CHAPTER 12 Rehabilitation concepts for pediatric brachial plexus palsies
Summary box
Initial evaluation and intervention
Physical examination of the infant should include the following: general inspection, weight, length, head circumference and growth percentiles, examination of both legs including hips, examination of both arms, observation of respiratory pattern and movement of the chest, observation for any signs of pain at rest or while the infant is being examined. Particular attention should be paid to examining the eyes for Horner’s sign (ptosis, meiosis, and anhydrosis; Figure 12.1), and to the resting position of the neck in the supine and prone resting positions for torticollis and during active and passive movement. Is neck strength normal for the patient’s age? In addition, examination of the affected arm should include observation in the resting position for classic postures of NBPP (eg, Waiter’s tip; Figure 12.2), testing passive and active ranges of motion, recording lengths and circumferences of all segments of the upper extremity, and estimation of motor power of the arm and hand.
At the end of the examination, the following questions should be answered and recorded (Table 12.1):
Table 12.1 Examination record for patients with neonatal brachial plexus palsy
| Affected arm |
| Infant reflexes |
| Feeding |
| Interaction with environment |
Initial rehabilitation management
A common presentation for the infant with NBPP (primarily affecting the upper trunk) is a weak or limp arm positioned in an internal rotation with the shoulder adducted, elbow extended, forearm pronated, and fingers and wrist flexed (Figure 12.2). As the nerves of the brachial plexus regenerate, motor function recovers. The course of recovery for an infant with an upper trunk (Erb’s) palsy includes slight shoulder flexion (often derived from the pectoralis muscle), enough to flex the shoulder to allow gravity to seemingly flex the elbow. Gradually, the infant learns to extend the wrist (Steindler effect) or flex the fingers to aid and/or augment elbow flexion (Figure 12.4). The focus of therapy with infants at this point is to facilitate shoulder flexion, particularly by abduction with external rotation at the shoulder, and elbow flexion against gravity. The timing for nerve repair/reconstruction varies within the surgical community, ranging from 3 months to 9 months of age. Most practitioners agree that recovery of shoulder flexion and abduction followed by elbow flexion against gravity beginning by <3 months of age obviates the need for surgical intervention. If clinical, electrodiagnostic, and radiographic data are consistent with nerve root avulsion injury, nerve repair/reconstruction may be recommended as early as 3 months of age.
The most important goal of therapy for NBPP patients is maintenance of soft tissue and joint flexibility. Passive range-of-motion exercises are critical and must be taught to the parents/caregivers to be performed routinely at home.1 These exercises can be performed safely and effectively to gently stretch the relevant muscles and joint structures to avoid development of contractures (resulting from excessive contraction of the functioning muscles that are not counterbalanced by the paretic muscles).
Children with NBPP risk developing skeletal deformities of the trunk and affected extremity due to poor bone growth associated with weakness of certain muscles, unopposed activities of other muscles, or muscle imbalance (Figure 12.5).2 Poor bone growth is a direct result of decreased weight-bearing coupled with lack of muscle tension upon areas of the bone that contribute to bone growth.
Infants
In the newborn period, the initial evaluation should ascertain the presence of clavicle or humeral fractures, respiratory problems, or other difficulties. In one study, 1 in 11 newborns with a clavicle fracture also had NBPP.3 In addition to evaluation of arm function, assessment should also be made of oral motor skills and feeding, head control, and head positioning. In an unpublished study, 43% of children under 6 months of age with NBPP also had torticollis.4 Feeding difficulties may be due to birth asphyxia, facial nerve injury, or breathing problems, including phrenic nerve injury.5
In healthy newborns with brachial plexus palsy, it is important to educate the parents on passive range-of-motion exercises for all muscle groups. These exercises should be performed at every diaper change. Additionally, parents should be educated regarding the need for “tummy time” at each diaper change to promote symmetrical head rotation and positioning. Torticollis is an abnormal head posture including ipsilateral tilt, contralateral rotation and translation,6 and it is the third most common pediatric orthopedic diagnosis in childhood.7 Persistent torticollis may lead to plagiocephaly and facial asymmetry; deformational plagiocephaly can be appreciated as early at 6 weeks of age with a preexisting diagnosis of torticollis.8 The major cause of deformational plagiocephaly is limited head mobility in early infancy secondary to cervical imbalance.9 For infants with torticollis, parents should be encouraged to vary the position of the infant’s head during play, feeding, and sleeping. Use of positioning wedges may be helpful. Home programs using neck stretches to address tightness of the sternocleidomastoid muscle may be required for some infants and should be taught to families by appropriately trained therapists.
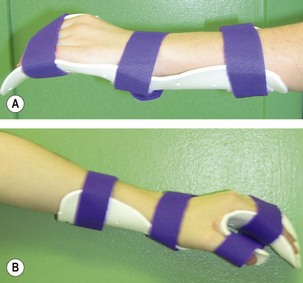
In some instances, a newborn will require a hand/elbow splint prior to discharge from the hospital. The indications for a hand splint are tightness of the finger joints and/or significant atrophy of the thenar eminence. If Horner’s sign is present, significant atrophy of the thenar eminence is usually present and indicates the need for a resting hand splint. The preferable position for a resting hand splint would be the intrinsic plus position (Figure 12.6). In the intrinsic plus position, the metacarpophalangeal joints are flexed at 60–70 degrees, the interphalangeal joints are fully extended, and the thumb is in partial abduction and flexion or opposed to the extended interphalangeal joint of the index finger. The wrist is held in extension at 10 degrees less than maximal.
Infants with NBPP learn quickly to adapt to their development with a unilateral bias. Progression toward symmetrical development begins with learning to roll prone to supine and back to both right and left sides. A similar approach can be applied when the child moves from supine to sitting position. Once a child has learned to transition into sitting, progression to 4-point positioning is appropriate. The strength and coordination required to sustain and/or reach from the point position is a precursor to crawling. Some infants master the “commando crawl” while others will not learn to crawl and will progress directly from sitting to walking. Therapy techniques to facilitate crawling include the use of elbow supports/splints, weight-bearing hand and/or wrist splints, shoulder support splinting or taping techniques, or use of positioning techniques9 combined with vibration or, in some situations, neuromuscular electrical stimulation. Protective reactions in the affected extremity are often delayed or weak, yet they must be a focus of therapy. A small therapy ball can be used to develop forward protective reactions in prone and sitting positions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree