• End-stage renal disease.
• Acute kidney failure accompanied by 1 or more of the following:
• Oliguria or anuria.
• Uremia (azotemia accompanied by platelet dysfunction and bleeding, change in mental status, or other uremic symptoms).
• Electrolyte or metabolic disturbance unresponsive to medical management (eg, hyperkalemia, hyponatremia or hypernatremia, acidosis, hypocalcemia, hyperphosphatemia).
• Inability to provide adequate nutrition or other intravenous therapy due to fluid restriction.
• Inborn error of metabolism: urea cycle disorders, propionic acidemia, maple syrup urine disease (hemodialysis and CRRT more effective and are preferred).
• Dialyzable toxin (hemodialysis and CRRT more effective and are preferred).
• Lack of adequate peritoneal membrane or cavity.
• Omphalocele.
• Diaphragmatic hernia.
• Gastroschisis.
• Recent abdominal surgery.
• Prior extensive abdominal surgery that might have resulted in adhesions or peritoneal scarring.
• Ventriculo-peritoneal shunt.
• Unsuitable social situation for home dialysis.
• Peritoneal dialysate solutions.
• Lactate-buffered, electrolyte-balanced dextrose solution most often used.
• Available as 1.5%, 2.5%, and 4.25% dextrose.
• Bicarbonate-buffered solutions are available.
• Icodextrin (glucose polymer) solution available; useful for patients with poor fluid removal.
• Solution warmer (blood transfusion warmer for continuous ambulatory peritoneal dialysis [CAPD] or warming tray on cycler).
• Automated cycler for intermittent peritoneal dialysis (IPD) or continuous cycling peritoneal dialysis (CCPD) or manual exchange set for CAPD.
• Peritoneal dialysis catheter.
• Surgically placed permanent catheter preferred in most situations.
• Temporary percutaneous catheter in unstable patients or per center preference for acute kidney failure.
• Peritoneal dialysis is the preferred method of chronic dialysis in children with end-stage renal disease.
• Children receiving peritoneal dialysis have less daytime disruption of school and social activities.
• Because peritoneal dialysis is performed every day, a more liberal fluid and dietary regimen is possible.
• Peritoneal dialysis might be the only option available to small infants who cannot tolerate the large fluid shifts and large extracorporeal circuit volume of hemodialysis, and to those patients who do not have adequate vascular access for hemodialysis.
• However, hemodialysis might be the only option for RRT for those children who have had extensive abdominal surgery, who have a social situation that precludes home dialysis, or in whom peritoneal dialysis has already failed due to repeated bouts of peritonitis or other complications.
• Hemodialysis and CRRT remain the treatments of choice for inborn errors of metabolism and toxic ingestions because peritoneal dialysis does not provide efficient and rapid clearance of metabolites and toxins.
• Renal replacement therapy (RRT) refers to any procedure whereby solute or water, or both, are removed from the body, generally during acute or chronic kidney insufficiency. • RRT can be divided into intermittent or continuous therapies.
|
• Educate and train family to use home dialysis in patients with end-stage renal disease.
• Counsel patients with end-stage disease extensively about long-term dialysis options (hemodialysis vs. peritoneal dialysis) and advantages, disadvantages, and risks of each option.
• Before starting peritoneal dialysis, a peritoneal dialysis catheter must be placed.
• After insertion, a healing period of several weeks or longer may be needed.
• Catheter can be used immediately for urgent dialysis, but there is a risk of increased rates of leakage and peritonitis.
• Surgical placement of the catheter is preferred.
• However, the catheter can be placed percutaneously at the bedside in unstable patients.
• The peritoneum consists of connective tissue covered by mesothelium.
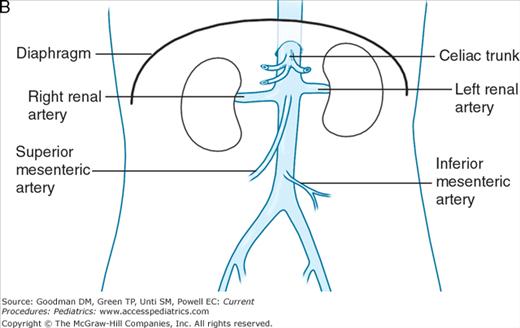
• The visceral peritoneum covers the intraperitoneal organs and receives its arterial blood supply from celiac, superior mesenteric, and inferior mesenteric arteries (Figure 68–1).
• The parietal peritoneum lines the inner abdominal and pelvic walls and the diaphragm and receives its arterial blood supply from adjacent structures.
• Venous drainage of the peritoneum occurs via the portal vein.
• Dialysate fluid is instilled into the peritoneal cavity via a peritoneal dialysis catheter manually or by automated cycler.
• Dialysate fluid is drained into a drainage bag and the peritoneal cavity is refilled with fresh fluid at regular intervals.
• Dialysis prescription is individualized for each patient regarding:
• Modality (eg, CAPD, CCPD, IPD).
• Type and concentration of dialysis solution.
• Volume of fluid (fill volume).
• Length of time in abdomen (dwell time).
• Number of cycles.
• Total treatment time.
• Additives to dialysis solution (potassium, heparin, antibiotics, amino acids).
• The peritoneal dialysis solution generally contains a prescribed concentration of dextrose (1.5, 2.5, or 4.25%)and a fixed amount of electrolytes and buffer (sodium chloride, lactate, magnesium, and calcium).
• The concentration of dextrose provides an osmotic gradient for movement of water from the blood vessels lining the peritoneal cavity into the dialysate solution, which then is drained.
• Adjustment of dextrose concentration, dialysate volume, number of cycles, and length of time the solution remains in the peritoneal cavity affect the removal of solute and water.
• For acute kidney failure, the following should be monitored carefully:
• Fluids and electrolytes.
• Strict intake and output.
• Daily weight.
• Blood pressure and vital signs.
• For long-term peritoneal dialysis, the following may be monitored at home:
• Total fluid drainage.
• Daily weight.
• Peritonitis.
• Bleeding.
• Perforation of bladder or other viscera by dialysis catheter.
• Pain.
• Dialysate leakage.
• Catheter obstruction.
• Electrolyte imbalance.
• Respiratory compromise due to increased intraperitoneal pressure or hydrothorax.
• Hypotension.
• Hypoalbuminemia from loss of protein into dialysate.
• Hyperglycemia, especially with higher dextrose concentrations.
• Inguinal or umbilical hernia.
• For acute kidney failure, as indicated following discontinuation of dialysis.
• For end-stage renal disease, regular follow-up (about once a month) by an experienced nephrologist and peritoneal dialysis nurse is required to manage dialysis prescription, complications, and other aspects of end-stage kidney disease.