Fig. 1
(a, b) Appearance of radial longitudinal deficiency. (a) A 6-month-old boy with bilateral radial longitudinal deficiency. Note associated absence of thumbs, significant radial deviation of wrist, shortened forearm, and limited elbow flexion. (b) Late radiographic appearance of a forearm and wrist in an 18-year-old boy with untreated Holt-Oram syndrome. Note significant radial deviation of the wrist, absence of thumb and index finger, and the lunate is articulating with the metaphysis of the ulna
In conjunction with the osseous abnormalities, there are corresponding abnormalities within the soft tissues. In the most general terms, the muscles that arise from the medial epicondyle are present but abnormal and can be fused distally, while the muscles that arise from the lateral epicondyle are often absent, accounting for the poor wrist extension seen in most cases (Bayne and Klug 1987). Muscles most commonly absent include the anconeus, supinator, extensor carpi radialis brevis, and pronator quadratus. The flexor carpi radialis is often absent, and if present, it is hypoplastic with an abnormal insertion. The extensor carpi radialis longus if present is often nonfunctional (Bora et al. 1981) (Flatt 1994).
Abnormal insertions of the residual radial wrist flexors directly into the carpus have been observed. Specifically, in patients with thrombocytopenia-absent radius (TAR) syndrome, a “brachiocarpalis” muscle has been noted originating on the anterolateral aspect of the proximal humerus and inserting into the radial side of the carpus (Oishi et al. 2009). This muscle has been postulated to be a cause of ongoing radial wrist deviation as well as persistent elbow flexion. It can be divided surgically in an effort to improve hand and elbow position (Fig. 2). In many cases of RLD, the flexor superficialis muscle may also be abnormal or fused to the surrounding carpus or metacarpals (which may complicate future opponensplasty procedures). Ulnar structures such as flexor carpi ulnaris muscle, extensor carpi ulnaris muscle, and hypothenar muscles are preserved. The thumb thenar muscles are hypoplastic or absent, and their presence is dependent on the amount of osseous hypoplasia seen within the thumb (Bayne and Klug 1987; Flatt 1994).
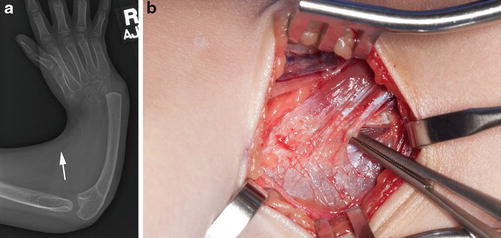
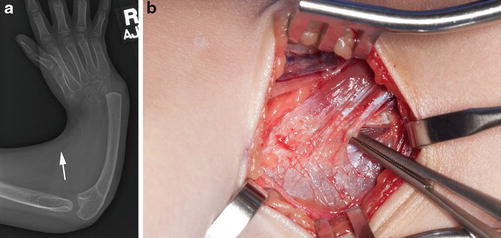
Fig. 2
(a, b) (a) AP radiograph of the forearm in a 4-year-old girl with TAR syndrome. The arrow points to a soft tissue density which represents the brachiocarpus muscle which begins at the humerus and inserts at the radial aspect of the carpus. (b) Intraoperative photograph showing the appearance of muscle with broad insertion into carpal capsule
With regard to neurovascular structures, the musculocutaneous nerve is usually absent or aberrant with its normally innervated muscles supplied by branches of the median nerve (Flatt 1994). The radial nerve frequently terminates at the elbow. Within the forearm, due to the absence of radial structures, the median nerve can lie radial and more dorsal than expected (Fig. 3). It may often supply residual radial structures that would have normally been supplied by the radial nerve. It also gives off a dorsal sensory branch replacing the terminal sensory branch of the radial nerve. The ulnar nerve is usually normal. The radial artery is frequently absent or hypoplastic being replaced occasionally by a persistent median artery while the ulnar artery is normal (Huffstadt and Broker 1978; Inoue and Miura 1991; Manske and McCarroll 1998).
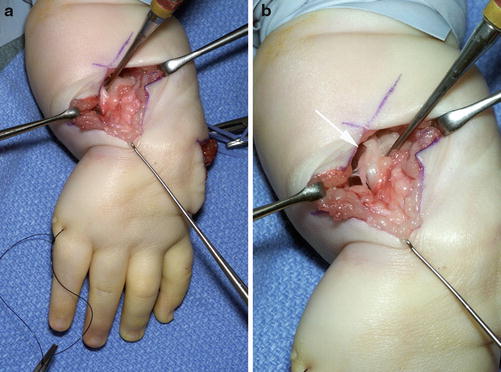
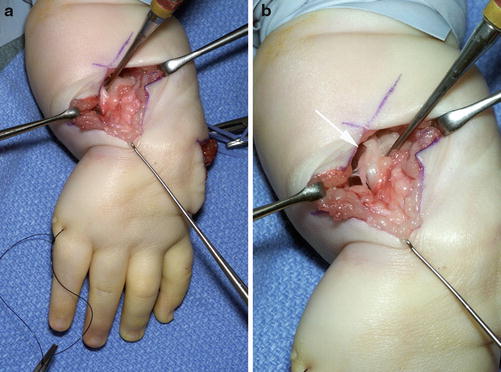
Fig. 3
(a) Intraoperative photograph showing the dorsal approach to the carpus in a 12-month-old during a centralization procedure. (b) The median nerve is noted to be radial (arrow) contributing to the radial sensation within the hand
Such anatomical abnormalities lead to a forearm which is short and j shaped. Some component of wrist radial deviation will be passively correctable, but in severe forms the wrist may be radially deviated beyond 90° and quite stiff. The elbow is usually held in an extended position and the child’s manipulation of objects is usually performed with the more mobile ulnar digits (Fig. 4). In milder forms of RLD where the thumb is present (but hypoplastic), more “normal” oppositional pinch and grasp may be possible, but cross pinch between the fingers tends to be the norm. The one exception is seen in children with TAR syndrome; in these cases, the thumb is always present and allows for some improvement in pinch and grasp (Hedberg and Lipton 1988). Sensation is normal within the hand. Finger motion is often restricted within in the radial digits and the joint shape in the radial phalanges is abnormal, often leading to flexion deformities at the PIP joint in older children or stiff straight digits in children presenting at earlier ages (Flatt 1994). Power grip is often compromised by the instability present at the wrist.


Fig. 4
Manipulation of smaller objects is usually performed with ulnar digits as shown in this 3-year-old girl with untreated RLD and significant radial deviation of the wrist
Incidence and Etiology
The incidence of RLD in literature is estimated between 1:30,000 and 1:100,000 live births (Bod et al. 1983; Kallen et al. 1984; Wynne-Davies and Lamb 1985; Bayne and Klug 1987; Urban and Osterman 1990). Although these statistics show radial deficiency to be rare, it is the most common of the major longitudinal deficiencies (which includes ulnar dysplasia and central deficiency). The frequency of unilateral and bilateral cases of RLD is similar (Lamb 1977; Lourie and Lins 1998; Geck et al. 1999). In unilateral cases, the right side is affected more often than the left side. There is no difference in incidence between the sexes for unilateral cases; however, bilateral cases occur more frequently in male patients at a ratio of 3:2 (Lamb 1977; Bod et al. 1983; Kallen et al. 1984; Wynne-Davies and Lamb 1985; Urban and Osterman 1990; Evans et al. 1994; Upton 2006).
The etiology of radial longitudinal deficiency remains largely unknown. The varied phenotypic spectrum of the disorder suggests both an environmental as well as genetic component (de Graaff and Kozin 2009). It is presumed that RLD is the result of an early disruption in the sequence of normal limb development as the upper limb develops from the migration of ectodermal and mesodermal tissue between the fourth and seventh postconception weeks. It is assumed that genetic, environmental, or idiopathic factors can all cause specific developmental defects during this period (Lamb 1977; Urban and Osterman 1990).
The formation of the embryonic limb bud is the first step toward normal development of the upper extremity (Daluiski et al. 2001). The apical ectodermal ridge (AER) represents a layer of surface ectodermal cells at the distal end of the embryonic limb bud that is responsible for cell signaling and limb differentiation. In experiments by Saunders, partial resecting of the AER in dogs resulted in failure of radial bone development (Saunders 1948). Changes in the distribution of fibroblast growth factors from the AER and the underlying mesoderm can impair the development of longitudinal skeletal formation along the limb’s proximal-distal axis. Niswander and Martin have shown in both mouse and chicken embryo models that fibroblast growth factor four (FGF-4) is capable of producing proliferation of mesenchymal cells within the developing limb bud AER. AER-deficient limb buds treated with FGF-4 were capable of developing normal patterns of limb outgrowth. Niswander and Martin also showed that bone morphogenic protein two (BMP-2) was capable of inhibiting this growth (Niswander and Martin 1993a, b; Niswander et al. 1993; Daluiski et al. 2001). Studies such as these help to elucidate the role fibroblast growth factors play in the etiology of RLD.
Known factors harmful to the cells within the AER include X-rays, thalidomide, oral anticoagulants, Coumadin derivatives, and anticonvulsants (Elbaum et al. 1995). Ogino and Kato have shown that WKAH/Hkm rats exposed to busulfan at weeks 10 through 11 of development develop limb deformities that are similar to longitudinal deficiencies seen in humans (Kato et al. 1990; Ogino 2004). In Ogino’s studies, limb changes were global suggesting that injuries to mesenchymal cells within the AER may have widespread implications for limb development.
Associated Anomalies and Syndromes
RLD is rarely an isolated finding and is associated with several congenital syndromes (Tables 1 and 2) (Goldfarb et al. 2006a; de Graaff and Kozin 2009). Isolated radial deficiency is estimated to comprise only 8–30 % of the cases (Goldfarb et al. 2006b; Koskimies et al. 2011). The frequency of associated anomalies increases with the severity of RLD (Goldfarb et al. 2006a). Associated anomalies are seen in 40 % of patients with unilateral involvement and 77 % of patients with bilateral involvement (Lin and Perloff 1985; Goldfarb et al. 2006a; Koskimies et al. 2011); (Goldberg and Bartoshesky 1985). Because greater than 70 % of the cases are associated with some other anomalies, signs of RLD should lead the practitioner to search for problems in other organ systems.
Table 1
Syndromes associated with RLD with known Mendelian inheritance pattern (From de Graaff 2009)
Syndrome | Inheritance pattern |
|---|---|
Thrombocytopenia-absent radius syndrome | Autosomal recessive |
Vertebral anomalies, anal atresia, cardiac abnormalities, tracheoesophageal fistula, renal anomalies, and limb anomalies (VACTERL) | Autosomal recessive/complex |
VACTERL association with hydrocephalus | X-linked |
Holt-Oram syndrome | Autosomal dominant |
Fanconi’s anemia | Autosomal recessive/X-linked |
Duane-radial ray syndrome | Autosomal dominant |
Baller-Gerold syndrome | Autosomal recessive |
Townes-Brocks syndrome | Autosomal dominant |
Rothmund-Thomson syndrome | Autosomal recessive |
Skeletal | Cervical rib-radial ray (Funston syndrome) |
Costovertebral dysplasia (Keutel syndrome) | |
Klippel-Feil syndrome | |
Cardiac | Anemia-triphalangeal thumb (Aase-Smith syndrome) |
Cornelia de Lange syndrome | |
Cutaneous | Cutaneous poikiloderma (Rothmund-Thomson syndrome) |
Renal | Renal-radial ray aplasia (Sofer syndrome) |
Craniofacial | Acrofacial dysostosis (Nager syndrome) |
Acro-reno-ocular syndrome | |
Craniofacial microsomia | |
Eye-radial syndrome | |
Lacrimal auriculo-dento-digital syndrome (LADD or Levy-Hollister syndrome) | |
Radial ray-choanal atresia | |
Micrognathia and limb anomalies (Hanhart syndrome) | |
Mandibulofacial dysostosis (Treacher Collins syndrome) | |
Oculo-auriculo-vertebral dysplasia (Goldenhar syndrome) | |
Oro-cranio-digital syndrome (Juberg-Hayward syndrome) | |
Roberts syndrome |
The most common syndromes associated with RLD include the VACTERL association, Holt-Oram syndrome, Fanconi’s anemia, and thrombocytopenia-absent radius (TAR) syndrome (Riordan 1955; Heikel 1959; Fanconi 1967; Skerik and Flatt 1969; Lamb 1977, 1991; Manske et al. 1981; Wynne-Davies and Lamb 1985; Bayne and Klug 1987; Urban and Osterman 1990; Botto et al. 1997; James et al. 1999, 2004; Maschke et al. 2007). These syndromes will be discussed in more detail, while a list of other associated anomalies is provided in Tables 1 and 2.
VACTERL Association
VACTERL is an acronym for vertebral anomalies (V), anal atresia (A), cardiac anomalies (C), tracheoesophageal fistula (TE), renal anomalies (R), and limb abnormalities (L). Three of these malformations need to be present to meet the criteria for the VACTERL association. The most common occurring anomalies are cardiovascular defects and renal agenesis; RLD is the most common occurring limb defect in the VACTERL association, but other hand anomalies can include thumb hypoplasia and polydactyly (Quan and Smith 1973). The cardiovascular anomalies most frequently encountered in these children are atrial septal defects (ASD) and ventricular septal defects (VSD) (Buck-Gramcko 1985; Wynne-Davies and Lamb 1985). A multidisciplinary approach needs to be taken with these children to determine the appropriate time for limb surgery.
Holt-Oram Syndrome
Holt-Oram syndrome is an autosomal-dominant disorder of variable penetrance. It is characterized by RLD and associated cardiovascular malformations, most commonly atrial or ventricular septal defect. Other associated hand anomalies can include radioulnar synostosis, triphalangeal thumb, and humeral defects. Occasionally, spinal malformations may be present. The incidence of Holt-Oram syndrome is estimated at 1 in 200,000 live births (Holt and Oram 1960; Goldberg and Bartoshesky 1985; Elbaum et al. 1995; Bossert et al. 2002).
Fanconi’s Anemia
Fanconi’s anemia is an autosomal-recessive pancytopenia associated with RLD and is characterized by major organ deformities and early-onset bone marrow failure. The disorder is associated with multiple mutations in the transcription factor TBX5, a gene located on chromosome 12q24.1 (Li et al. 1997). Clinical features include growth retardation, major organ abnormalities, hypo- or hyperpigmentation of the skin (café-au-lait spots), typical facial appearance (small head, eyes, and mouth), and a predisposition to develop certain forms of cancers. The risk of squamous cell cancer of the mucous membranes, liver cancer, and acute myeloid leukemia is increased several fold in these individuals. 90 % of children will develop acute bone marrow failure within the first decade of life (Wilks et al. 2012). The pancytopenia can be treated with bone marrow transplantation, but even with these efforts, life expectancy is only estimated at 30 years (range 0–50) (Wilks et al. 2012).
Early detection is critical so that bone marrow transplant can be performed before the patient has had to receive multiple blood transfusions, which can complicate future bone marrow transplantation. Bone marrow transplantations performed before the age of 10 in these children have shown improved outcomes (Wilks et al. 2012). While early detection provides the best chance of long-term survival, signs of anemia are not noticeable on standard blood tests at birth due to the late onset of the anemia. To detect this condition in infancy, a diepoxybutane (DEB) fragility testing chromosomal challenge can be conducted (Esmer et al. 2004). If the test is abnormal, close hematologic monitoring is recommended to identify early signs of bone marrow failure as the child ages (Auerbach et al. 1985; Goldfarb et al. 2006b). In addition, a search for a bone marrow match can be performed prior to the onset of pancytopenia.
Fanconi’s anemia is most commonly associated with preaxial skeletal deformities and has been reported to occur in 3.5 % of cases of RLD but may also be seen in 7 % of patients with other congenital thumb anomalies. One case has been documented in a child with unilateral thumb duplication. Present recommendations include DEB fragility testing in children with RLD, especially when associated with abnormal facies or abnormal skin pigmentation (Esmer et al. 2004; Upton 2006; de Graaff and Kozin 2009; Webb et al. 2011; Wilks et al. 2012).
TAR Syndrome
Thrombocytopenia-absent radius (TAR) syndrome is characterized by a hypomegakaryocytic thrombocytopenia in association with RLD (de Graaff and Kozin 2009; Fig. 5). A microdeletion in 1q21.1 has been found to be associated with the development of this disorder (Klopocki et al. 2007). The incidence is estimated at 1 per 239,000 to 1 per 500,000 live births (Hall 1987; Goldfarb et al. 2006b). Clinical manifestations include bruising, severe hemorrhaging, and, in 30 % of the cases, cardiac and/or renal abnormalities (Urban and Osterman 1990). Other associated malformations include varus knee deformities, knee flexion deformities, and internal tibial rotation (D’Arcangelo et al. 2000). Only 50 % of children will show signs of thrombocytopenia at birth, but 90 % will show abnormalities by 4 months of age (Hall et al. 1969). The only surgery which is medically justified before the child experiences a stabilization of the platelet count is cardiac surgery. Hematologic treatment of severe thrombocytopenia consists of platelet transfusions. Platelet counts can be negatively affected by viral illnesses, minor trauma as well as any surgery.


Fig. 5
Photograph of a 3-year-old female with TAR syndrome. Note appearance and position of thumb
A particular phenotypic characteristic for TAR syndrome is the presence of the thumb despite radial deficiency (Hedberg and Lipton 1988). Although present, the thumb usually lacks normal function due to stiffness of the thumb and other digits (Fig. 5). Most thumbs lack interphalangeal joint (IP) motion and tend to have an extension deficit at the metacarpal-phalangeal (MP) joint, resulting in impaired hand grasp of large objects (Goldfarb et al. 2007).
The frequent association of RLD with the aforementioned syndromes emphasizes the importance of a thorough and complete physical exam. This should include an assessment of facial features and lower limbs and cardiac and spinal examination (Goldfarb et al. 2006b). Further testing should include spinal radiographs, an echocardiogram, a complete blood count with peripheral blood smear, and a renal ultrasound exam (Elbaum et al. 1995; Goldfarb et al. 2006b; Maschke et al. 2007; Manske and Goldfarb 2009). Additionally, close collaboration with a specialized pediatrician is necessary to provide an appropriate long-term treatment plan. Due to the high incidence of associated anomalies, many patients with RLD need specialized cardiac monitoring while undergoing general anesthesia. Surgical procedures should be conducted in a specialized pediatric center capable of monitoring these children during the perioperative and postoperative period (Quan and Smith 1973).
Assessment of Radial Longitudinal Deficiency
Signs and Symptoms and Baseline Hand Function
Radial longitudinal deficiency (RLD) is characterized by a radial-deviated wrist and the affected hand held in flexed position. The deformity is always present at birth but continues to develop with growth of the limb. If untreated, wrist position tends to deteriorate with further radial deviation occurring with growth. Stiffness develops with increasing palmar subluxation of the carpus and ulnar bowing during infancy (Lamb 1977). Associated hand anomalies include thumb hypoplasia and stiffness of the radial digits (index and long most commonly). Forearm length is usually only 60 % of the unaffected side (Bayne and Klug 1987; Sestero et al. 2006). The extent of hand disability depends on the severity of the dysplasia. In severe cases, joint dysfunction can extend proximal to the elbow and shoulder (Urban and Osterman 1990).
Diagnostic Imaging
The defining characteristic of RLD is hypoplasia of the radius. The standard radiographic assessment in RLD patients consists of bilateral anteroposterior and lateral radiographs of the arm, forearm, wrist, and hand. The wrist is preferably positioned as straight as possible without stress for imaging (Manske et al. 1981; Ekblom et al. 2013).
Several radiographic parameters have been established to study wrist position preoperatively and postoperatively (Manske et al. 1981). The hand-forearm angle (HFA) is used to quantify the angulation between the hand and forearm. The HFA can be measured using a standard anteroposterior (AP) radiograph and is defined as the angle between the longitudinal axis of the long finger and the longitudinal axis of the distal ulna (Manske et al. 1981). In many cases, the ulna will be bowed toward the hypoplastic or absent radius. This will provide a false appearance of the actual HFA. To standardize the longitudinal axis of the distal ulna, a line is drawn across the distal epiphyseal plate of the ulna. From the middle of the epiphyseal plate, a perpendicular line can be drawn, which is defined as the longitudinal axis of the ulna. The direct angle between this constructed line and the longitudinal axis of the long finger measures the HFA (Fig. 6). The hand-forearm position (HFP) is determined as the shortest distance between a line drawn through the longitudinal axis of the distal ulna and the proximal pole of the fifth metacarpal. The HFP can be determined from a standard AP radiograph. The base of the fifth metacarpal can be deviated radial or ulnar to the ulnar shaft; therefore, radial and ulnar displacement is measured as plus or minus to this point (Fig. 6). The ulnar bow can be measured by using the aforementioned method for determining the longitudinal axis of the distal ulna. The longitudinal axis of the proximal ulna can be constructed in a similar way, and the intersection of these two lines measures the ulnar bow in degrees. Ulnar bow is measured on a standard AP radiograph.


Fig. 6
The hand-forearm angle can be measured radiographically from the angle created between a line placed axial through the third metacarpal and capitate and a line placed perpendicular to the ulnar articular surface (also known as the distal ulna midline). Distance (A) represents the hand forearm position which measures the distance from the base of the fifth metacarpal to the distal ulna midline. The ulna bow is measured by the angle created by the distal ulna midline and a line drawn through proximal midline of the ulna
Classification
In 1976, the International Federation of Societies for Surgery of the Hand classified RLD within Category I, which describes a failure of formation of parts (Swanson 1976). In 1987, Bayne and Klug expanded upon this classification breaking RLD into four categories based on the radiologic characteristics of the radius; this classification has been modified several times since its introduction (Bayne and Klug 1987). Their description of the four types of RLD is based on the severity of the osseous deficit (Fig. 7). Type I is defined as a minimally shortened radius of more than 2 mm with respect to the ulna (James et al. 1999). There is no ulnar bowing and elbow function is normal. Thumb hypoplasia is almost always present and the radial carpal bones are usually hypoplastic. Surgical management of the wrist in these cases is rare, and if necessary, surgery is usually directed toward improving any abnormalities in thumb function (Maschke et al. 2007).
Fig. 7
The original Bayne classification system for RLD (Copyright Mayo Foundation)
In type II , both proximal and distal epiphyses are affected resulting in a hypoplastic radius. This type of deficiency is commonly referred to as “radius in miniature” (Bayne and Klug 1987). The ulna is usually thickened and bowed toward the radius. The hand and wrist are subsequently positioned more radially. Thumb hypoplasia and an absent scaphoid are common in type II (Lamb 1977). To limit the amount of radial deviation and to facilitate better surgical results, patients should be splinted and stretched at an early age. Surgery in these cases consists of procedures to correct radial bowing of the ulna and to stabilize the wrist. Surgical options are described in detail further in this chapter.
Type III consists of partial absence of the radius. This deficit can be located in the proximal, middle, or distal third of the radius, but type III usually presents with a proximal radial remnant (Manske and McCarroll 1998). Some proximal remnants may not be visible until older age (Upton 2006). Thumb hypoplasia or aplasia is often present, and absence of the scaphoid and trapezium is frequently seen in this subgroup. Patients often have tight soft tissue (the anlage) extending from the remaining radial remnant to the carpus. This results in the wrist moving into flexion and pronation.
Type IV is characterized by complete absence of the radius. The hand is severely displaced to the radial side, and in older patients, the carpal bones may articulate with the radial border of the distal ulna. Ulnar bowing is present and normal growth and development of the ulna is inhibited. Overall ulnar growth is limited and the forearm rarely grows to more than 60 % of the contralateral side (Heikel 1959). Limited elbow motion is often seen. This type of deformity is always seen in conjunction with thumb aplasia and limited motion of the radial digits. The one exception to this is the patient with TAR syndrome where the thumb is always present but has limited function (Hedberg and Lipton 1988).
This Bayne classification was expanded by James and colleagues (James et al. 1999) to include patients with hypoplasia of the thumb without significant deficiency in the radius (classified as type N) and patients with abnormalities in the radial carpal bones classified as type 0 (Fig. 8). In cases of type 0, the radial carpal bones are absent or hypoplastic, but there is no shortening of the distal radius; however, abnormalities may exist in the proximal radius such as congenital dislocation of the radial head or radioulnar synostosis (Maschke et al. 2007). Further modifications were made by Goldfarb and colleagues to address abnormalities in the humerus. They use the classification of type V RLD for deficits of the proximal humerus, abnormalities of the glenoid, and distal humerus articulation with the ulna (Goldfarb et al. 2005). Despite these additions, types III and IV are thought to be the most common types of RLD (Upton 2006).


Fig. 8
AP radiographs in a child with bilateral thumb hypoplasia and evidence of an absent scaphoid on the left or type N deficiency
Treatment
There are three treatment options for RLD: (1) no treatment, (2) stretching and splinting alone, and (3) surgical correction in conjunction with postoperative stretching and splinting. The ultimate goal of any treatment is to improve hand function (i.e., grip strength and precision pinch), improve functional length, and improve appearance. An important aspect of any discussion regarding treatment should focus on providing the parents with realistic expectations for immediate and late posttreatment outcomes and the time required for each intervention.
Surgical treatment of RLD has changed tremendously over the past 30 years but is still focused on wrist stabilization and realignment during infancy and on lengthening the forearm during adolescence (Taghinia et al. 2007). Starting at birth, initial close contact with the coordinating pediatrician can expedite the initiation of treatment. Timing of any surgical intervention must be postponed until all hematologic and cardiac problems are stabilized. The multidisciplinary needs of these young patients make treatment in a single pediatric surgical center desirable for patients and their parents.
No Treatment
No treatment is most appropriate in cases where patients have substantial associated anomalies which may result in severe cognitive delays or life-threatening illness. Bayne and others have also suggested that treatment may be contraindicated in cases of mild disease, adult patients who have adapted to their hand and wrist deformities, and in patients who have limited elbow function with the inability to flex beyond 90°. In such patients, straightening the wrist may limit toileting and the ability to get the hand to the mouth (Flatt 1994) (Bayne 1991; D’Arcangelo et al. 2000).
Stretching and Splinting
The two methods of nonsurgical treatment are splinting and stretching of the tight radial soft tissues (Fig. 9). These treatment modalities are most appropriate for types I and II deformities. Therapy can start early after birth. Careful stretching by the parents or caregivers is thought to limit the radial contraction deformity and may create a more central hand-forearm position (HFP). Stretching of the wrist involves progressive longitudinal distraction, ulnar deviation, and extension while stabilizing the ulnocarpal joint (Maschke et al. 2007). The wrist is to be stretched as close to neutral as possible using gentle but firm passive traction. Due to the lack of consensus on the optimal rate for stretching, the most convenient interval is to combine stretching with an everyday activity such as diaper changes (Goldberg 1976; Flatt 1994; Maschke et al. 2007).
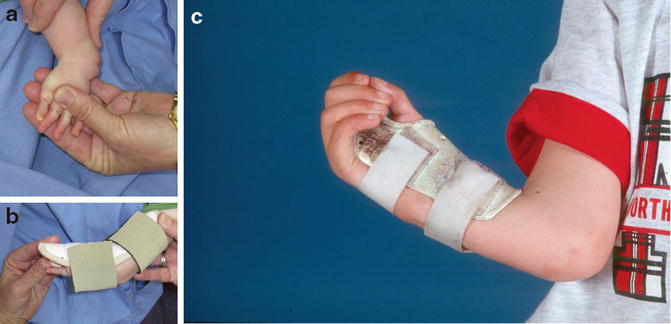
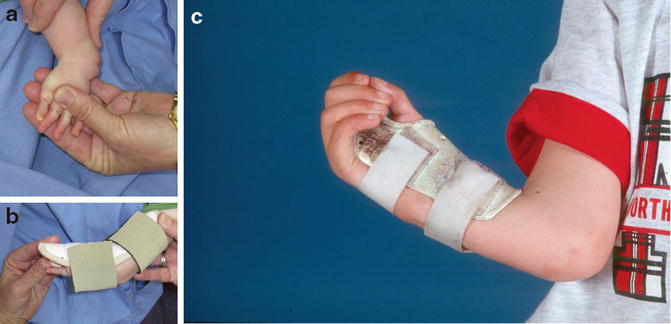
Fig. 9
(a–c) Stretching and splinting techniques are very helpful in preparing the wrist prior to centralization and radialization procedures and to maintain surgical correction after surgery. (a) Stretching techniques should be taught to parents and be performed three to four times a day. (b) Wrist splints may be applied to push the wrist into a more neutral position. (c) Splints may be worn after centralization procedures, as in this child with TAR, to prevent radial recurrence of wrist position
Serial splinting or casting is the other major technique for nonsurgical treatment. A radial gutter splint, which leaves the ulnar digits free, can be used to preserve the correction achieved with stretching. It is initially recommended to wear the splint during day and night, only taking the splint off during dynamic stretching. Once passive motion of the carpus is achieved, the splint regimen can be changed to usage of a splint during the night or periods of rapid growth (D’Arcangelo et al. 2000; Maschke et al. 2007).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


