7 Pulsed Doppler and Color Duplex Sonography in the Assessment of Tubal Patency Since Fitzgerald and Drumm introduced the Doppler principle into obstetric and gynecological diagnosis in 19776, the applications of this ultrasound technique have spread from obstetric medicine to the fields of gynecology and reproductive medicine3,7,15. The hemodynamics of the vessels of the lesser pelvis and especially of the internal genital organs are investigated by continuous-wave (CW) Doppler, pulsed-wave (PW) Doppler, and color-flow mapping (CFM). These techniques can be used, for example, to study the dependence of blood flow changes on the ovarian cycle or the hemodynamic effects of pregnancy or neoplasia. Tubal patency. To date, only a few reports have been published on the assessment of tubal patency with spectral Doppler ultrasound3a. Fallopian tube disease is one of the most frequent causes of infertility, accounting for approximately 25% of cases. The detection of tubal patency, then, is an important element in the evaluation of infertility. Conventional methods of testing such as pertubation, radiographic hysterosalpingography, and laparoscopic chromopertubation have drawbacks that include lack of precision, radiation exposure, and invasiveness. One alternative is the sonographic assessment of tubal patency9. The first such experience at our center was gained with the transvaginal scanning of the passage of saline solution through the oviducts. When a suitable ultrasound contrast medium became available (Echovist, Schering), we were able to improve the quality of B-mode visualization10. Subsequent studies were done to determine whether the use of pulsed Doppler and transvaginal color duplex scanning could furnish additional information in the noninvasive evaluation of tubal patency9a. Clinical population. Since the advent of ultrasound tubal imaging, 210 women have been examined with B-mode and Doppler ultrasound at our infertility clinic. The average patient age was 33 years. Two-thirds of the patients had primary infertility, and one-third had secondary infertility (Table 7.1). Only 20% of the patients had been previously evaluated for a tubal factor, but nearly all of the women had received prior infertility treatment. Timing of the examination. The examination was performed in an initial series before a planned laparoscopy in patients with stimulated cycles. The patients were eventually assigned to a gamete intrafallopian transfer (GIFT) program or an in-vitro fertilization (IVF) program based on tubal imaging results and laparoscopic findings. Written informed consent was obtained. The ultrasound assessment of tubal patency was performed in the late follicular phase, as this offers the best conditions for passing an intrauterine catheter atraumatically through the canal of the estrogen-primed cervix. Preparations for the examination. Prior to the outpatient procedure, acute genital infection was excluded by the determination of erythrocyte sedimentation rate (ESR), hemoglobin, and white blood cell count and by gynecological examination with a speculum and bimanual palpation. The ultrasound study was performed in a gynecological chair with no premedication or general anesthesia. After careful aseptic preparation of the vagina, a pediatric Foley catheter 2.7 mm in diameter (see Chapter 8) was passed through the cervical canal into the uterine cavity using sterile technique, and the catheter cuff was inflated with 2 ml of saline solution. In a few cases (e.g., patients with a previously operated cervix), it was necessary to grasp the cervix with a tenaculum or dilate the cervical canal. Next the endovaginal probe was introduced.
Applications of Doppler Sonography in Reproductive Medicine
Assessment of Tubal Patency
Patients and Method
| Characteristics of the patients examined | |
|---|---|
| Number (n) | 210 |
| Age (years) | 32.5 (25–41) |
| History of infertility (years) | 3.4 (2–10) |
| Primary infertility (%) | 65 |
| Secondary infertility (%) | 35 |
| Duration of study (months) | 60 |
Ultrasound equipment. The following ultrasound systems were used in the examinations:
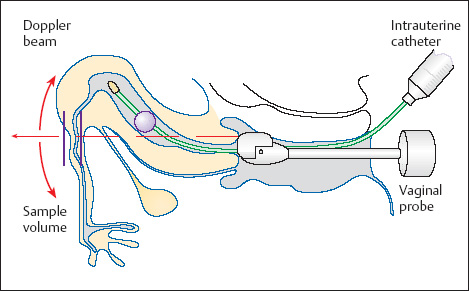
 Mechanical rotary scanner with a forward scan direction and 240° wide-angle view, a B-mode frequency of 5 and 7.5 MHz, a pulsed Doppler frequency of 4.5 MHz, and a pulse repetition frequency (PRF) of 3.9–15.6 kHz (Kretztechnik Combison 320–5 and 410, Zipf, Austria). The active Doppler beam could be freely steered over the entire B-mode area (240°), and the Doppler sample volume (1–15 mm) could be positioned at any depth over the 17 cm range of the scanner (Fig. 7.1).
Mechanical rotary scanner with a forward scan direction and 240° wide-angle view, a B-mode frequency of 5 and 7.5 MHz, a pulsed Doppler frequency of 4.5 MHz, and a pulse repetition frequency (PRF) of 3.9–15.6 kHz (Kretztechnik Combison 320–5 and 410, Zipf, Austria). The active Doppler beam could be freely steered over the entire B-mode area (240°), and the Doppler sample volume (1–15 mm) could be positioned at any depth over the 17 cm range of the scanner (Fig. 7.1).
 Electronic curved linear array with a forward-directed 150° beam, a B-mode frequency of 5–9 MHz, a pulsed Doppler frequency of 5 MHz, color duplex Doppler, and a penetration depth of 8–10 cm (Ultramark 9 HDI ESP, ATL, Bothell, WA, USA).
Electronic curved linear array with a forward-directed 150° beam, a B-mode frequency of 5–9 MHz, a pulsed Doppler frequency of 5 MHz, color duplex Doppler, and a penetration depth of 8–10 cm (Ultramark 9 HDI ESP, ATL, Bothell, WA, USA).
Fig. 7.1 Instrumentation used for tubal imaging with Doppler ultrasound. The catheter for contrast instillation is inside the uterus, and the endovaginal probe is in the posterior fornix. The Doppler sample volume has been positioned over the intramural and near-proximal tubal segment.
Contrast medium. The contrast medium consisted of a freshly prepared suspension of galactose microparticles (Echovist R, Schering, Berlin). Microbubbles adsorbed to the surface of the particles provide enhanced reflection of the ultrasound waves and increased sonodensity.
Examination Technique
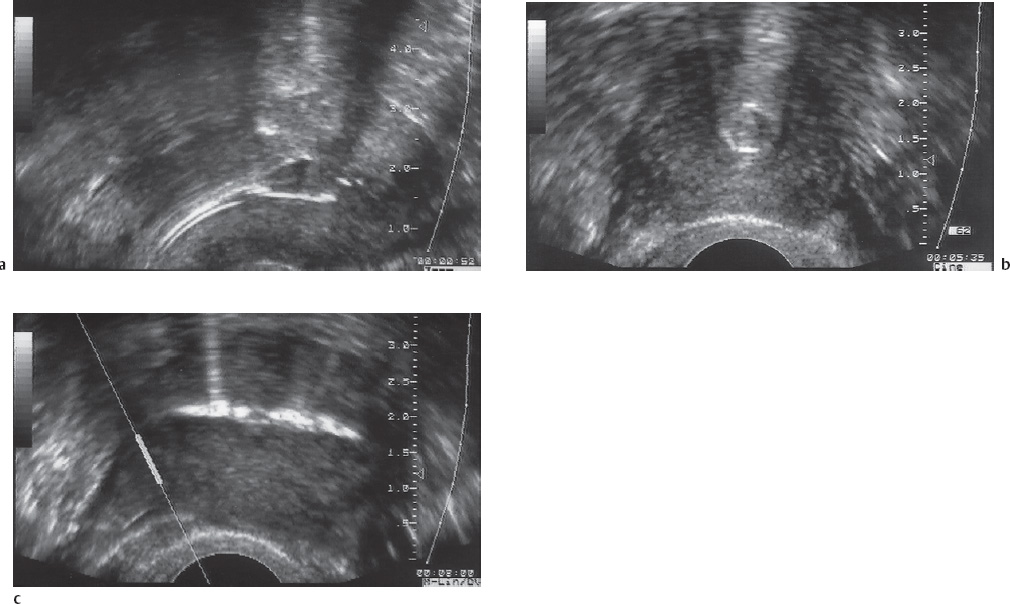
The uterine fundus is imaged in a B-mode reference plane in which the echogenic catheter tip and inflated cuff can be identified, and then a small contrast bolus is injected (Fig. 7.2).
B-mode analysis. Contrast enhancement can be seen in the uterine cavity, across the uterotubal junction, in the intramural part of the tube, and even in distal tubal segments in some cases. The flow of contrast medium can be tracked in the real-time image. The contrast agent is administered in small, pulsatile injections for optimum B-mode visualization of the flow dynamics.
Fig. 7.2 Appearance of the inflated catheter cuff within the uterus.
a Longitudinal scan.
b Transverse scan.
c Initial contrast appearance in the uterine fundus. The sample volume is positioned over the proximal part of the right fallopian tube.
Based on the visual and acoustic analysis of the Doppler frequency shift of the fluid bolus passing through the fallopian tubes, the tubes are classified as patent, partially obstructed, or completely obstructed (Fig. 7.3).
Patent tube. If the tube is patent, the pulsatile contrast injection flows into the intramural and adjacent proximal tubal segment, where the Doppler sample volume has been placed. The inflow phase is brief and characterized by a sharp rise in the Doppler frequency shift. Unobstructed distal outflow is characterized by a slow and steady decline in the Doppler shift over time (Fig. 7.3a).
Partial obstruction. With a partially obstructed tube, the Doppler spectrum shows a sharp initial peak caused by intratubal turbulence. This is followed by a brief stoppage of contrast flow, with absence of a Doppler shift, caused by increased peripheral resistance (Fig. 7.3b). If the contrast volume is able to surmount this resistance, the Doppler trace shows an additional phase of lower-frequency shifts as a sign of decreased outflow against a resistance. This phase is always of lower amplitude and shorter duration than in a patent tube.
Complete obstruction. If the tube is completely obstructed, the contrast medium enters the sample volume in the intramural part of the tube, where it produces short, intense Doppler shifts of low amplitude. There are no additional signals following these initial peaks, signifying an absence of outflow distal to the sample volume (Fig. 7.3c).
Color flow. When the flow of the contrast medium is additionally analyzed by color-flow imaging, the already intense signals from the Echovist solution may produce conspicuous noise and superimposed artifacts in the patent tube unless the sensitivity of the system for flow velocities is set extremely low. Color-flow analysis (flow direction, turbulence) is indicated only if the B-mode and spectral findings are equivocal or if an obstruction is suspected. Color flow is often the only technique that can detect the spillage of contrast medium from the fimbriated end of the tube.
Documentation. When Doppler scanning is added to the qualitative B-mode analysis, it becomes possible to make a rough quantitative evaluation of flow through the fallopian tubes. The entire examination is recorded on videotape, and selected images are documented with hard copies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree