CHAPTER 21 Rehabilitation concepts for adult brachial plexus injuries
Summary box
Anatomy and physiology
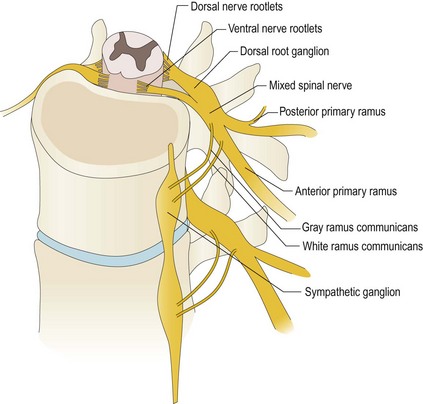
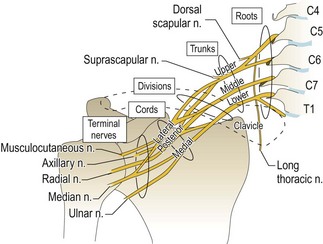
The brachial plexus is commonly formed from the C5 through T1 nerve roots and extends from the spinal cord to the axilla. The plexus may be pre-fixed or post-fixed and receive contributions from the C4 or T2 nerve roots respectively. There are five separate identifiable sections of the brachial plexus: roots, trunks, divisions, cords, and terminal branches or nerves. The dorsal and ventral rootlets exit the spinal cord and fuse to form the dorsal and ventral roots (Figure 21.1). The percentage of sensory and motor fibers composing each root varies. The largest percentage of motor fibers is found in the C5 and C6 roots; C7 and T1 have the least. The greatest number of sensory fibers is found in the C7 root, followed in descending order by C6, C8, T1, and C5. The brachial plexus also carries sympathetic fibers. The dorsal root ganglion is comprised of the cell bodies of the sensory nerves and lies within the confines of the spinal canal and foramen.
The C5 and C6 roots merge to form the upper trunk and the C8 and T1 roots merge to form the lower trunk. C7 becomes the middle trunk. The point at which C5 and C6 merge (Erb’s point) marks the location at which the suprascapular nerve emerges. Each trunk then divides into anterior and posterior divisions and passes beneath the clavicle. The posterior divisions merge to become the posterior cord, and the anterior divisions of the upper and middle trunk merge to form the lateral cord. The anterior division from the lower trunk forms the medial cord (Figure 21.2). The cords are named for their relationship to the second segment of the axillary artery, to which they are typically bound.
The posterior cord forms the axillary nerve and the radial nerve. The lateral cord splits into two terminal branches: the musculocutaneous nerve and the lateral cord contribution to the median nerve. The medial cord contributes to the median nerve as well as to the ulnar nerve.1
A few terminal nerve branches come off the roots, trunks, and cords of the plexus. The branches off the C5 root include a branch to the phrenic nerve, the dorsal scapular nerve (rhomboid muscles), and the long thoracic nerve (serratus anterior muscle). The branches off C6 and C7 roots also contribute to the long thoracic nerve (serratus anterior muscle). The branches off the upper trunk include the suprascapular nerve (supraspinatus and infraspinatus muscles) and the nerve to the subclavius muscle. The lateral cord gives off the lateral pectoral nerve (pectoralis major); while the posterior and medial cords each have three branches. The posterior cord gives off branches (proximal to distal) that include the upper subscapular nerve, thoracodorsal nerve, and the lower subscapular nerve. The medial cord gives off the medial pectoral nerve, the medial antebrachial cutaneous nerve, and the medial brachial cutaneous nerve.2 By noting loss of function to these muscles, one can pinpoint the level of brachial plexus injury.
A preganglionic injury is when the spinal roots are injured proximal to the dorsal root ganglion and may be avulsed from the spinal cord. Preganglionic injuries can be separated into central avulsions, in which the nerve is avulsed directly from the spinal cord, and intradural ruptures, in which rootlets rupture proximal to the dorsal root ganglion. An injury distal to the dorsal root ganglion is called postganglionic. Distinguishing between a preganglionic and a postganglionic injury is important when considering the implications for prognosis. It is possible that traumatic brachial plexus injuries may include damage to both pre and post-ganglionic portions of the plexus, which can further complicate assessment of prognosis. There is little potential for spontaneous recovery of preganglionic avulsion injuries.3 These injuries will require some type of surgical intervention to improve function. A complete avulsion injury of all the roots contributing to the plexus has more limited options for surgical intervention to improve nerve function. Spontaneous recovery may occur following a postganglionic injury or may need surgery to improve function depending on the degree of injury (neurapraxia, axonotmesis, or neurotmesis).
Neurapraxia is a conduction block at the site of injury without macroscopic injury to the nerve. There may be a demyelinating injury, but Wallerian degeneration does not occur. As soon as the block is resolved, nerve function to the target organ will normalize. The recovery time may extend from hours to months, depending on the extent and severity of the injury to the myelin covering. Nerve conduction studies will show no conduction across the area of injury but will show normal sensory and motor conduction distal to the area of injury; this finding is unique to neurapraxias. In axonotmesis, the axon is disrupted, but the epineurium and perineurium remain intact. Wallerian degeneration will occur distal to the injury and generally will be complete over the course of 7 to 10 days. Regeneration from the surviving proximal axon stump is still possible and can occur at a rate of 1 to 4 mm per day.4 In neurotmesis, the entire nerve trunk is ruptured and axonal continuity is lost and spontaneous recovery will not occur. Without surgical intervention, this injury pattern will heal as a nonfunctional neuroma.
Classification of plexopathies
It is difficult to ascertain the number of brachial plexus injuries that occur per year. With the advent of extreme sports, high energy motor sports and increased numbers of individuals surviving motor vehicle accidents, the number is increasing. Most brachial plexus injuries occur in males aged 15 to 25 years. The rule of “seven seventies” is based on experience with over 1,000 patients with brachial plexus injuries. Approximately 70% of traumatic brachial plexus injuries occurred secondary to motor vehicle accidents; of these, approximately 70% involved motorcycles or bicycles. Of the cycle riders, approximately 70% had multiple injuries. Overall, 70% had supraclavicular lesions; of those, 70% had at least one root avulsed. At least 70% of patients with a root avulsion also have avulsions of the lower roots (C7, C8, or T1). Finally, of patients with lower root avulsion, nearly 70% will experience persistent pain.2,5
Brachial plexopathies are best classified according to the region involved, such as supraclavicular (root and trunks), retroclavicular (divisions), and infraclavicular (cords and terminal nerves) sites. Although this approach is anatomically simple, it has considerable clinical utility because the incidence, severity, prognosis, and lesion type vary among these regions.6
In general, supraclavicular plexopathies are more common, more frequently due to closed traction (which can produce lengthy lesions), usually more severe (because greater force is required to produce them), and typically associated with a worse outcome. The supraclavicular plexus is further divided into upper (C5 and C6 roots and upper trunk), middle (C7 root and middle trunk), and lower (C8 and T1 roots and lower trunk) portions; this is a clinically relevant distinction. Patients with upper trunk plexopathies tend to recover more completely because, in general, these lesions may more commonly have some degree of demyelinating conduction block, the muscles they innervate are in closer proximity, making recovery of muscle function more likely whether following spontaneous nerve regeneration or following surgical repair compared to those muscles innervated by the lower trunk of the plexus that have the worse recovery potential. The infraclavicular plexus is not subdivided because lesions affecting it do not show significant regional differences in incidence, severity, prognosis, or lesion type.1
Because most brachial plexopathies are axon loss in nature, neurologic examination frequently discloses weakness and sensory loss. With supraclavicular lesions, the pattern of sensory and motor loss is segmental—dermatomal and myotomal, whereas infraclavicular plexopathies produce nonsegmental patterns that resemble those observed with involvement of one or more terminal nerves.1
Patient evaluation
Physical examination
The physician should be suspicious of a brachial plexus injury when examining a patient with severe head, neck, shoulder girdle and proximal upper extremity injury. The examiner should record active and passive ranges of motion, sensory levels, as well as the presence or absence of reflexes. Acutely, inspection of the extremity should not demonstrate significant changes in muscle bulk or passive joint motion, but with time, atrophy of the involved muscles together with limitation of passive joint motion may become apparent. Detailed muscle testing of the shoulder girdle and upper extremity muscles of involved extremity should be compared to the opposite side. Table 21.1 summarizes key myotomes to examine.
Table 21.1 Cervical root and clinically relevant gross motor function
| C5 | Shoulder abduction, extension, and external rotation; some elbow flexion |
| C6 | Elbow flexion, forearm pronation and supination, some wrist extension |
| C7 | Diffuse loss of function in the extremity without complete paralysis of a specific muscle group, elbow extension, consistently supplies the latissimus dorsi |
| C8 | Finger extensors, finger flexors, wrist flexors, hand intrinsics |
| T1 | Hand intrinsics |
The distribution of absent muscle function, weakness or normal strength will help identify the site and extent of injury to the plexus (Table 21.1). A thorough knowledge of muscle anatomy is necessary to evaluate an upper extremity with plexus injury because residual muscle function may only be at Trace (or 1 MRC scale) levels that require precise localization and palpation of the muscle to assess for presence of a voluntary muscle contraction. Sensory examination is extremely important. The presence or absence of sensation should further help pinpoint the location and degree of involvement of the plexus. Deep pressure sensation may be the only clue to the continuity of a nerve with no motor function; testing can be made by by full pinch to the nail base and pull the patient’s finger outward. Any burning suggests continuity of the nerve tested. When no burning is elicited, these examination findings are less helpful because neurapraxia can persist for more than 6 months.4 Sensory examination of dermatomes to help identify a precise root level, however, can be unreliable because of overlap from other nerves or anatomic variation.
Certain findings suggest preganglionic injury on clinical examination. For example, the patient should be examined for the presence of Horner syndrome, consisting of miosis (small pupil), enophthalmos (sinking of the orbit), ptosis (lid droop), and anhydrosis (dry eyes), which is suggestive of a root avulsion at the C8-T1 level (Figure 21.3). Injury to the long thoracic nerve or the dorsal scapular nerve suggests a higher (more proximal) level of injury because both nerves originate at the root level. Elevation of the diaphragm on the side of injury suggests phrenic nerve involvement and proximal root level injury to the upper plexus.
When evaluating the patient with brachial plexus injury, it is important to consider additional points during the examination as these may have significant management and rehabilitation considerations. With head, neck and shoulder trauma resulting in plexus injury, there may be a concomitant spinal cord injury, and the trunk and lower limbs should be examined for the presence of altered strength, sensory levels, increased reflexes, and pathologic reflexes. Muscles innervated by nerves adjacent to but not originating from the brachial plexus should be evaluated, as the nerves supplying these muscles may have been injured as well. This includes the spinal accessory nerve innervating the trapezius and sternocleidomastoid, the phrenic nerve innervating the diaphragm and cervical plexus innervating the levator scapuli. Involvement of any of these nerves will have both functional and surgical management implications. It is also important to assess the vascular status of the involved upper extremity because injury to adjacent vascular structures such as the axillary artery can occur especially with infraclavicular plexus lesions.7
Rehabilitation of adults with brachial plexopathy
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree