Three essential attributes of renal function:
Glomerular ultrafiltration
Tubular absorption of filtered solutes and water
Tubular secretion of organic and nonorganic ions
General: malaise and growth failure
Gastrointestinal (GI): feeding difficulties, vomiting, anorexia, and GI bleeding at times
Asymptomatic in many cases
Neonatal history
Prenatal diagnosis of hydronephrosis or urinary tract abnormality
Edematous/hypertrophied placenta (>25% of birth weight) suggests congenital nephrotic syndrome.
Maternal infection. Congenital TORCH infections can present as neonatal nephrotic syndrome and seeding of renal parenchyma with infections (e.g., cytomegalovirus); maternal sepsis can cause hypoperfusion and injury to the infant’s kidneys.
Perinatal asphyxia with macroscopic hematuria in neonatal period might suggest renal venous thrombosis in the same child with hematuria when older.
Family history: inherited renal conditions such as cystic kidney diseases (ARPKD, ADPKD, nephronophthisis), thin basement membrane disease, Alport syndrome, and some nephrotic syndromes because of inherited mutations. Specific inquiry regarding any family member on dialysis or with a kidney transplant is often insightful.
Past medical history: recurrent gross hematuria (IgA nephropathy), intermittent swelling, high blood pressure, medication exposures, and daytime or nocturnal enuresis
Dietary history
Growth and nutrition
Hydration status (edema or dehydration)
Circulation, including four extremity pulses, precordium, lungs (pulmonary edema), and abdominal palpation
Physical examination
Maintain a broad focus in newborns, as many renal diseases are associated with other congenital defects (imperforate anus, VACTERL association, single umbilical artery, gonadal dysgenesis, and Wilms tumor).
Palpate the abdomen for renal masses (enlarged kidney in renal vein thrombosis, renal tumors, and multicystic dysplastic kidneys).
Abnormalities of appearance
Hematuria (confirm with urinalysis and microscopic examination)
Cloudy: suggestive of infection/crystalluria
Abnormalities of urine volume
Anuria: complete cessation of urine output
Oliguria: insufficient urine for homeostasis (usually <500 mL/24 hr for adults or 1 mL/kg/hr in infants). See Table 24-1 for laboratory values that indicate a prerenal or renal cause.
Polyuria: increased fluid intake, failure of antidiuretic hormone (ADH) release, resistance to ADH, and osmotic diuresis
Blood: tests for heme moiety (hemoglobin and myoglobin). If positive, it is necessary to confirm red blood cell (RBC) morphology by microscopic examination.
Protein: standard Clinistix detects albumin; less sensitive for free light-chain proteins (Bence Jones) or low-molecular-weight “tubular” proteins
Glucose: standard Clinistix detects glucose alone; to test for other sugars, a Clinitest is necessary.
Nitrite: 90% of common urinary pathogens are nitrite-forming bacteria.
Urinary concentration: tested by specific gravity, but osmolality is more accurate with large molecules such as glucose
Urine bilirubin: elevated in any disease that causes increased conjugated bilirubin in the bloodstream (negative in hemolytic disease)
Urine urobilinogen: increased in conditions that increase the production of bilirubin or decrease the liver’s ability to remove reabsorbed urobilinogen from the portal circulation (positive in both liver disease and hemolytic disease)
Microscopic examination
In healthy children, 1-2 RBCs/high-power field (HPF) or 1-2 white blood cells (WBCs)/HPF is normal.
Casts: precipitation of debris in renal tubules
Hyaline casts: low renal blood flow
Red cell casts: hematuria of glomerular origin suggestive of glomerulonephritis
Fatty casts (Maltese-cross structures): commonly seen in nephrotic syndrome
Crystals
Calcium oxalate: hypercalciuria (envelope or dumbbell shape of crystals)
Uric acid crystals: hyperuricosuria (appear as rhombic plates or rosettes)
Hexagonal (benzene ring structure) cystine crystals: cystinuria
Ammonium magnesium phosphate crystals: only form in alkaline pH; seen with urease-splitting organisms (coffin-lid appearance of crystals)
Fine, needle-like crystals: tyrosinemia
TABLE 24-1 Laboratory Differentiation of Oliguria | |||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||
Schwartz formula: used to calculate the glomerular filtration rate (GFR) mL/min/1.73 m2
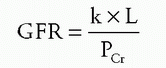
L = length in cm
k = constant of proportionality
Full-term newborn through first year: 0.45
Children up to 13 years: 0.55
Adolescent males (13-21 years): 0.7
Adolescent females (13-21 years): 0.57
Child with chronic kidney disease: 0.413
PCr = plasma creatinine
Blood urea nitrogen (BUN): not an accurate predictor of renal function
Factors that increase serum BUN: GI hemorrhage, dehydration, increased protein intake, and increased protein catabolism (systemic infection, burns, glucocorticoid therapy, early phase of starvation)
Factors that decrease serum BUN: high fluid intake, decreased protein intake, advanced starvation, and liver disease
Calculation of GFR using U × V/P
To standardize: creatinine clearance
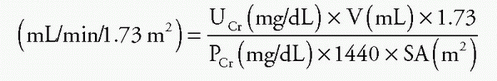
UCr = urinary concentration of creatinine
V = urine volume in 24 hours
PCr = plasma concentration of creatinine
SA = body surface area
If a child >3 years of age has <15 mg/kg/day of creatinine in a 24-hour urine collection, it probably means that the collection did not actually occur over 24 hours or that not all the urine has been collected.
For normal values of GFR, see Table 24-2.
Renal function can be categorized as glomerular, tubular, or hormonal (Table 24-3).
TABLE 24-2 Normal Glomerular Filtration Rate (GFR) by Age | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Defined as an increase in creatinine of 0.5 mg/dL over the baseline
TABLE 24-3 Summary of Diagnostic Renal Evaluation by Function | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Acute tubular necrosis (ATN): 45% (ischemia or nephrotoxins)
Prerenal: 21% (heart failure, sepsis, or volume depletion)
Acute on chronic: 13% (mostly ATN and prerenal disease)
Urinary tract obstruction: 10%
Glomerulonephritis or vasculitis: 4%
Acute interstitial nephritis: 2%
Serum BUN/creatinine ratio (use with caution in children)
Prerenal >20:1
Other causes of high BUN: GI bleed, steroids, and tetracycline
Other causes of low creatinine: reduced muscle mass in chronically ill children
Urinalysis
Prerenal: hyaline casts
Intrinsic renal disease: RBCs and WBCs, granular/RBC/WBC casts, or renal epithelial cells
Urine sodium concentration
Prerenal: <20 mEq/L
Intrinsic disease: >40 mEq/L
Fractional excretion of Na (FENa) = (UNa·Cr)/(PNa·UCr) × 100
Prerenal: <1%
ATN: >2%
Unequivocal if 1%-2%
Not useful if patients are taking diuretics
Fractional excretion (FE) of urea = (Uurea·PCr)/(Purea·UCr) × 100
Prerenal: <35%
Intrinsic: >60%-65%
Urine osmolality
Prerenal: >500 mOsmol
Intrinsic: <450 mOsmol
Urine-to-plasma creatinine concentration
Prerenal: >40
Intrinsic: <20
Increased anion gap
An increase in unmeasured anions: diabetic ketoacidosis; lactic acidosis; uremia; and ingestion of salicylates, ethylene glycol, and methanol
Severe diarrhea can also cause an increased anion gap acidosis in children and infants.
Normal anion gap
GI bicarbonate loss (diarrhea, intestinal/pancreatic fistulas, resins)
Renal tubular acidosis (RTA)
Type I: defective proton (H+) secretion
Type II: defective HCO3 reabsorption
Type IV: hypoaldosteronism
Tests for diagnosis of RTA (Table 24-4)
Urine pH
pH: <5.5 proximal type I and type IV
pH: >5.5 distal type I
Urine ammonia levels: low in distal type I
Urine anion gap (urine sodium + potassium + chloride)
Negative in proximal type I
Positive in distal type I and type IV
TABLE 24-4 Types of Renal Tubular Acidosis | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|



