or without eye pain, headache, malaise, anorexia, and lymphadenopathy begins. Suboccipital, postauricular, and anterior cervical lymph nodes are most prominent. In children, the 1st manifestation of rubella is usually the rash, which is variable and not distinctive. It begins on the face and neck as small, irregular pink macules that coalesce, and it spreads centrifugally to involve the torso and extremities, where it tends to occur as discrete macules (Fig. 239-3). About the time of onset of the rash, examination of the oropharynx may reveal tiny, rose-colored lesions (Forchheimer spots) or petechial hemorrhages on the soft palate. The rash fades from the face as it extends to the rest of the body so that the whole body may not be involved at any 1 time. The duration of the rash is generally 3 days, and it usually resolves without desquamation. Subclinical infections are common, and 25-40% of children may not have a rash.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree