Fig. 1
In this rare open proximal humerus fracture in an adolescent, the tent-shaped morphology of the proximal humeral physis is clearly displayed
The most important pathoanatomical considerations in treating proximal humerus fractures are related to the growth potential of the proximal humerus and the wide range of motion possible through the shoulder . The proximal humeral physis contributes 80 % of the length of the humerus, and the metaphyseal region of the humerus is capable of remodeling substantial amounts of displacement and angulation (Mooney and Webb 2009). The combination of physeal reorientation with growth and periosteal remodeling of bone accounts for the ability of growing bones to “straighten” themselves in very skeletally immature patients (Abraham 1989), and the proximal humerus may have the most remodeling potential of any area of the body. In addition, the growth potential and active periosteum of this area lead to rapid fracture union. Coupled with this, the wide range of motion of the shoulder can accommodate substantial residual deformity and angulation without functional loss. This explains the reason that the vast majority of proximal humeral fractures in children can be treated nonoperatively.
Assessment of Proximal Humerus Fractures
Signs and Symptoms of Proximal Humerus Fractures
Most patients with proximal humerus fractures present following a traumatic event and direct or indirect force application to the affected arm. The signs and symptoms of proximal humerus fractures are pain, decreased movement, swelling, and ecchymosis in older children, which may be delayed up to 24 hours after the injury. In infants the only sign may be “pseudoparalysis ” of the affected arm. Associated neurological or vascular injury is rare (Hwang et al. 2008). If there is axillary nerve involvement, it can be tested for by assessing sensation on the lateral shoulder in cooperative patients. Severe swelling and a pulsatile mass should prompt vascular examination, but the authors have never encountered a vascular injury in a skeletally immature patient with a proximal humerus fracture.
Imaging for Proximal Humerus Fractures
Good quality anteroposterior and lateral radiographs of the shoulder are needed to properly assess the fracture (Fig. 2). It is important to get a lateral view without rotating the arm, with a transthoracic or scapular Y-view preferred (Fig. 3). Rotating the arm will be painful in unstable fractures and will only provide a lateral view of the distal fragment. Contralateral shoulder radiographs are rarely of benefit but can be used for comparison in infants or younger patients. Advanced imaging is rarely needed in proximal humerus fractures. In infants ultrasound can be used to diagnose proximal humeral physeal injuries. Computed tomography or magnetic resonance imaging can be utilized to evaluate for a possible physeal arrest if deformity develops following fracture.



Fig. 2
Anteroposterior and lateral views of a proximal humerus fracture

Fig. 3
In this scapular-Y lateral view, there is 100 % displacement of the metaphysis (distal fragment) anterior to the proximal humeral epiphysis/humeral head
Radiographs should be carefully scrutinized to assess whether or not the bone is normal or abnormal, especially when the mechanism of injury involved minimal or minor trauma. The proximal humerus is a common site of pathologic fractures in skeletally immature patients, especially secondary to unicameral or simple bone cysts (Fig. 4). General management principles are to allow healing of the fracture first and then to address the benign bone lesion.
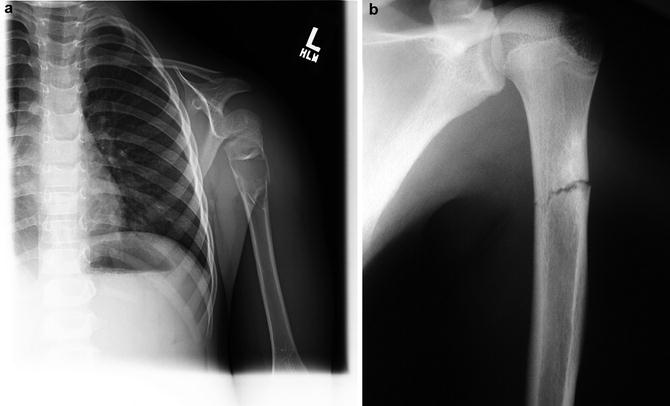
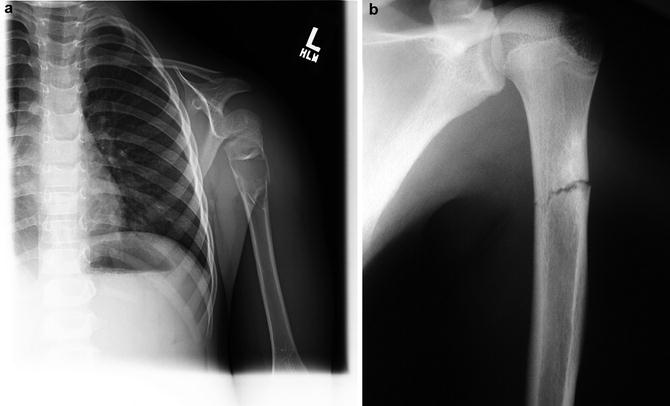
Fig. 4
(a) The most common pathologic lesion of the proximal humerus is a unicameral bone cyst as shown here. These frequently present with pathologic fracture following a minimal traumatic mechanism of injury. (b) When fractures are sustained after minimal trauma or secondary to muscle contractions in sport, the radiograph should be carefully scrutinized for a bone lesion that would weaken the bone. This fracture through a nonossifying fibroma was sustained when throwing a ball
Injuries Associated with Proximal Humerus Fractures
Neurovascular injuries are a rare complication of proximal humerus fractures, with a reported incidence of 0.4 %. There is increased likelihood with valgus displacement , as the metaphyseal fragment displaces medially and can impinge on the neurological structures exiting the axilla (Hwang et al. 2008). If nerve injury does occur, it is most likely to involve the axillary nerve, with lesser incidence of involvement of other nerves exiting the axilla. Vascular injury to the axillary artery is extremely rare in children.
The rotator cuff is a related anatomic structure that may be injured in proximal humerus fractures in adults, but is not typically involved in younger patients. Since the supraspinatus, infraspinatus, and teres minor insert onto the greater tuberosity and the subscapularis on the lesser tuberosity, contractile forces on the proximal fragment will usually result in abduction and some external rotation.
Proximal Humerus Fractures Classification
The Neer-Horowitz classification is used most commonly for proximal humerus fractures – it is confusing as the grade I uses millimeters of displacement, and grades II through IV use displacement as a percentage of the width of the shaft of the humerus: grade I, no or minimal displacement (<5 mm); grade II, less than 1/3 shaft width displacement; grade III, less than 2/3 shaft width displacement; and grade IV, more than 2/3 shaft width displacement (Neer and Horwitz 1965). This classification system is used to determine the method of treatment (operative vs. nonoperative) and the adequacy of reduction (Fig. 5). Classifying fractures using the Salter-Harris system can be used as well, with younger patients tending to have Salter-Harris type I fractures and older children and adolescents most commonly having Salter-Harris type II fracture patterns. As intra-articular (trans-epiphyseal) fractures (Salter-Harris types III and IV) and growth arrest following proximal humeral fractures are both exceedingly rare in the proximal humerus, the use of the Salter-Harris classification is not clinically very useful.
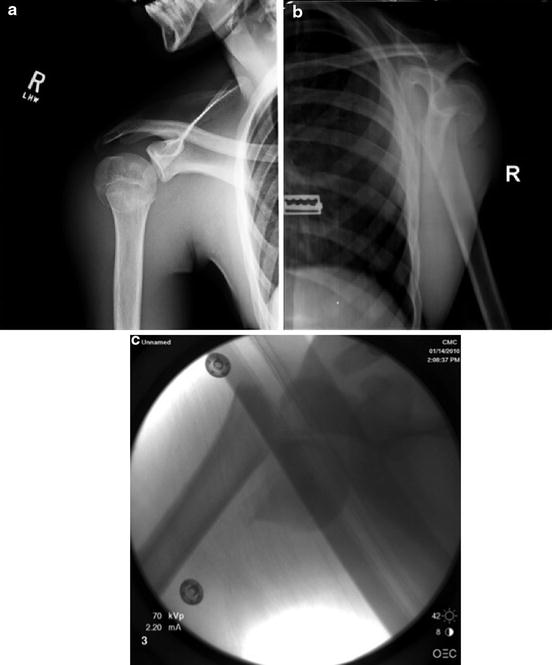
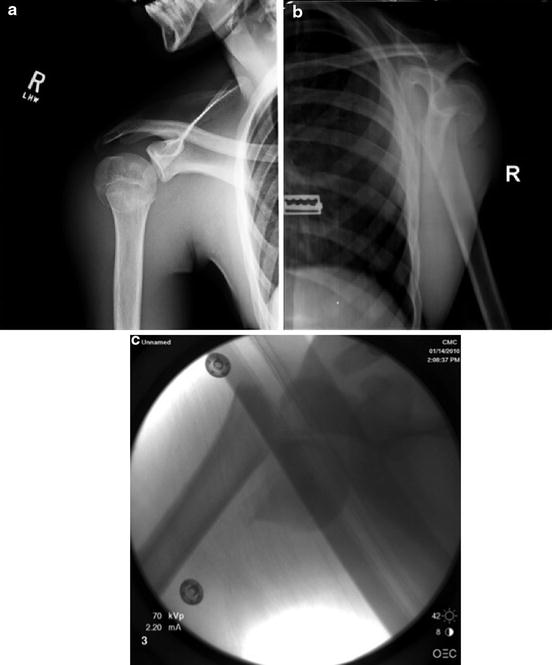
Fig. 5
Neer grade III or IV displacement. (a, b) shows a Neer grade III fracture in a 14-year-old linebacker sustained during a football tackle. (c) shows a Neer grade IV fracture sustained by a 15-year-old multitrauma patient who also had bilateral femur fractures
Proximal Humerus Fractures Outcome Assessment
The reported outcomes of proximal humerus fractures are almost always satisfactory, regardless of the method of treatment. This does not mean that an individual patient is guaranteed to have a satisfactory outcome, but it does make it quite difficult to perform rigorous outcome studies with the statistical power capable of determining the suitability of one treatment option over another for a particular patient. Currently such a study does not exist, and the majority of the literature available consists of small retrospective case series and the expert opinions of the authors. Assessment tools available to evaluate shoulder function outcomes after proximal humerus fracture include many standardized scores (Constant score, Hospital for Special Surgery (HSS) score system, and the American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form), but their value for injuries in this area is questionable. A recent retrospective case-control study comparing reduction and pinning to reduction and intramedullary rod fixation for proximal humerus fractures points out the difficulty in designing studies and using outcome assessments to discern clinically important differences in outcome based on treatment choices. In this large series of 73 skeletally immature patients, all achieved “clinical and radiographic healing without functionally limiting loss of global shoulder motion compared to the contralateral shoulder, pain or weakness” (Hutchinson et al. 2011).
Proximal Humerus Fractures Treatment Options
Nonoperative Management of Proximal Humerus Fractures
Indications/Contraindications
Most proximal humerus fractures can be treated nonoperatively and result in good radiographic healing and functional results (Table 1). Nondisplaced or minimally displaced fractures (Neer grade I or II) are treated with immobilization with a sling and swathe or sling for 2–3 weeks. In displaced fractures (Neer grade III or IV), closed reduction should be attempted in most cases (Fig. 6). In some very young children, even severely displaced fractures may be treated with only immobilization. In these cases, an above-the-elbow cast with a neck collar and cuff around the wrist to suspend the cast and allow it to apply traction to the fracture while the patient is upright may be used. This has been called “hanging arm cast ” treatment and can be effective for younger patients (less than 11 years) with displaced fractures (Fig. 7). Patients are instructed to sleep in a semi-erect position for 1–2 weeks after the fracture.
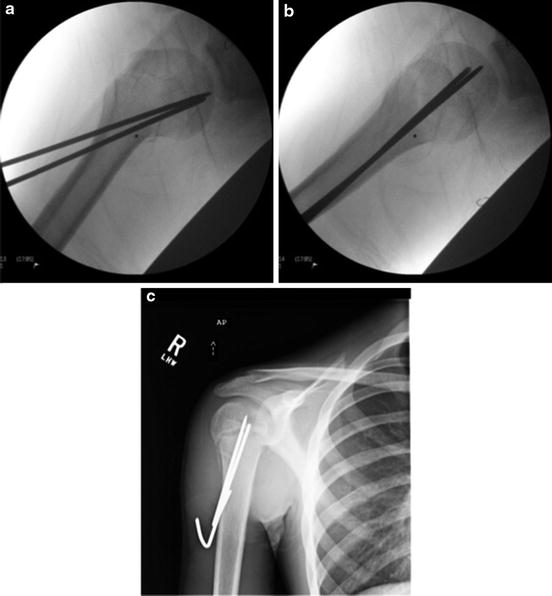
Table 1
Indications and relative contraindications for the nonoperative management of proximal humerus fractures
Proximal humerus fractures | |
|---|---|
Nonoperative management | |
Indications | Contraindications (relative) |
All patients < Neer grade II displacement | Severe displacement (Neer grade III–IV) |
Any amount of displacement in <12 years | Patient approaching skeletal maturity |
Neurovascular injury | |
Open fracture | |
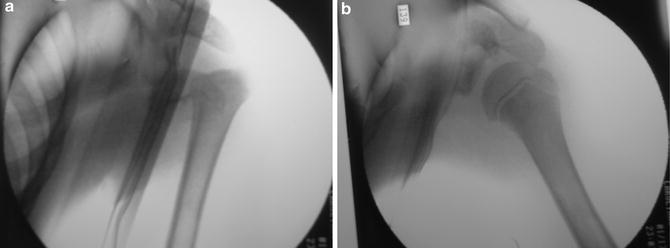
Fig. 6
This case nicely illustrates the value of attempting closed reduction, even in markedly displaced fractures. This 11-year-old had an apparent fracture dislocation (note inferior position of humeral head relative to the glenoid (a) and a completely displaced (Neer grade IV) fracture). The inferior subluxation may have been so-called pseudosubluxation. Traction, abduction, and external rotation resulted in an anatomic, stable reduction under conscious sedation in the emergency department (b)
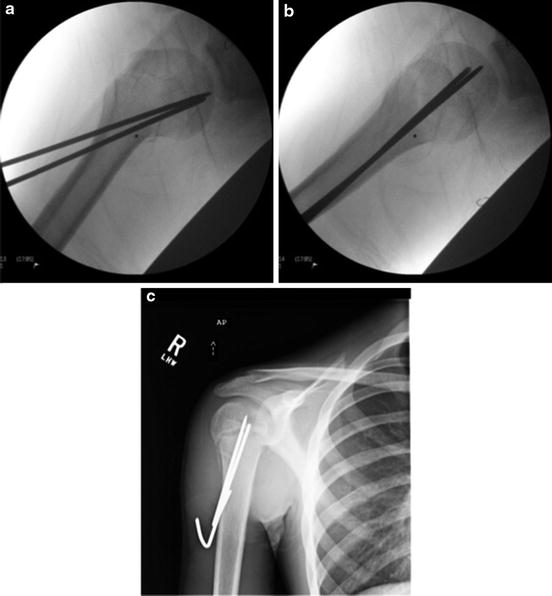
Fig. 7
Two large pins are used to stabilize a proximal humerus fracture after acceptable closed reduction (a, b). At 3 weeks early periosteal healing is noted and the pins are removed in the clinic. Note the large bends in the pins outside the skin (c)
Defining the amount of residual deformity after closed reduction that is “acceptable” is dependent on the age of the child; expert opinion by Beaty has provided some general guidelines – any amount of displacement and up to 70° angulation in children less than 5 years old, displacement up to 50 % width of shaft and angulation up to 40–45° in ages 5–12 years, and displacement of <30 % width of the shaft and up to 15–20° angulation in children greater than 12 years old (Beaty 1992). There are few specific contraindications to closed reduction – open fractures or fractures with vascular injury should be treated with open reduction .
Techniques
Closed reduction with immobilization: Closed reduction is achieved using traction, 90° of flexion, then 90° of abduction and external rotation. Occasionally manual pressure applied to the proximal aspect of the distal fragment (proximal metaphysis) from anterior to posterior is helpful to push the fragment back inside the soft tissue envelope as traction is applied. Once the closed reduction maneuver is performed, fluoroscopy can be used to assess the reduction with the arm held in abduction. Once reduced, the traction is then released, and some axial load applied from distal to proximal to attempt to engage the fragments and hold the reduction as the arm is brought back to the patient’s side. As in the management of all displaced fractures, the goal is to obtain an acceptable reduction and then maintain the reduction through fracture union. Often the difficulty in proximal humerus fractures is maintenance of the reduction as the arm is brought back to the side. Historically this resulted in treatment of these fractures with overhead traction or “salute” casts with the arm held in abduction, flexion, and external rotation (Mooney and Webb 2009). These techniques do not have a role in modern fracture management. After closed reduction, patients are placed in a sling and swathe, and post-reduction radiographs should be analyzed carefully. The position should be judged as acceptable or unacceptable. If mild residual varus is present, the use of a small abduction pillow between the elbow and the trunk can help maintain improved alignment. If acceptable, immobilization for approximately 3 weeks is all that is necessary. The patient can then begin progressive range-of-motion exercises. Formal physical therapy is rarely necessary in pediatric orthopedic practice after fracture. If the position is unacceptable, then closed reduction and fixation in the operating room is scheduled electively.
Outcomes
Fractures at this site tend to have very good outcomes as a result of increased growth (proximal humeral physis contributes 80 % of humeral growth) and remodeling that occurs here (Blount 1954; Salter 1970; Hohl 1976; Kohler and Trillaud 1983; Mooney and Webb 2009). Nonoperative management is the treatment of choice for the majority of proximal humeral fractures, even in severely displaced fractures (Bahrs et al. 2009). Large-scale studies of nonoperative management of proximal humerus fractures in the pediatric population, with 5 and 8 years of follow-up, have shown excellent functional and radiographic outcomes (Kohler and Trillaud 1983; Baxter and Wiley 1986). A recent review and meta-analysis, which studied 12 publications with follow-up ranging from 0.6 to 9 years, revealed no nonunions reported and few malunions (Pahlavan et al. 2011). Some of the long-term complications reported were stiffness, loss of motion, weakness, and functional limitations.
Operative Treatment of Proximal Humerus Fractures
Indications/Contraindications
Surgical intervention is indicated in the rare open fracture in this location; however, most operatively treated fractures will be severely displaced fractures in adolescents near skeletal maturity (Neer grades III–IV) (Table 2). In nearly all of these patients, the surgeon will be able to achieve closed reduction under fluoroscopy once adequate anesthesia is obtained. Intra-articular fractures in skeletally immature patients are very rare, but if encountered, the principles are the same as for displaced joint fractures in other locations. Anatomic restoration of the articular surface is desired provided that can be maintained until fracture union with the use of fixation. In young patients, stiffness is not as much of a concern as in adults, and so often, less rigid fixation that is easily removed is coupled with immobilization until fracture union.
Table 2
Indications and relative contraindications for the operative management of proximal humerus fractures
Proximal humerus fractures | |
|---|---|
Operative management | |
Indications | Contraindications |
Open fracture | Young children
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|