Reticulonodular Opacities
Alexander J. Towbin, MD
DIFFERENTIAL DIAGNOSIS
Common
Surfactant Deficient Disease
Bronchiolitis
Mycoplasma
Pulmonary Edema
Less Common
Langerhans Cell Histiocytosis
Aspergillus
Tuberculosis
Pneumocystis jiroveci
Rare but Important
Pulmonary Alveolar Proteinosis
Systemic Lupus Erythematosus
Niemann-Pick Disease
Pulmonary Venoocclusive Disease
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Characterized by interstitial thickening and multiple small nodules
Nonspecific pattern of disease
Helpful Clues for Common Diagnoses
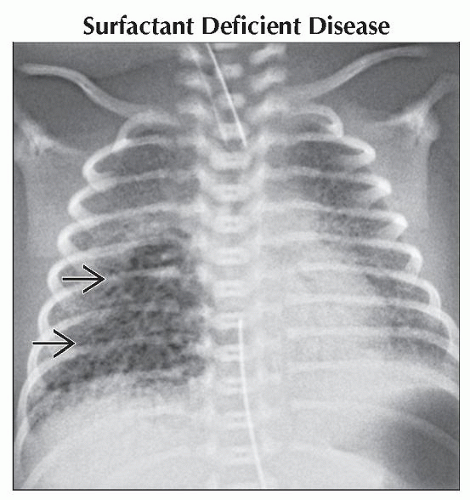
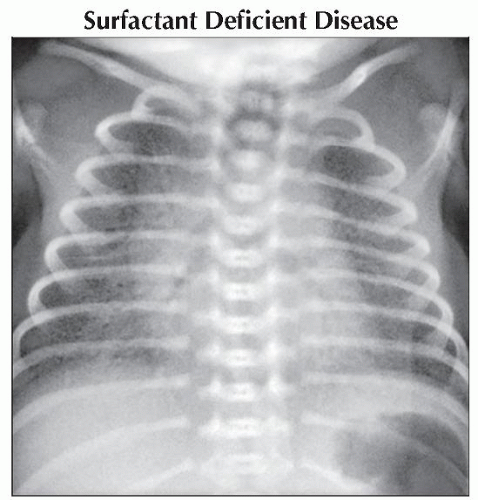
Surfactant Deficient Disease
a.k.a. respiratory distress syndrome, hyaline membrane disease
Most common cause of morbidity in premature infants
Most common in premature infants
Lack of mature type 2 pneumocytes
Most common in infants born at < 28 weeks fetal gestation
More common in males and infants of diabetic mothers
Radiograph: Decreased lung volume and diffuse reticulonodular opacities
Findings worst at 12-24 hours of life
Complications: Pneumothorax, pneumomediastinum, pulmonary interstitial emphysema
Treatment: Surfactant via endotracheal tube
Severe disease → bronchopulmonary dysplasia
Bronchiolitis
Respiratory syncytial virus (RSV) is most common cause
Most common cause of hospitalization in infants
Usually self-limiting illness
Radiograph: Hyperinflation, atelectasis, and peribronchial cuffing
Risks for severe disease: Prematurity, age < 12 weeks, chronic lung disease, congenital heart disease, immunocompromised
Mycoplasma
Common cause of community-acquired pneumonia
Most common cause of pneumonia in children > 5 years old
More severe presentation in children < 5 years old
Radiograph: Lobar consolidation, air bronchograms, or reticulonodular opacities
Reticulonodular opacities in 52%; more common in lower lobes
Pulmonary Edema
2 main causes: Cardiogenic and noncardiogenic
Cardiogenic pulmonary edema occurs when pulmonary capillary pressure is high
Overwhelms lymphatic system’s ability to resorb fluid
Associated with congenital heart disease
Usually occurs in 1st 6 months of life
Noncardiogenic causes can be neurogenic, negative pressure, or miscellaneous
Neurogenic: Associated with head trauma
Onset within hours of injury
Negative pressure: Associated with upper airway obstruction
Rapid onset and resolves when obstruction is relieved
Other causes of noncardiogenic edema: Fluid overload, acute glomerulonephritis, inhalational injury, and allergic reaction
Helpful Clues for Less Common Diagnoses
Langerhans Cell Histiocytosis
Unknown etiology
Strong association with cigarette smoking
Typically affects young adults between ages 20-40
Can affect any age
Can present with spontaneous pneumothorax
Early findings: Upper and middle lobe nodules that spare lung bases and costophrenic sulcus
Late findings: Reticulonodular opacity and cystic changes
Aspergillus
Aspergillus fumigatus: Fungus found in soil, water, and decaying organic material
Disease can be caused by allergic reaction or invasive disease
Often colonizes in patients with underlying airway disease
Aspergillomas grow in pulmonary cavities as with tuberculosis or cystic fibrosis
Invasive disease is associated with chronic granulomatous disease
Tuberculosis
Caused by Mycobacterium tuberculosis
Pulmonary infection is most common manifestation
Infection in children is usually due to close contact with infected adult
Children are less resistant to organism and disseminated disease is more common
Hallmark of primary tuberculosis is large hilar or mediastinal adenopathy
Pneumocystis jiroveci
a.k.a. Pneumocystis carinii, Pneumocystis pneumonia (PCP)
Increased incidence with AIDS and other immunocompromised states
Radiograph: Parahilar granular opacities, extensive consolidation, ground-glass opacity
Helpful Clues for Rare Diagnoses
Pulmonary Alveolar Proteinosis
Characterized by intraalveolar accumulation of surfactant-like material
3 types: Idiopathic, secondary, and congenital
Congenital type manifests in neonates; accounts for 2% of cases
Radiograph: Bilateral central and symmetric opacities with sparing of costophrenic angles and apices
Opacities can range from ground-glass to reticulonodular to consolidation
CT: “Crazy-paving” are thick septal lines superimposed on ground-glass opacity
Treatment: Whole-lung lavage, lung transplant
Systemic Lupus Erythematosus
Systemic disease
Most common thoracic manifestation is pleuritis
Can cause interstitial lung disease
Niemann-Pick Disease
Autosomal recessive disorder
Characterized by accumulation of sphingomyelin due to deficiency of sphingomyelinase
Radiograph: Diffuse reticulonodular pattern
Pulmonary Venoocclusive Disease
Rare cause of pulmonary arterial hypertension
Characterized by occlusion of pulmonary venules by fibrous tissue
Findings: Nodular ground-glass opacity, septal lines, lymph node enlargement
Image Gallery
 AP radiograph of the chest shows diffuse granular opacities of both lungs. Surfactant deficiency is the most common cause of morbidity in preterm infants. |
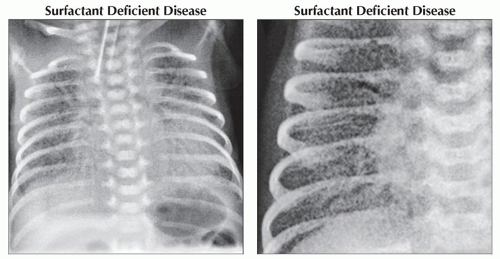 (Left) AP radiograph of the chest shows diffuse granular opacities in both lungs. Surfactant deficiency is most common in infants born at less than 28 weeks fetal gestation. (Right) AP radiograph of the chest in a different patient shows diffuse granular opacities of the right lung. Surfactant deficiency is caused by a lack of mature type 2 pneumocytes. It is treated with exogenous surfactant given by an endotracheal tube.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|