Renal
Shana McCormack
Paritosh Prasad
Avram Z. Traum
Urinalysis
Evaluation
(Pediatr Clin North Am 2006;53:325)
| Urine Dipstick Test Finding | Nonpathologic Causes | Pathologic Causes |
|---|---|---|
| Specific gravity (low) | Polydipsia | DI, renal tubular dysfunction |
| Specific gravity (high) | Inadequate volume intake | Volume depletion |
| pH (low) | High-protein diet | Acidosis |
| pH (high) | Low-protein diet; recent meal | RTA (inappropriate renal response); UTI (ie. Proteus) |
| Blood present (can represent RBCs, Hgb, myoglobin) | Menses, traumatic catheterization, exercise | Glomerular d/o, tubular d/o, UTI, stones, hypercalciuria, urinary tract trauma, tumor rhabdo, hemolysis |
| Protein present | Orthostatic proteinuria, fever, exercise | Glomerular disorders, tubular disorders, UTI |
| Glucose present | Renal glycosuria (SGLT2 transporter defect) | Diabetes mellitus, Fanconi anemia |
| Ketones | Restricted carbohydrate intake | Diabetes mellitus starvation, EtOH |
| Bilirubin present | None | Hepatitis, biliary obstruction |
| Urobilinogen present | Low amounts: systemic Abx Rx | Hepatitis, intravascular hemolysis |
| Nitrite present | None | UTI (Enterobacteriaceae only), bacturia |
| LE present (from PMNs) | Fever | UTI, glomerulonephritis, pelvic inflamm, sterile pyuria |
Urine protein/Cr ratio correlates w/ total daily protein excretion based on g/1.73 m2 BSA. Low Cr in cachectic child or ↓ muscle mass (e.g., myopathy, myelomeningocele) may overestimate ratio. Nml ratio <0.2 mg protein/mg Cr.
Urine albumin/Cr ratio correlates w/ excretion of albumin in timed sample. Ratio >30 mg/g Cr abn. (Nml albumin excretion <20 mg/d), and microalbuminuria defined as 30–300 mg/d, and not typically detected on U/A.
Urine calcium/Cr ratio correlated w/ excretion of Ca++ in a timed sample. Nml ratio depends on age; in school-aged children and adolescents, should be <0.21.
Acute Renal Failure
Definition
(Adolesc Med Clin 2005;16:1)
Sudden onset, inadeq renal fxn to clear metab waste, maintain nml fluid and electrolyte balance. May be oliguric (30%) or urine output may be nml to ↑ (70%).
Epidemiology
(Pediatr Rev 2002;23:47; Am J Kidney Dis 2005;45:96)
Epidemiology of renal failure changed in face of advances in pediatric ICU care, congenital heart surgery, and pediatric oncology/bone marrow transplantation.
Previously intrinsic renal disease was felt to be the most common cause of ARF
Now ARF is most commonly found as a morbidity assoc w/ other systemic illness
Retrospective review at 3° care pedi hospital w/ most common causes ARF to be renal ischemia (21%), nephrotoxic medications (16%), and sepsis (11%).
In developing countries, 3 most common causes of ARF are: Hemolytic-uremic syndrome (31%), glomerulonephritis (23%), prerenal ischemia (18%)
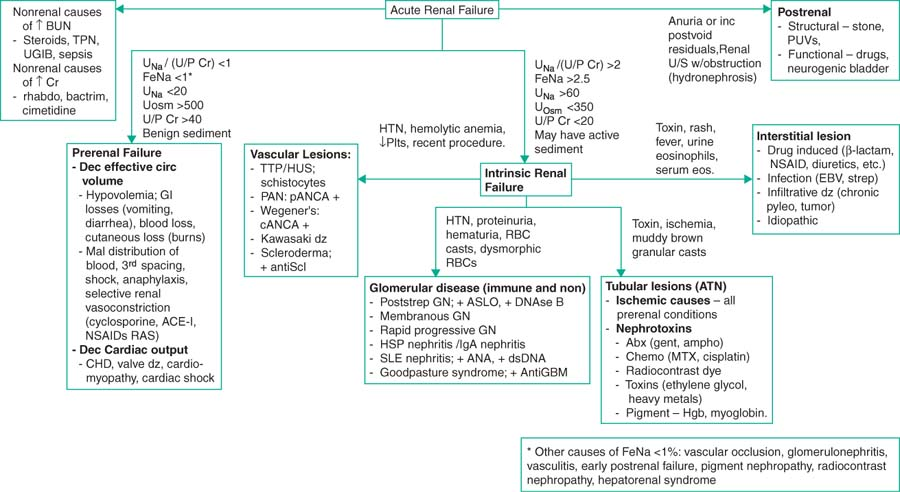 |
Etiology
(Adolesc Med Clin 2005;16:1)
Pre-renal: renal hypoperfusion (intravasc volume loss 2/2 dehydration, trauma, capillary leak from sepsis/burns/nephrotic syndrome, poor cardiac function)
Post-renal: structural/obstructive causes (rare, 2/2 pelvic mass or ureteral obstruct)
Intrinsic-renal: underlying kidney injury or dz
Endogenous toxins: Hgb, myoglobin, or uric acid in tumor lysis
Exogenous toxins: NSAIDs, Abx, antifungals, chemo, contrast, ACE-I in some
Allergic rxn/interstitial nephritis
Infxn: Pyelo, postinfectious syndromes, such as post-Streptococcal GN or HUS
Immune-mediated vasculitides: SLE, polyarteritis, Wegener, Goodpasture
Vascular; renal artery or vein thrombosis of a single or transplanted kidney
Diagnostic Evaluation
(Pediatr Rev 1995;16:101; Pediatr Rev 2002;23:47)
Complete H&P focused on narrowing the above differential
Initial labs: U/A w/ microscopy & culture, CMP, CBC, sediment
Fractional excretion (FE) Na = (PCr × UUN)/(BUN × UCr) (inaccurate w/ diuretics)
PCr is plasma conc of Cr; PNa is plasma conc of Na
UCr is urinary conc of Cr, and UNa is urinary conc of Na.
FENa <1%; ↓ renal perfusion, w/ hypovolemia, low cardiac output states.
FeNa >2%; spilling Na, makes intrinsic renal dz more likely (i.e., ATN).
FE Urea = (PCr × UUN)/(BUN × UCr); <35%–40% prerenal (use if on diuretics)
Glomerular filtration rate (mL/min/1.73 m2) calculated as length (cm) × (K/plasma Cr conc), (K is coefficient 0.45 for <1–12 mo; 0.55 for 2–12 yo and older girls, and 0.7 for boys 13–18 yo via the Schwartz formula.
Creatinine clearance (CrCl) is a surrogate marker of GFR.
Consider: Albumin, cholesterol, serum complement, antinuclear Ab, streptococcal serologies, blood and stool cultures, toxicology screen
Imaging may include ultrasound, CT, MRI/MRA; biopsy may be indicated
Therapy
(Adolesc Med Clin 2005;16:1)
Etiology dependent; please see sections on specific dx under proteinuria/hematuria
Monitor BP, volume status, serum chemistries (specifically, ARF produces hyperkalemia, as the kidneys are responsible for 90% of renal potassium excretion) and acid-base status (specifically, ARF produces metabolic acidosis)
Avoid nephrotoxic agents and dose all meds according to estimated CrCl
Renal replacement Rx (dialysis, CVVH) indicated for life-threatening volume overload, hyperK, hypoNa, metabolic acidosis refractory to medical mgmt, complications of uremia (pericarditis, encephalopathy), or to clear toxins
Prognosis
(Arch Pediatr Adolesc Med 2002;156:893)
Dependent on underlying etiology, much worse if multiorgan involvement; >50% mortality if three or more organs are involved
Chronic Renal Failure
Definition
(Pediatr Nephrol 2003;18:796)
Chronic renal insufficiency is defined as CrCl <75 mL/min/1.73 m2.
Etiology
(Pediatr Nephrol 2003;18:796)
∼40% w/ congenital urologic anomalies.
Causes of CRI (↓ order prevalence): Obstructive uropathy, aplastic/hypoplastic/dysplastic kidneys, reflux nephropathy, FSGS, polycystic kidney dz, immunologic dz, syndrome of agenesis of abd musculature, renal infarction, HUS, cystinosis, others, unknown.
Complications
(Pediatr Nephrol 2003;18:796)
Infections prompt 45% of hospital admissions in one series.
Other potential complications include: Anemia, hypertension bone disease.
Short stature is common (one series shows delay of -1.4 SD at the time of registry to a CRI database); recombinant growth hormone is one possible therapy.
Prognosis
(Pediatr Nephrol 2003;18:796; J Am Soc Nephrol 2005;16:2796)
Proteinuria, low Hct, hypoalbuminemia, hypoCa, hyperphos, hyperPTH all assoc w/ rate of progress to ESRD, as is age at dx and the dx itself.
Rx of anemia, hypoCa, and hyperphos leads to improved outcomes in the short-term
Cardiac and vascular abn (LVH, diastolic dysfxn, ↑ carotid intima-media thickness) are progressive and may be related to ↑ calcium-phosphorus product.
Glomerular disorders, including FSGS, increase risk of progression to ESRD.
Secondary Hypertension
Definition
(Pediatr Rev 2007;28:283)
2° HTN (BP >95th percentile for age and ht) – ↑ BP 2/2 underlying, identifiable cause
Etiology and Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


