Prune-Belly Syndrome
Frohlich first reported a neonate born with congenital absence of his abdominal musculature in 1839 and Parker later described the accompanying genitourinary tract abnormalities of hydroureteronephrosis, megacystis, and undescended testes (UDT).1,2 Combined, this triad comprises the condition known as ‘prune-belly syndrome’ (PBS), which was coined by Osler in 1901 (Fig. 61-1).3 Eagle and Barrett reviewed this rare, congenital syndrome and detailed the characteristic features that includes congenital absence or deficiency of the abdominal wall musculature, urinary tract abnormalities including a large hypotonic bladder (megacystis), dilated ureters, dilated prostatic urethra, and bilateral UDT.4 In addition, other anomalies, such as cardiac, pulmonary, gastrointestinal, renal and orthopedic can also be present.5 In an effort to quell the negative connotation that may be associated with this terminology, various other labels have been used, including Eagle–Barrett syndrome, triad syndrome, and abdominal musculature deficiency (AMD) syndrome.5–7 Despite the good intentions of the new nomenclature, the most widely accepted designation has remained ‘prune-belly syndrome.’
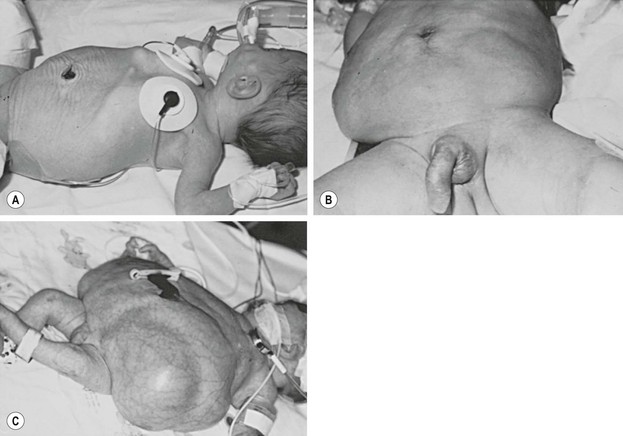
FIGURE 61-1 Variable degrees of abdominal wall laxity can be seen in patients with PBS. (A) Subtle wrinkling in a less severely affected infant. (B) Typical appearance. (C) Severely affected neonate. (Courtesy of D. M. Joseph, MD.)
The incidence of PBS is approximately 3.8 per 100,000 live births based on data from the Kids’ Inpatient Database.8 Of those affected, nearly 50% are white, 30% black, and 10% Hispanic. Children with incomplete forms of the condition may present with the typical abdominal wall changes, but no urologic or testicular manifestations. Using strict criteria for the definition of PBS, which includes cryptorchidism, all patients must be male. Female patients, however, with characteristic abdominal wall and urologic findings, make up a small proportion of patients with an incomplete form of PBS.9,10
Genetics
Genetic factors may play a role, yet no specific gene defect for PBS has been identified. Hepatocyte-nuclear factor-1β (HNF1β), a transcription factor responsible for regulating gene expression necessary for mesodermal and endodermal development, has recently become a gene of interest. Two case reports of PBS with interstitial deletions in chromosome 17q12 encompassing HNF1β have been described.11,12 However, recently, 32 patients with PBS were screened for the presence of HNF1β mutations and only 1 (3%) was found to have a mutation.13
A study evaluating consanguineous union of parents with two male offspring found to have PBS and three with posterior urethral valves point to two loci, 1q and 11p, with likely only one being the causative gene.14 Sporadic cases of PBS have also been associated with other chromosomal abnormalities, including Turner syndrome and trisomies 13 and 18.15–18
Embryology
The etiology for PBS is unclear. While there is no consensus, various hypotheses have been proposed to explain the usual constellation of findings. The most widely accepted mechanism is early urethral obstruction during gestation, leading to a massively distended bladder and ureters.19 This obstruction may be anatomic,20 but others have proposed a functional cause, potentially related to hypoplasia of the prostate.21 Regardless whether if it is functional or anatomic, the urethral obstruction with ensuing bladder distension is thought to lead to the classic abdominal wall muscle and skin changes. In addition, the high grade urethral obstruction and secondary bladder changes can lead to renal dysplasia with oligohydramnios and the subsequent pulmonary dysplasia that is seen in many PBS children. Finally, to account for the cryptorchidism, it is suggested that the distended bladder prevents the normal descent of the testes, thus explaining their intra-abdominal position.
Another reasonable hypothesis involves a primary mesenchymal defect early in embryogenesis that leads to incomplete differentiation or failure of migration of the lateral mesoderm. The failure of migration of the lateral mesoderm explains the typical abdominal wall appearance, but does not account for the genitourinary and testicular abnormalities.22 It is suggested that not only is there a defect in the lateral plate mesoderm, but there is also a defect within the intermediate plate mesoderm, which would then affect embryogenesis of the paramesonephric and mesonephric ducts.23
Clinical Features
Genitourinary Anomalies
Bladder
The bladder is usually very large and irregular with a patent urachus identified in approximately 25% of patients.4 PBS patients typically have a compliant bladder with a very large capacity and smooth wall that has an increased ratio of collagen to muscle fibers. Because of these findings, a delay in the first sensation to void is often seen.24 In some patients with severe muscle loss, the bladder will bulge and give the impression of a pseudodiverticulum most commonly seen at the dome of the bladder.7 The trigone is typically enlarged with displaced ureteral orifices laterally and superiorly, which likely contributes to the high incidence of vesicoureteral reflux (VUR).5,7 A poorly defined bladder neck opens into a dilated prostatic urethra. Many patients will void efficiently, but this can vary and some believe a relative outlet resistance exists. Regardless, PBS patients should be followed closely as their ability to empty can deteriorate.25
Ureters
The ureteral orifices are displaced laterally and superiorly, and typically are dilated and tortuous, particularly distally where the smooth muscle is not as normal compared to the proximal ureter (Fig. 61-2). The degree of ureteral pathology can vary and may even be segmental.26 Collagen fibers and connective tissue have been found to be abundant between muscle bundles containing few muscle cells. Thus, there is poor contractility of the ureter and the propulsion of urine is hindered, resulting in upper tract stasis.27,28 With the bladder and ureteral abnormalities, it is no surprise that approximately 75% of patients will have VUR (Fig. 61-3).29 It is rare, however, for PBS patients to have ureteral obstructions.30

FIGURE 61-2 This voiding cystourethrogram in a patient with PBS shows large, dilated distal ureters. The bladder is marked with an asterisk.
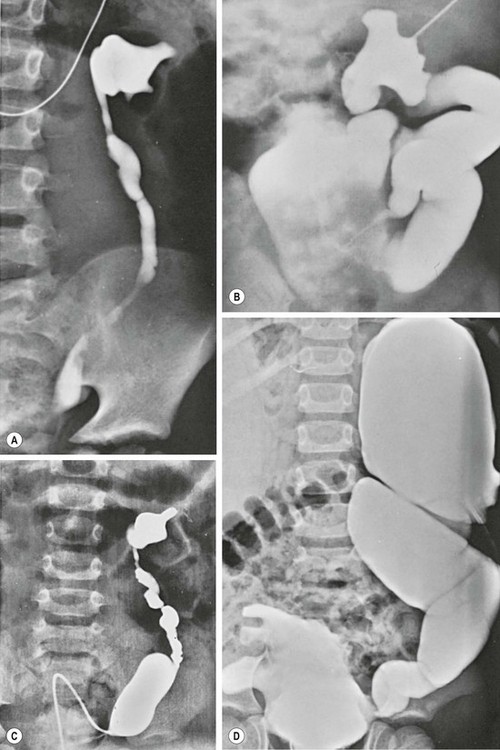
FIGURE 61-3 Variable degrees of dilation and dysmorphism of the upper urinary tract are seen in PBS. (A) Dysmorphic renal pelvis with mild ureteral dilation. (B) Calyceal clubbing and a tortuous ‘wandering’ ureter. (C) Dysmorphic pelvis with exaggerated dilation of the distal ureteral spindle. (D) Bizarre appearance of the collecting system as well as the bladder.
Kidneys
Renal abnormalities span a large spectrum ranging from completely normal to severe dysplasia. Of those with dysplasia, one kidney may be affected with a normal contralateral kidney.31 The mechanism for the renal abnormalities is uncertain but possibilities include bladder outlet obstruction and abnormal ureteral bud–metanephric blastema interaction.32
Hydronephrosis is typically seen and can be quite variable in spite of severe ureteral and renal pelvic distension. Most hydronephrosis is nonobstructive in nature, and the degree of hydroureteronephrosis does not directly correlate with the amount of parenchymal injury.30,32
Posterior Urethral, Prostate and Accessory Sex Organs
The extremely dilated posterior urethra seen in PBS children is thought to be secondary to generalized hypoplasia of the prostate epithelium with replacement of the normal smooth muscle anteriorly with connective tissue. While obstructive lesions are rare in the distal posterior urethra,29,33 several investigators have described valve-like obstructive tissue in this location.34–36
The prostate appears widened secondary to the loss of smooth muscle support. One theory supporting this finding is an abnormal epithelial–mesenchymal interaction (Fig. 61-4).20,37 Ejaculatory failure can result from this lack of normal prostatic parenchyma. Some patients may have retrograde ejaculation due to an incompetent bladder neck.34,38

FIGURE 61-4 Posterior urethral dilation (asterisk) is often found in children with PBS. This dilation is similar to that seen in boys with posterior urethral valves.
The vas and seminal vesicles are typically affected, with atresia commonly present. However, some patients present with dilation of both of these structures.23
Anterior Urethra
Typically the anterior urethra is normal. However, atresia of the bulbar or membranous urethra has been reported, occurring in 18% of patients in one review.39
PBS is also associated with two variations of megalourethra.40 The scaphoid megalourethra, the most common and less severe form, is associated with a deficiency of the spongiosum and preservation of the normal glans and corporal bodies (Fig. 61-5). The fusiform type has a deficiency of not only the spongiosum, but also of the corpus cavernosum.41 With voiding, the entire phallus enlarges in patients with the fusiform variety, while those children with the scaphoid form only have dilation of the anterior urethra.
Testes
Most children have bilateral intra-abdominal testes which are commonly found near the ureterovesical junction. More proximal locations have also been described.5,7 Data have varied regarding testicular histology in patients with PBS. Some reports have described normal testicular histology and other series have found diminished spermatogonia with Leydig cell hyperplasia when compared to normal controls, suggesting the testicular findings are caused by more than the cryptorchid state.7,42 Regardless of the histological findings, azospermia is the rule in adult PBS patients, with no reported cases of a natural paternity from patients with PBS.43
Extragenitourinary Anomalies
Abdominal Wall
The most characteristic clinical finding in PBS patients is the wrinkled and floppy appearance to the abdominal wall with bulging flanks and creased skin in the newborn. As patients age and the amount of cutaneous abdominal adipose tissue increases, a more potbelly appearance is noted. The degree of the ‘pruned’ appearance and deficiency of the abdominal wall musculature can vary significantly (see Figure 61-1). While rarely completely absent, the medial and inferior aspects of the abdominal wall are most severely involved, with normal or near-normal abdominal wall at the periphery.30,44 The most affected individual muscle is the transversus abdominis followed in decreasing frequency by the rectus abdominis inferior to the umbilicus, internal oblique, external oblique, and superior aspect of the rectus.29 While the innervation of the abdominal muscle appears unaffected, microscopy has found variations in or decreased muscle fiber size, excessive collagen accumulation, and myofilamentous disarray and loss.45
Cardiac
Cardiac anomalies are present in approximately 10% of affected children. The most common findings include patent ductus arteriosus, atrial and ventricular septal defects, and tetralogy of Fallot.46,47
Pulmonary
Pulmonary issues are common and typically related to the degree of renal dysplasia and oligohydramnios. Neonates exhibiting pulmonary distress should be presumed to have pulmonary hypoplasia and hyaline membrane disease. These children are also at increased risk for both pneumonia and spontaneous pneumothorax which is not necessarily related to the degree of hypoplasia.48 Older patients may be found to have significant restrictive lung disease thought to be related to musculoskeletal abnormalities rather than parenchymal lung disease.49
Gastrointestinal
The most common gastrointestinal anomaly is intestinal malrotation.29 This is thought to be due to an incomplete rotation of the midgut leading to a narrow mesentery.50 Other intestinal abnormalities include persistent cloaca, gastroschisis, omphalocele, imperforate anus, colonic atresia, volvulus, and anorectal malformation.50–53 A similar condition to PBS, known as megacystis-microcolon-intestinal hypoperistalsis syndrome (MMIHS), presents with a functional obstruction of the gastrointestinal tract with malrotation, microcolon, and a large nonobstructed bladder. Some have postulated a common pathogenesis, and a very rare case of both MMIHS and PBS has been reported.54,55 Chronic constipation can be a life-long issue and is believed to be due to lack of intra-abdominal pressure from the lax abdominal wall.
Musculoskeletal
Musculoskeletal abnormalities are common, occurring in approximately 50% of children.56–58 The most common orthopedic deformity is clubfoot, with an incidence of at least 25%, and nearly 50% are affected bilaterally.58 Other findings include congenital scoliosis, talipes equinovarus, and pectus excavatum.56,58
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



