Retropubic Mid-Urethral Sling
Geoffrey W. Cundiff
INTRODUCTION
The mid-urethral sling has revolutionized the treatment of stress urinary incontinence in women by offering an easy-to-learn, minimally invasive procedure that provides excellent and reproducible results. Given the prevalence of stress urinary incontinence and associated burden of disease, the mid-urethral sling is an important procedure for the gynaecologic surgeon to master.
The retropubic approach was the original description of the mid-urethral sling but was soon followed by the transobturator approach. There is ample level-1 evidence demonstrating similar efficacy for the two approaches, but with different complication profiles. Based on these differences, the retropubic approach may provide lower complication risks for younger and older patients.
PREOPERATIVE CONSIDERATIONS
The most important preoperative preparation for a mid-urethral sling is to insure the proper diagnosis. There are several guidelines available that define the necessary diagnostic criteria (1,2). This does not routinely require urodynamics, provided that the symptoms of urinary loss with an increase in intraabdominal pressure is present and leakage can be demonstrated with a stress test (3).
In postmenopausal patients with atrophic vaginal epithelium, preoperative estrogen cream can be used to promote a healthier mucosal epithelium. A preoperative bowel prep is not indicated. While there is no evidence to support it, most surgeons utilize intraoperative antibiotic prophylaxis with a second generation cephalosporin or clindamycin in penicillin-allergic patients. There is level II data comparing a single dose of perioperative antibiotic prophylaxis to continued postoperative prophylaxis (4). This study suggests that a single dose is preferable, as the multiple dose regime had higher adverse events without an improvement in preventing surgical site infections. In the absence of patient-specific risks, deep venous thromboembolism prophylaxis is not necessary as the surgery usually takes less than 45 minutes, making it a low risk for development of deep vein thrombosis. It should be considered, however, in patients with other risk factors that increase their overall risk for development of deep vein thrombosis.
The patient should be positioned in lithotomy or modified lithotomy position with both a vaginal and lower abdominal fields. Either regional anesthesia or general anesthesia is appropriate, although level II data suggests an association between regional anesthesia and acute postoperative urinary retention that could prolong the postoperative stay (5). The mid-urethral sling procedure can also be accomplished with local anesthesia, and some surgeons prefer this approach as it allows the surgeon to adjust tension based on feedback of whether leakage occurs when the patient is asked to cough. Submucosal infiltration with injectable 1% lidocaine with epinephrine simplifies postoperative pain management and assists with dissection and hemostasis. A Foley catheter should be placed during the surgery to drain the bladder and define the course of the urethra. Following is a brief description of the surgical procedure used (see also video: Retropubic Mid-urethral Sling)
SURGICAL TECHNIQUE
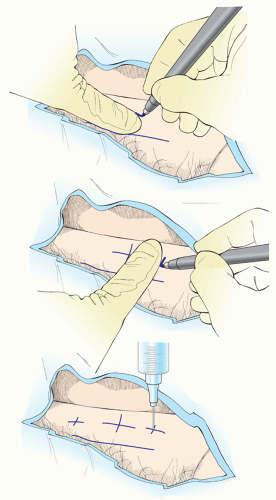
 The surgical approach begins in the suprapubic field with identification of the exit incisions for the sling. (Figure 31.1). The incisions are approximately 2 cm lateral to the midline in a transverse line that is 1.5 cm above the superior symphysis pubis. Once the sites are identified, they should be infiltrated with local anesthetic, and two small stab incisions made. (Figure 31.1) Some surgeons follow the original technique described by Ulmsten that included hydrodissection of the Retzius space using a dilute solution of Lidocaine, although experience suggests that this does not improve the safety of the procedure.
The surgical approach begins in the suprapubic field with identification of the exit incisions for the sling. (Figure 31.1). The incisions are approximately 2 cm lateral to the midline in a transverse line that is 1.5 cm above the superior symphysis pubis. Once the sites are identified, they should be infiltrated with local anesthetic, and two small stab incisions made. (Figure 31.1) Some surgeons follow the original technique described by Ulmsten that included hydrodissection of the Retzius space using a dilute solution of Lidocaine, although experience suggests that this does not improve the safety of the procedure.The surgery now moves to the vaginal field. The vaginal incision is made longitudinally in the midline, over the mid-urethra. A 1-2 cm incision is adequate, and is usually just proximal to the urethral meatus (Figure 31.2). Infiltration with local anesthetic in the line of intended dissection facilitates the dissection. The dissection is done sharply with Metzenbaum scissors and is carried laterally to the white line (arcus tendineus fasciae pelvis) (Figure 31.2). A rough indication of adequate dissection is when the screw joining the two scissor blades reaches the margin of the surgical incision. It is important not to buttonhole the vaginal epithelium, so countertraction with an Allis clamp on the margin of the incision, as well as a vaginal finger against the epithelium is useful. (Figure 31.2)
Once the dissection is complete, the sling is placed using the sling trocar. The trocar provides a minimally invasive means of placing the sling, but the blind nature of the passage makes this the most dangerous part of the procedure. To maximize the safety of the trocar passage, the surgeon should have a clear understanding of the retropubic anatomy, and the intended path of the trocar with respect to surrounding anatomical structures. The final goal is for the sling to lay beneath the mid-urethra, then pierce the pubocervical fascia just medial to the white line, traversing the space of Retzius, before piercing the rectus fascia and exiting the abdominal incisions. Proper handling of the trocars will allow the surgeon to accomplish this.
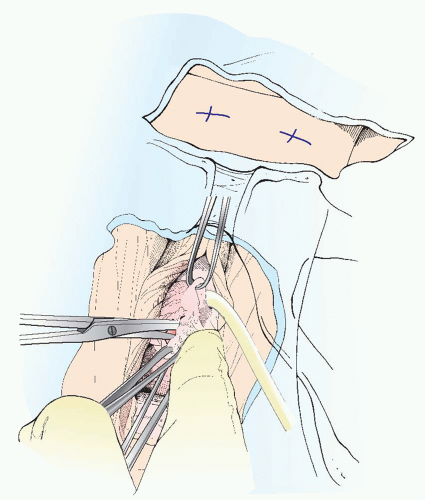 FIGURE 31.2 A midline incision is made in the distal anterior vaginal wall just proximal to the external urethral meatus. |
The original description of the procedure advocated the use of a catheter guide that is intended to move the urethra laterally to minimize injury during trocar placement. We do not use this catheter guide as it has not been shown to improve safety and increases operating time.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree