Newborn Life Support, reproduced with the kind permission of the Resuscitation Council (UK)
On successfully completing this topic, you will be able to:
understand the importannt physiological differences in the newly born baby
understand the equipment used for resuscitation at birth
understand how to assess and resuscitate the baby at birth
understand additional measures for special situations
Introducton
The resuscitation of babies at birth is different from the resuscitation of all other age groups as it usually involves a process of assisted transition from intra- to extra-uterine life, rather than recovery of a human with serious illness or injury. Knowledge of the physiology of normal transition and how interruption to transition leading to hypoxia affects this is essential to understand the process outlined in the algorithm for resuscitating newborn babies. The majority of babies will establish normal respiration and circulation without help. A tiny minority will not, and will require intervention. As some babies may be born unexpectedly out of hospital, in non-maternity setting within hospitals, or unwell as a result of peripartum circumstances, it is important that clinicians working in ‘receiving’ specialties have an understanding of the differences between resuscitating older children and a baby who has just been born. Ideally, someone trained in newborn resuscitation should be present at all deliveries. It is advisable that all those who attend deliveries regularly should have been on courses such as the Newborn Life Support course, organised by the Resuscitation Council (UK), European Resuscitation Council courses, or the Neonatal Resuscitation Programme, organised by the American Academy of Pediatrics.
Normal physiology
Successful transition at birth involves moving from a fetal state, where the lungs are fluid-filled and respiratory exchange occurs through the placenta, to that of a newly born baby whose air-filled lungs have successfully taken over that function. Preparation for this in a pregnancy progressing without incident is thought to begin in advance of labour, with detectable cellular changes occurring that may subsequently prime the lung tissues for reabsorption of the intra-alveolar fluid.
After delivery, a healthy term baby usually takes its first breath within 60–90 seconds. Stimuli for this first breath include exposure to the relative cold of the ex-utero environment, the physical stimulus of being handled at delivery, and hypoxia resulting from obstruction of the umbilical cord during clamping.
In a term baby, approximately 100 ml of fluid is cleared from the airways and alveoli, initially into the interstitial pulmonary tissue, and then later into the lymphatic and capillary systems. During vaginal delivery, only around 35 ml of fluid from the uppermost airways will be displaced by physical forces experienced by the baby during passage through the birth canal.
The respiratory pattern in newborn mammals has specifically evolved to efficiently replace the fluid in the airways and alveoli with air during the first few breaths. Animal studies show that at initiation of breathing, the inspiratory phase is longer than the expiratory phase (expiratory braking) and in humans, expiration occurs against a partially closed glottis creating backpressure (producing crying or sometimes a grunting sound). In a healthy baby the first spontaneous breaths may generate a negative inspiratory pressure of between –30 and –90 cmH2O. This pressure is 10–15 times greater than that needed for later breathing but is necessary to overcome the viscosity of the fluid filling the airways, the surface tension of the fluid-filled lungs, and the elastic recoil and resistance of the chest wall, lungs and airways. These powerful chest movements also aid displacement of fluid from the airways into the interstitial tissue before subsequent clearance into the lymphatics and ultimately the circulation. The combined effect of these events is to establish the baby’s functional residual capacity (FRC).
Neonatal circulatory adaptation commences at the same time as the pulmonary changes. Lung inflation and alveolar distension releases vasomotor compounds which reduce the pulmonary vascular resistance as well as increasing oxygenation. Evidence shows that as pulmonary vascular resistance falls during establishment of the FRC significant changes in stroke volume can be seen in the heart. Where the umbilical cord has been clamped prior to the first breath, a decrease in heart size is immediately seen, followed by return to its original size. This observation suggests a ‘sink’ effect with blood being rapidly drawn into the pulmonary vessels as the lungs inflate with air during the first breaths, without access to placental blood to fill the emptied heart quickly hence the observed decrease in size. The increase in size subsequently seen is likely due to the same large volume of blood returning to the left side of the heart from the expanded pulmonary circulation. Bradycardia has been noted in these babies consistent with the observed changes and, importantly, is not seen in babies who take their first breath before cord clamping. Circulatory adaptation proceeds with closure of the inter-atrial foramen due to pressure changes as the pulmonary venous return to the left atrium increases and finishes with functional, then permanent, closure of the ductus arteriosus over the following days.
Pathophysiology
The approach to resuscitating newborn humans evolved from observation of the pathophysiology of induced, acute, fetal hypoxia during pioneering mammal-based research in the early 1960s. The results of these experiments, which followed the physiology of newborn animals during acute, total, prolonged asphyxia and subsequent resuscitation are summarised in Figure 12.1.
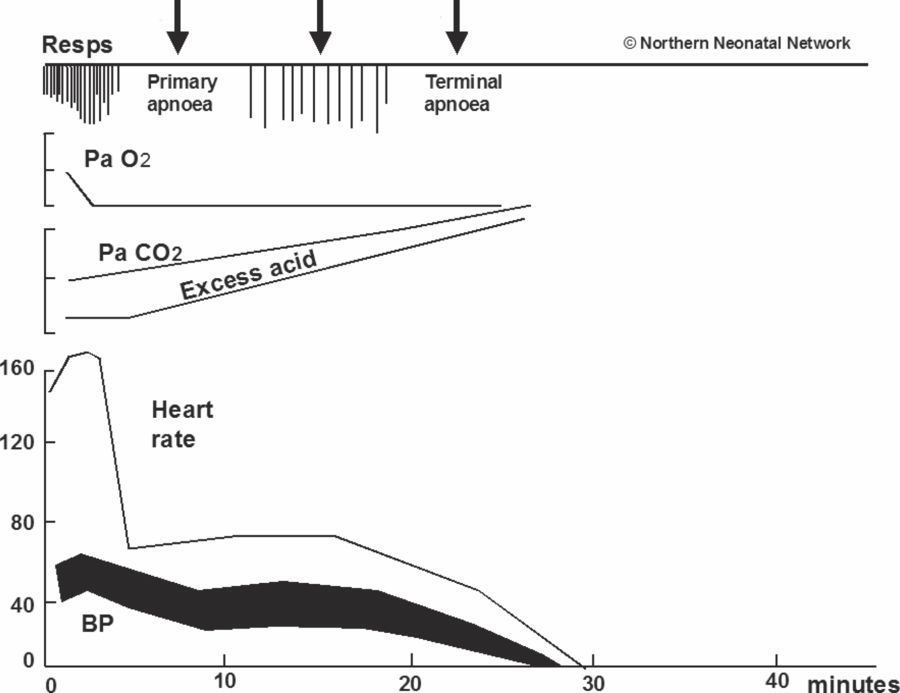
When the placental oxygen supply is interrupted or severely reduced, the fetus will initiate respiratory movements (i.e. attempt to breathe) in response to hypoxia. If the interruption of oxygen from the placenta continues and these attempts at breathing fail to provide an alternative oxygen supply – as they will inevitably fail to do so in utero surrounded by amniotic fluid – the baby will become unconscious. If hypoxia continues, the higher respiratory centre becomes inactive and unable to continue to drive respiratory movements. The breathing therefore stops, usually within 2–3 minutes. This cessation of breathing is known as primary apnoea (Figure 12.1).
In the presence of hypoxia a marked bradycardia will occur quickly. Intense peripheral vasoconstriction helps to maintain blood pressure with diversion of blood away from non-vital organs. The reduced heart rate also allows a longer ventricular filling time, and thus an increased stroke volume, which also helps maintain blood pressure.
As hypoxia continues, primary apnoea is broken: loss of descending neural inhibition by the higher respiratory centre allows primitive spinal centres to initiate forceful, gasping breaths. These deep, irregular gasps are easily distinguishable from normal breaths as they only occur 6–12 times per minute and involve all accessory muscles in a maximal, ‘whole body’, inspiratory effort. If this fails to draw air into the lungs and hypoxia continues, even this reflexive activity ceases and terminal apnoea begins. Without intervention, no further innate respiratory effort will occur. The time taken for such activity to cease is longer in the newly born baby than at any other time in life, taking up to 20 minutes.
The circulation is almost always maintained until after all respiratory activity ceases. This resilience is a feature of all newborn mammals at term and is largely due to the reserves of glycogen in the heart permitting prolonged, anaerobic generation of energy in the cardiomyocytes. Resuscitation is therefore relatively uncomplicated if undertaken before all respiratory activity has stopped. Once the lungs are aerated, oxygen will be carried to the heart and then to the brain provided the circulation is still functional (Figure 12.2). Recovery will then be rapid. Most babies who have not progressed to terminal apnoea will resuscitate themselves if their airway is open. Once gasping ceases, however, the circulation starts to fail and resuscitation becomes more difficult. Support for the circulation is then required in addition to support for the breathing (Figure 12.3).
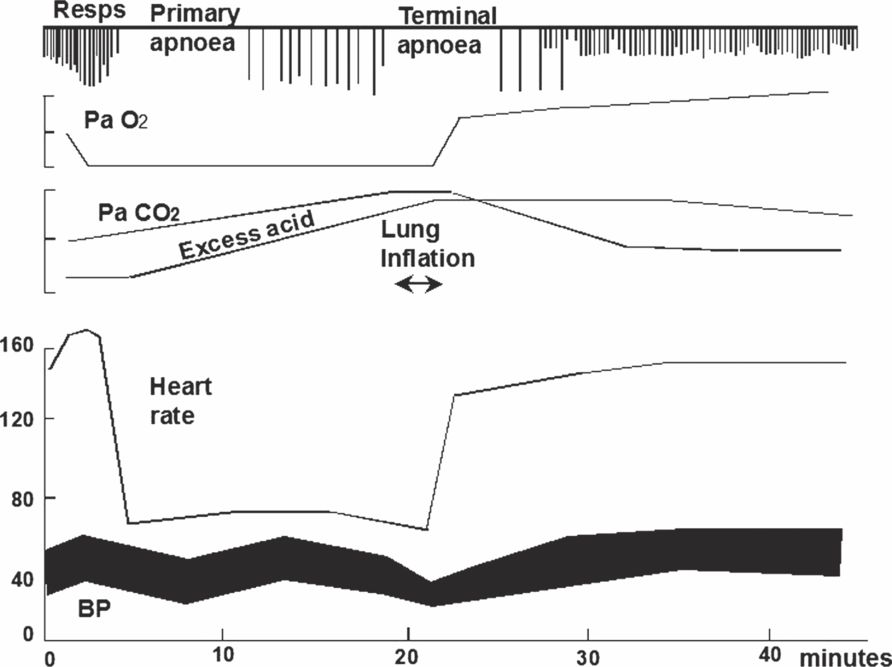
Effects of lung inflation and a brief period of ventilation on a baby born in early terminal apnoea but before failure of the circulation.
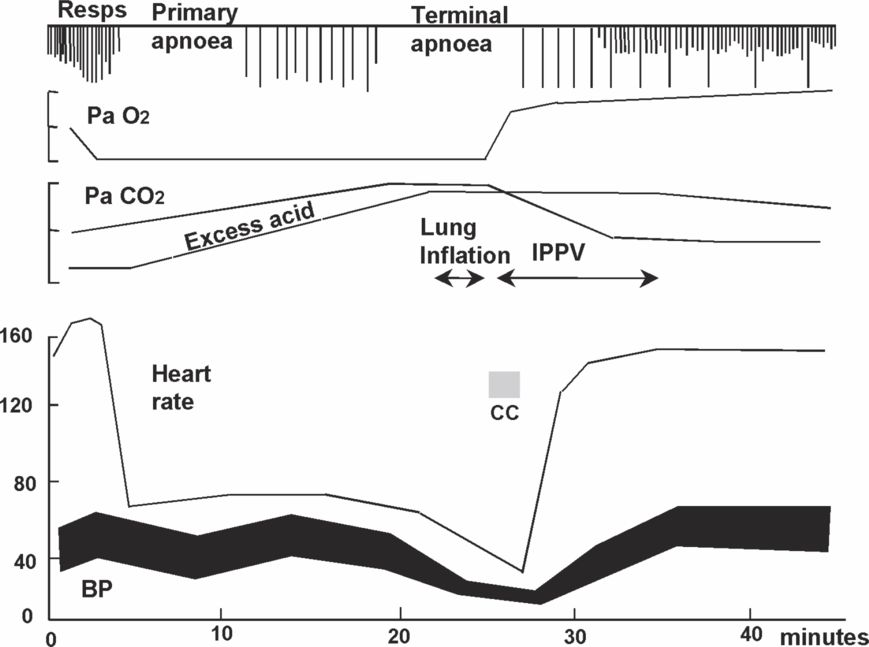
Response of a baby born in terminal apnoea. In this case lung inflation is not sufficient because the circulation is already failing. However, lung inflation delivers air to the lungs and then a brief period of chest compressions delivers oxygenated blood to the heart which then responds.
Equipment
For many newborn babies, especially those born outside the delivery room, the need for resuscitation cannot be predicted. It is therefore useful to plan for such an eventuality. Equipment that may be required to resuscitate a newborn baby is listed in box 12.1 below. As a minimum, most babies can be resuscitated if there is access to: a firm, flat surface; warmth; a way to deliver air or oxygen to the lungs in a controlled fashion to displace the fluid present in the airways at delivery if the baby does not breathe itself (ranging from using mouth-to-mouth to equipment-based techniques); and guidance from someone who is familiar with the process of newborn resuscitation (either as part of the resuscitation team or by telephone at the time of need).
A flat surface
Radiant heat source and dry towels
Plastic bag for term and preterm babies
Suitable hats
Suction with catheters of at least 12 Fr gauge
Face masks
Bag–valve–mask or T-piece with pressure-limiting device
Source of air and/or oxygen
Oropharyngeal (Guedel) airways
Laryngoscopes with straight blades, 0 and 1
Nasogastric tubes
Cord clamp
Scissors
Tracheal tubes sizes 2.5 to 4.0 mm
Umbilical catheterisation equipment
Adhesive tape
Disposable gloves
Saturation monitor/stethoscope
Strategy for assessing and resuscitating a baby at birth
Resuscitation is likely to be rapidly successful if commenced before the baby has progressed beyond the point at which its circulation has started to fail.
Babies in primary apnoea can usually resuscitate themselves if they have a clear airway. Unfortunately it is not possible during the initial assessment to reliably distinguish whether an apnoeic newborn baby is in primary or terminal apnoea. A structured approach that will work in either situation must therefore be applied to all apnoeic babies. The structured approach is outlined below. In reality the first four steps (up to and including assessment) are completed simultaneously. After this, appropriate intervention can begin following an ABC approach:
Call for help
Ask for help if you expect or encounter any difficulty or if the delivery is outside the labour suite.
Start clock
If available, or note the time of birth.
At birth
There is no need to rush to clamp the cord at delivery. It can be left unclamped while the following steps are completed. Dry the baby quickly and effectively. Remove the wet towel and wrap in a fresh, dry, warm towel. (For very small or significantly preterm babies it is better to place the wet baby in a food-grade plastic bag – and later under a radiant heater). Put a hat on all babies regardless of gestation. Assess the baby during and after drying: decide whether any intervention is going to be needed.
If your assessment suggests that the baby is in need of resuscitation, clamp and cut the cord. If the baby appears well, wait for at least 1 minute from the complete delivery of the baby before clamping the cord to allow autotransfusion and reduce the likelihood of iron deficiency anaemia.
If the baby is assessed as needing assistance/resuscitation then this becomes the priority. There is not yet sufficient evidence for advocating active resuscitation of the newborn human while still attached to the placenta by a functioning umbilical cord. Thus, the cord needs to be clamped and cut in order to deliver assistance/resuscitation.
Keep the baby warm
The normal temperature range for a newborn baby is 36.5°C to 37.5°C. For each 1°C decrease in admission temperature below this range in otherwise healthy term newborn babies, there is an associated increase in mortality of 28%. In environments likely to receive sick babies or infants the room temperatures should be kept, as a baseline, as close as possible to the recommended minimum for term babies. Where delivery or admission of a newborn baby is imminent outside these environments, anticipation and active management of room temperature to achieve this baseline as quickly as possible is required: eliminate any draughts from the room (close window and doors where possible) and heat the room to above 23°C (term babies) or 25°C (preterm babies).
Once delivered, dry the baby immediately and then wrap in a warm, dry towel. In addition to increased mortality risk, a cold baby has an increased rate of oxygen consumption and is more likely to become hypoglycaemic and acidotic. If this is not addressed at the beginning of resuscitation it is often forgotten. Most heat loss at delivery is caused by the baby being wet (evaporation) and in a draught (convection). Babies also have a large surface area-to-weight ratio exacerbating heat loss. Ideally an overhead heater or external heat source should be available and switched on, but drying effectively and wrapping the baby in a warm dry towel with the head covered, ideally by a hat, is the most important factor in avoiding hypothermia. A naked dry baby can still become hypothermic despite a warm room and a radiant heater, especially if there is a draught. In all babies, the head represents a significant part of the baby’s surface area (see ‘Preterm babies’ below) so attention to providing a hat is invaluable in maintaining normothermia.
Out of hospital: Babies born at all gestations outside the normal delivery environment may benefit from placement in a food grade polyethylene bag or wrap after drying and then swaddling. Alternatively, well newborn babies >30 weeks gestation who are breathing may be dried and nursed with skin-to-skin contact (or kangaroo mother care) to maintain their temperature whilst they are transferred. Exposed skin should be covered to protect against cooling draughts.
Assessment of the newborn baby
During and immediately after drying and wrapping the baby, make a full assessment as outlined below.
| A/B | • Breathing | Regular, Gasp, None |
| C | • Heart rate | Fast, Slow, Very Slow/Absent |
| C | • Tone | Well Flexed, Reduced Tone, Floppy |
Unlike resuscitation at other ages, all three items need to be assessed in parallel to be able to then decide on need for resuscitation and begin treatment and then assess its effect. This is different to the linear hierarchy of assessment and treatment used at other ages. In the newborn baby, heart rate and breathing provide the most useful information and are the only items which need regularly reassessing during resuscitation to assess effectiveness of intervention. At the initial assessment, however, taking note of the baby’s tone can also be informative: a baby who is very floppy is likely to be unconscious, suggesting that the baby may have been subject to hypoxia.
Colour, while no longer formally assessed, is still a potentially useful indicator of status. Normal babies are born ‘blue’ and become ‘pink’ in the first minutes of life. A baby who is pale and white (‘shut down’ due to intense peripheral vasoconstriction) is more likely to be acidotic: this sort of appearance suggests significant cardiovascular response to peripartum compromise.
Breathing movements and colour can be determined by observation during drying; tone can be evaluated whilst in the act of drying the baby. Heart rate is determined by auscultation of the heart using a stethoscope: this can be done during the drying by a second person or immediately afterwards if there is a lone responder.
Breathing
Most well term babies will take their first breath 60–90 seconds after delivery and establish spontaneous regular breathing sufficient to maintain the heart rate ≥100 beats/min within 3 minutes of birth. If there is no breathing (apnoea), gasping or irregular ineffective breathing that persists after drying, intervention is required.
Heart rate
In the first couple of minutes, auscultating at the cardiac apex is the best method to assess the heart rate. Palpating peripheral pulses is not practical and is not recommended. Palpation of the umbilical pulse can only be relied upon if the palpable rate is ≥100 beats/min. A rate less than this should be checked by auscultation, and it may not be possible to feel a cord pulse when there is a heart rate that can be detected by auscultation.
In delivery suites, saturation monitors using Masimo (or similar) technology are now widely used by NICU teams when resuscitation is required at term, or when preterm babies have been delivered. However, applying a saturation monitor should not interrupt the process of resuscitation. It is also good practice to correlate the probe reading (heart rate), once good detection signal strength is achieved, with the auscultated heart rate. An ECG, if available, can give a rapid accurate and continuous heart rate reading during newborn resuscitation. In low-resource or non-specialist settings (especially if the only saturation monitor probe available is designed to fit a larger child or adult) the use of a stethoscope is recommended to allow resuscitation to proceed without delay.
The probe for the saturation monitor must be applied to the right (not left) hand or wrist in order to accurately reflect the preductal saturations (which are most likely to reflect the oxygenation of blood returning to the left atrium and that which is being distributed to the coronary arteries and cerebral circulation). A correctly applied pulse oximeter can give an accurate reading of heart rate and saturations within 90 seconds of application. Oxygen saturation levels in healthy babies in the first few minutes of life may be considerably lower than at other times (See Figure 12.4). Attempting to judge oxygenation by assessing colour of the skin or mucous membranes is not reliable, but it is still worth noting the baby’s colour at birth as well as whether, when and how it changes later in the resuscitation. Very pale babies who remain pale and bradycardic after resuscitation may be hypovolaemic as well as acidotic. Similarly, tone immediately at birth should be assessed, and then changes noted as resuscitation progresses.




