CHAPTER 19 Reconstructive procedures for the upper extremity
Summary box
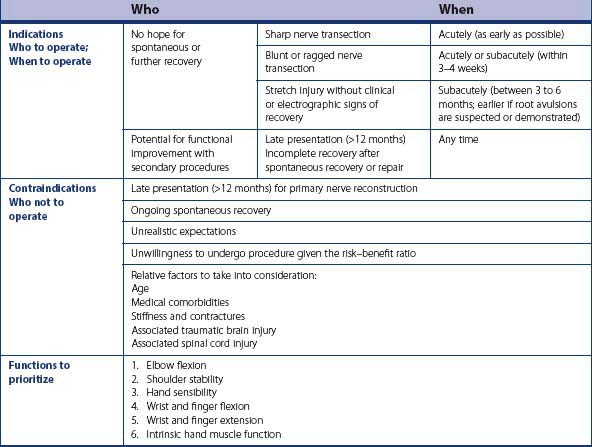
Indications/contraindications
The indications and contraindications for the reconstruction of upper extremity function after a brachial plexus injury are summarized in Table 19.1 and can be divided into 3 concepts: who to operate, when to operate, and the priority of functions depending on the nature of the brachial plexus injury.
Priorities for functional reconstruction
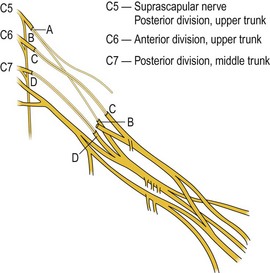
In all these situations, if post-ganglionic neuromas conducting nerve action potentials are found at exploration, neurolysis is done; on the other hand, when nerves are found at exploration to be ruptured or to have a postganglionic neuroma not conducting a nerve action potential, interpositional grafts are typically performed between the proximal nerve and specific targets. We routinely use intraoperative electrodiagnostic assessment to confirm the proximal nerve integrity (i.e. preservation of somato-sensory and motor-evoked potentials). Generally, C5 is used to target shoulder stability/abduction (suprascapular nerve, axillary nerve, or posterior division of upper trunk), C6 to target elbow flexion (anterior division of upper trunk, or musculocutaneous nerve), and C7 to target elbow extension (posterior division of middle trunk, or radial nerve) (Figure 19.1). When proximal nerves are found to be avulsed or have significant preganglionic injuries, different options are available depending on the brachial plexus injury pattern as described below (see Table 19.2).
Table 19.2 Common reconstructive options
| Type of brachial plexus injury | Nerve axon donor | Common targets |
|---|---|---|
| Any injury with neuroma-in-continuity conducting NAP | Neurolysis | |
| Any injury with nerve rupture or post-ganglionic neuromas not conducting NAP and good proximal nerves (preserved SSEP and MEP) | Direct repair or repair with graft if possible | |
| C5 nerve | Shoulder stability, abduction, and external rotation: Suprascapular nerve Axillary nerve Posterior division of UT | |
| C6 nerve | Elbow flexion: Anterior division of UT Musculocutaneous nerve | |
| C7 nerve | Elbow extension: Posterior division of MT Radial nerve | |
| Complete C5–T1 panplexus injury | Nerve transfers: XI | Suprascapular nerve Musculocutaneous nerve Free functioning muscle |
| Motor ICN | Musculocuatenous nerve Motor branch to the biceps | |
| Sensory ICN | Lateral cord contribution to the median nerve | |
| Other potential donors: Phrenic nerve Contralateral C7 nerve | ||
| C5–C6–C7 and C5–C6 Additional options | Ulnar nerve fascicle(s) | Motor branch to the biceps |
| Median nerve fascicle(s) | Motor branch to the brachialis Motor branch to the biceps | |
| C5–C6 Additional options | Triceps motor branches from radial nerve | Axillary nerve proper Anterior division of axillary nerve |
| Other potential donors: Medial pectoral nerves Ipsilateral C7 nerve | ||
| C8–T1 Options | Tendon transfers Selective arthrodesis of joints Free functioning muscle transfer | |
Abbreviations: ICN= intercostals nerve, MEP=motor-evoked potential, MT=middle trunk, NAP= nerve action potential, SSEP=somato-sensory-evoked potential, UT=upper trunk.
Complete (pan) brachial plexus injury
In patients with complete brachial plexus injury, useful recovery may still be obtained despite obvious limitations in the availability of functional donor nerves. If no proximal nerve is available, a common strategy consists of transferring the spinal accessory nerve to the suprascapular nerve (for shoulder stability), motor intercostal nerves to the musculocutaneous nerve or to the motor branch of the biceps (for elbow flexion), and sensory intercostals nerves to the lateral cord contribution of median nerve (for hand sensibility). When proximal nerves are available, a reconstructive strategy using multiple nerve transfers and nerve grafts may allow the possibility of regaining additional useful functions, including even rudimentary hand function. Additional donors have also been described, such as the phrenic nerve and contralateral C7 nerve. Our group stopped using the phrenic nerve, in view of our population of patients (often overweight and at risk to develop cardio-respiratory disease in their lifetime) and of the occurrence of respiratory function compromise in one patient. After review of our results from hemi-contralateral C7 nerve transfer for hand function, we now seldom choose this approach to regain hand function because of the poor functional grasp that was obtained.1 However, we currently often neurotize a free functioning gracilis muscle for elbow flexion in the acute stage to increase the chances of achieving adequate elbow flexion. If the triceps can be reinnervated (such as by nerve grafts from C7 or spinal accessory nerve), we consider using a free functioning muscle for both elbow flexion and finger flexion by prolonging the distal gracilis tendon to the flexor digitorum profundus and flexor pollicis longus tendons.
C5–C6 brachial plexus injury
When preganglionic injuries of the C5 and C6 nerves are present, several nerve transfer options exist to restore shoulder stability and elbow flexion. Potential donor nerves include the spinal accessory nerve, the triceps motor branches of the radial nerve,2,3 the medial pectoral nerves, the ulnar or median nerve,4–8 the intercostals nerves, the phrenic nerve, the ipsilateral9 and the contralateral C7 root. A common treatment approach includes the transfer of ulnar nerve fascicle(s) to the biceps motor branch of the musculocutaneous nerve to restore elbow flexion (Oberlin’s transfer), and a spinal accessory nerve transfer to the suprascapular nerve. The Oberlin’s transfer, with its good results, is now the procedure of choice for biceps reinnervation in preference to intercostal or spinal accessory nerve transfers.10 In our group, we attempt dual reinnervation when possible of both the shoulder (supraspinatus and deltoid) and elbow (biceps and brachialis muscles). The deltoid can be reinnervated using a triceps motor branch of the radial nerve to the axillary nerve and the brachialis muscle can be reinnervated with a fascicle from the median nerve.
C8–T1 brachial plexus injury
We treat lower trunk brachial plexus injuries by a combination of tendon transfers, selective arthrodesis of joints, and/or free functioning muscle transfer. The approaches to restore hand function are described in greater detail in Tu and Chung’s chapter on hand reconstruction. Tendon transfers, such as extensor carpi radialis longus to flexor digitorum profundus and brachioradialis to flexor pollicis longus, can be performed to restore finger flexion and pinch. Selective arthrodesis of the interphalangeal and carpometacarpal joint of the thumb can also improve both grasp and pinch. As the results of nerve repair are poor in lower trunk injuries because of the distance and time for reinnervation, we generally do not attempt nerve surgery in these patients. Others have suggested distal nerve transfers using the supinator motor branch to the posterior interosseous nerve, the brachialis branch of musculocutaneous nerve to the anterior interosseous median nerve fascicles, or the radial nerve branch to the extensor carpi radialis brevis muscle to the anterior interosseous nerve.11–15 At present, when good tendon transfer and arthrodesis options exist, we prefer these approaches.
Pre-procedural/therapeutic considerations
Not all patients are appropriate candidates for free functional (gracilis) muscle transfer (FFMT). A few particular pre-operative considerations are specific to this particular reconstructive approach and need to be discussed. First, a viable arterial and venous supply must be present. Second, an expendable motor nerve must be present near the transferred muscle’s neurovascular pedicle to reinnervate the transferred muscle. The third and fourth intercostal motor nerves and the spinal accessory nerves are usually good candidates. The patients considered for FFMT must understand the inherent risks, including flap loss, and the expected outcomes.16 They must be prepared to undergo a major operation with hospitalization and extensive rehabilitation and understand the goals of the surgery.
The upper extremity recipient bed for the transferred muscle must provide adequate skin coverage and ideally be free of adherent scar, to allow for muscle and tendon gliding. However, this may not always be possible in cases of brachial plexus injury. If the skin is significantly scarred, it may be difficult to cover the muscle transfer. Transferring a skin paddle with the muscle may help, but this is reliable only proximally for the gracilis myocutaneous flap17 and coverage of the distal end of the muscle and tendon may remain an issue. Using the muscle transfer for the “dual purpose” of providing elbow flexion and coverage of exposed structures or hardware is not recommended as it will lead to inevitable scarring and result in poor outcomes.
Another important consideration is the assessment of the vasculature to the injured upper extremity, especially when a FFMT is considered. In these patients, especially when the first rib has been fractured, the axillary and subclavian vessels may have sustained an injury.18,19 In the authors’ experience, a normal peripheral pulse does not preclude vascular injury, especially in the major branches. Therefore, we generally evaluate the vasculature using MR angiography (MRA). Special attention is given to the thoracoacromial trunk, our preferred source of arterial supply for the FFMT. Other options to formally evaluate the vasculature include CT angiography or conventional angiography. Any of these vascular studies will also assess post-traumatic stenosis and the patency of a previous vascular repair or reconstruction. In cases in which the thoracoacromial trunk is not intact, alternative options may be explored for the vascular anastomoses, including vein graft, arteriovenous loop preparation, and end-to-side anastomosis into the axillary artery.20
Procedural approach
Step-by-step description of all reconstructive options is beyond the scope of this chapter. However, we will briefly described the most commonly used approaches including brachial plexus exploration and neurolysis, nerve grafts, common nerve transfers (spinal accessory nerve, intercostal nerves, Oberlin procedure, and triceps branch to axillary nerve transfer), and the use of a free functioning muscle (gracilis muscle) transfer for elbow flexion. Other techniques to obtain hand function are described in Chapter 20.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree