CHAPTER 8 Radiographic assessment in pediatric brachial plexus palsies
Summary Box
Neurological aspects of neonatal brachial plexus palsy
Neonatal brachial plexus palsy (NBPP) may be due to traction of the nerves of the brachial plexus during the perinatal period.1 Radiographic imaging may be indicated urgently to assess for the presence of clavicular or humeral shaft fractures or diaphragmatic asymmetry in the case of a phrenic nerve lesion. Plexus-based neurological deficits in NBPP may mask symptoms due to coincidental, more peripheral, nerve lesions resulting from fractures of the long bones in the arm.2 Symptoms can even be caused solely by more distal peripheral nerve lesions. Uncommon differential diagnostic considerations are spinal cord tumors (Figure 8.1), hemangioma or other space-occupying lesions in the neck or brachial plexus, idiopathic plexitis, central lesions with hemiparesis, or arthrogryposis.3–6
Imaging studies for plexus lesions in NBPP are usually postponed and performed only when microsurgical nerve repair/reconstruction is indicated in babies with severe lesions. Inadequate recovery of motor function in an incomplete plexus injury at 3 months of age, or a total plexus lesion with no motor function, are indications to reconstruct the plexus and perform imaging as part of the preoperative work up.7–9 Preoperative ancillary investigations should provide information on type, location, and extent of nerve injury, and should support the clinical diagnosis and decision-making process.10 Ideally, imaging studies should depict the course of and supply information on the pathological anatomy of the cervical spinal roots, from their origin as dorsal and ventral rootlets at the spinal cord through the vertebral foramina, the extraforaminal spinal nerves, the trunks and divisions or cords of the brachial plexus down to the proximal parts of the main nerves of the arm. At present, functional imaging of central connections of the brachial plexus in babies remains unrealistic.
Of the 4 basic types of nerve injury,11 the 2 most severe types are managed by surgery: neurotmesis, a complete postganglionic disruption of a nerve with secondary neuroma formation, and avulsion, a preganglionic disconnection of a spinal nerve from the spinal cord. Early preoperative imaging is concentrated on these injury types, but more specifically on root avulsions. In NBPP, most lesions are at the level of the supraclavicular plexus structures, i.e., nerve roots, spinal nerves, and trunks. Combinations of different types of lesions within NBPP are common. The nerve surgeon who explores the injured brachial plexus in babies is sometimes puzzled by the pathological anatomy. Understanding the type or combination of different types of injury is crucial in deciding how best to reconstruct an injured plexus.
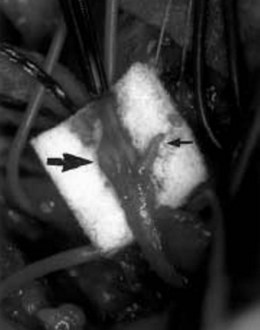
Nerve grafting and nerve transfer are the basic techniques used in micro-reconstructive nerve surgery. The success of nerve grafting procedures in NBPP depend on the presence of regenerating axons in proximal nerve stumps.1,11,12 When spinal roots are avulsed from the spinal cord, the spontaneous regenerative capacity of motor function is lost, as there is no connection with the central cell body of the motor nerve. During surgery, a root avulsion is evident when the dorsal root ganglion is retracted extraforaminally (Figure 8.2). If an avulsed nerve root is not extraforaminal, it sometimes appears pale and thin, but may look deceivingly normal at its exit from the foramen. Presuming the nerve to be normal and leaving it alone will, of course, be a wrong decision. Repair using such a nerve as a donor is doomed to be ineffective because it contains no regenerating axons. The same holds true for intradural and intraforaminal ruptures of spinal nerve roots that cannot be visualized during surgery.
Although of considerable academic interest, the presence of other types of lesions peripheral to the foramina actually is of less clinical importance because these can readily be recognized and analyzed at operative exploration of the brachial plexus.12
If, after reconstruction and nerve grafting or transfer, a child fails to recover, exact imaging of the extraforaminal plexus structures gains more importance. This would include cases of secondary neuromas of graft connections, focal lesions in proximal distributions of nerves, or other causes of failed surgical repair. Rarely, late neurological symptoms develop secondary to NBPP. The related pathology can be detected by appropriate imaging. These include arachnoid cysts compressing the spinal cord or herniation of the spinal cord into a large pseudomeningocele.13 Superficial siderosis of the central nervous system after root avulsions is a well-known occurrence in adult traumatic cases, but should also be considered in pediatric cases.14
Orthopedic aspects of neonatal brachial plexus palsy
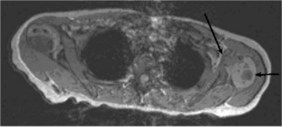
Some infants with NBPP have clavicular15 (Figure 8.3) or humeral shaft fractures. The primary neurological lesion may also lead to development of secondary deformities of the shoulder and arm; specifically, structural changes in bones and joints. Because NBPP predominantly involves the upper nerve roots or upper trunk, a muscular imbalance – paralysis of the abductors and external rotators, and a relative dominance of internal rotators – appears around the shoulder. Consequently, a characteristic secondary deformity develops; a flexion and internal rotation contracture of the shoulder with a posterior subluxation of the humeral head.1,16 This influences growth of the shoulder in the following manner: the cartilaginous part of the glenoid loses its flat form and becomes convex; retroversion of the glenoid increases; and the posterior labrum shifts posteriorly. This leads to development of a pathological biconcave glenoid fossa and a posteriorly subluxated humeral head, easily appreciated on MRI (Figure 8.4). At first these deformities are cartilaginous; however, with gradual ossification of the cartilage, bony deformities evolve. In the case of posterior subluxation of the humeral head, the coracoid process is directed caudally instead of anteriorly. The scapula is rotated externally and tilted anteriorly, and is smaller than the normal side. In some cases, humeral head retroversion is larger than normal because of the lack of normal remodelling.16 Another frequent deformity in children is a flexion contracture of the elbow, usually mild, and seldom combined with a radial head dislocation.17 Depending on the extent of paresis of the lower arm muscles, pronation and/or supination can be reduced, sometimes leading to contractures. In the more extensive types of NBPP, hand function is reduced and wrist and finger contractures can develop.
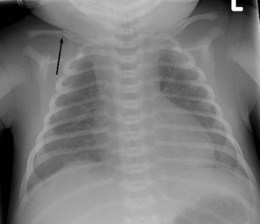
Figure 8.3 Plain radiograph of clavicle fracture associated with NBPP. Arrow indicates broken clavicle.
Radiographic imaging is used in the first days postpartum to exclude fractures in the shoulder region, other rare causes of symptoms, and the presence of a diaphragmatic asymmetry caused by phrenic nerve paresis (Figure 8.5). Computed tomography (CT)-myelogram or magnetic resonance imaging (MRI) is not indicated for acute injury. Around the third month, imaging (CT-myelogram or MRI) is indicated mainly to exclude root avulsions in babies who do not show sufficient neurological recovery (Table 8.1).
Table 8.1 Indications for radiographic imaging in neonatal brachial plexus palsy
| Patient age | Imaging | Indication |
|---|---|---|
| First week of life | Radiograph | Fractures, luxations, paresis diaphragm |
| Ultrasonography | Paresis diaphragm, entrapment of radial nerve in humeral shaft fracture | |
| 3–4 months | MRI | Diagnose preganglionic root lesions, differential diagnosis of early shoulder deformity |
| CT-myelography | Diagnose preganglionic root lesions | |
| Ultrasonography | Shoulder position and dynamics | |
| >1 year | MRI, radiograph, or selective other imaging | Secondary deformities |
| Ultrasonography | Shoulder position and dynamics | |
| Puberty | Radiographs | Subluxation, deformity |
| CT | Secondary deformities of shoulder |
CT = computed tomography; MRI = magnetic resonance imaging
Plain radiographs
Neurological/neurosurgical aspects
A chest X-ray should be the standard procedure to assess for diaphragmatic paralysis consequent to a phrenic nerve lesion. In babies with indications for nerve surgery, plication of a paralytic diaphragm, preferably by an endoscopic procedure, may be necessary. A post-plication chest radiograph is recommended before exploring the brachial plexus. A chest X-ray is especially important when intercostal nerve transfers are considered, so as not to compromise breathing and sucking activity further.18 The same holds true to check functional integrity of the diaphragm when the phrenic nerve is being considered as a possible donor in a nerve transfer in babies with suspected multiple root avulsions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree