Maged M. Costantine, MD
PRURITIC CONDITIONS ASSOCIATED WITH RASH
• Pruritic Urticarial Papules and Plaques of Pregnancy
• Atopic Eruptions of Pregnancy
• Pemphigoid Gestationis (Herpes Gestationis)
PRURITIC CONDITIONS NOT ASSOCIATED WITH RASH
• Intrahepatic Cholestasis of Pregnancy
INTRODUCTION
Pruritus is a common complaint that affects up to 14% of pregnant women.1 It usually affects the skin of the abdominal wall and, in the majority of cases, it is believed to be secondary to striae development and skin stretching and/or distention. Most skin specific lesions in pregnancy are pruritic and usually resolve after delivery. Essential for the workup of pregnant women with pruritic complaint is to discern the presence or absence of rash. In this chapter, we will elucidate a simple approach in the identification, diagnosis, and treatment of pruritus occurring in pregnancy. We will also elaborate an algorithm for simple workup and management of these conditions.
CLINICAL CASE
A 30-year-old G2P0010 at 34 weeks of gestation presents for prenatal care. Patient was complaining of generalized itching that involved her palms and soles. She said the itching is worse at night. Physical examination did not reveal any rash, jaundice, or hepatomegaly. Her prenatal labs showed hepatitis B surface antigen negative. Patient also reports history of hepatitis B vaccination. You ordered fasting bile acids, liver aminotransferase enzymes, and hepatitis C antibody. You additionally started the patient on ursodeoxycholic acid (UDA) 300 mg TID suspecting intrahepatic cholestasis of pregnancy. Patient was counseled and started on twice weekly nonstress test and an ultrasound for fetal growth was ordered. Laboratory results returned confirming the clinical suspicion with negative hepatitis C antibody, elevated fasting bile acids (47 μmol/L), AST 113 U/L, and ALT 145 U/L. You decide to continue UDA and antepartum fetal surveillance and discuss with the patient your plan to induce labor at 37 weeks.
PRURITIC CONDITIONS ASSOCIATED WITH RASH
Pruritic Urticarial Papules and Plaques of Pregnancy
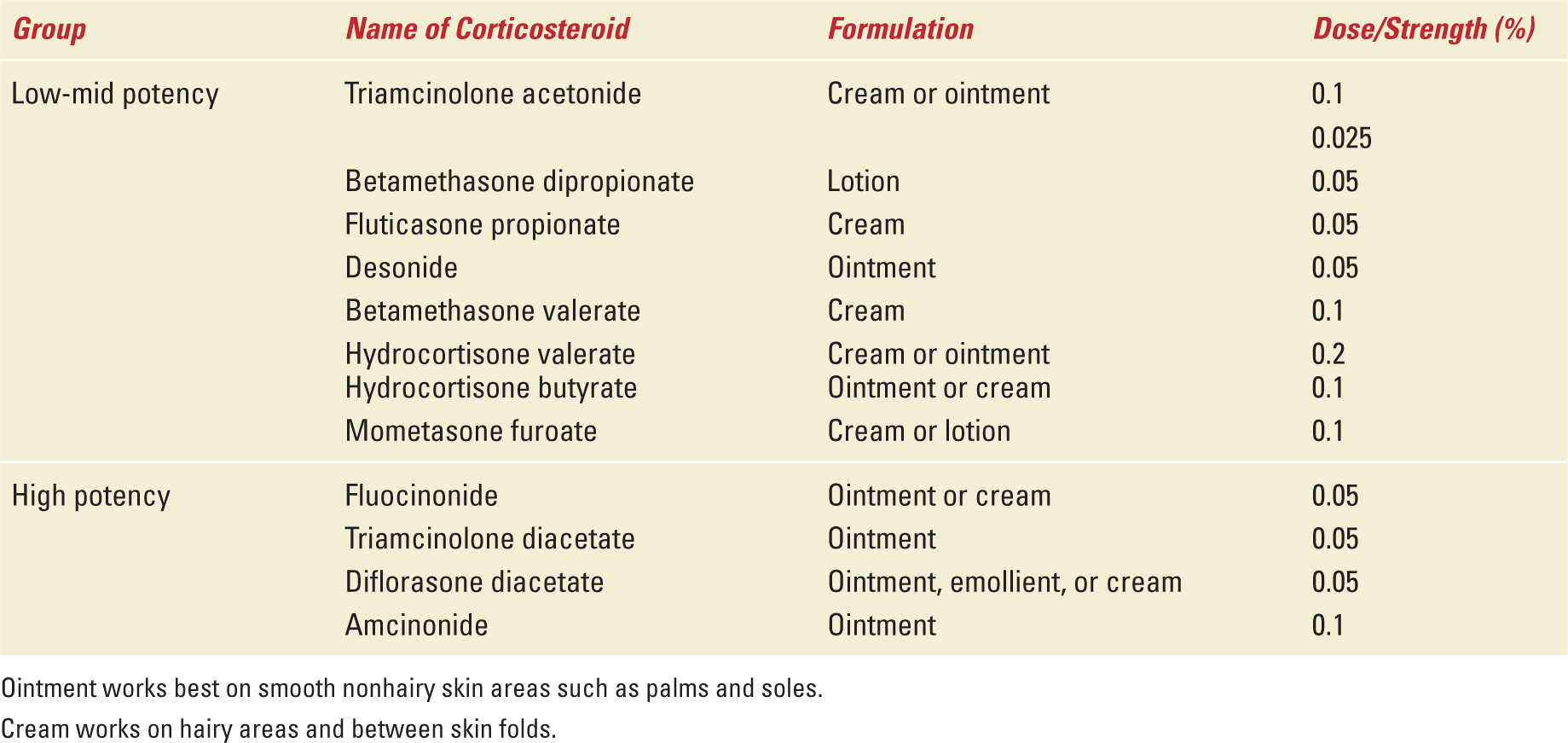
Pruritic urticarial papules and plaques of pregnancy (PUPPP) is the most common pruritic rash of pregnancy, complicating 1/160 to 1/300 pregnancies. It is also referred to as toxemic rash of pregnancy and was first reported by Holmes and Black in 1982 as a polymorphic eruption of pregnancy. Up to 75% of patients with PUPPP are nulliparous, and the condition is 8- to 12-fold more common in women with multiple gestations. Other risk factors include obesity and hypertension. The diagnosis of PUPPP is clinical; laboratory tests and skin biopsies are not required. PUPPP is characterized by erythematous papules that start in the abdomen, and later coalesce to form urticarial plaques.2 Abdominal striae are most commonly involved (more than 60% of patients) and the umbilicus and peri umbilical area are usually spared. The rash can spread to the thighs, buttocks, and arms while the face, palms, and soles are usually spared. The onset of disease is typically during the third trimester and it usually resolves within several weeks after delivery or immediately before delivery. PUPPP is associated with moderate to severe itching in up to 80% of patients. Unlike some of the other dermatoses of pregnancy, PUPPP is not associated with adverse maternal or fetal outcomes and the mainstay of management consists of symptoms relief using low to mid potency topical corticosteroids as initial therapy (Table 35-1) and nonsedating antihistamines. The disease does not recur in future pregnancies.3
Topical Steroid Therapy |
Atopic Eruptions of Pregnancy
Atopic eruption of pregnancy is a new terminology that includes eczema in pregnancy, prurigo gestationis, and pruritic folliculitis of pregnancy. They all share a common association with atopy. The rash usually appears at mid gestation and is characterized by nodular or papular patches with or without excoriations commonly accompanied by extensive pruritus. The extremities are usually involved.3 The recurrence rate in subsequent pregnancies is low and the rash usually resolves by 12 weeks postpartum.4 Management consists of low to mid-potency topical corticosteroids (see Table 35-1) for controlling symptoms and emollients to maintain adequate skin hydration. None of these conditions is associated with adverse maternal or fetal outcomes, and the prognosis is usually good.
Pemphigoid Gestationis (Herpes Gestationis)
Pemphigoid gestationis is an uncommon blistering skin disease that affects 1/1700 to 1/50,000 pregnancies. Herpes virus does not cause the disease but rather it is an autoimmune disease, and human leukocyte antigen haplotypes B8 and DR3/DR4 are believed to play a role in its pathogenesis.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


