Fig. 1
TRS passive infant terminal devices

Fig. 2
Hosmer child passive hand

Fig. 3
Livingskin custom glove restoration
Voluntary opening terminal device : A voluntary opening (VO) terminal device is closed at rest. Cable and harness activation is required to open and grip an object. Rubber bands or springs hold the terminal closed. To open the device, the user must apply tension through the harness and cable. Relaxing the tension will close the terminal device on the object. The amount of grip force is controlled by the number of rubber bands or the tension of the spring.
Voluntary closing terminal device : A voluntary closing (VC) is open at rest. Cable and harness activation is required to close the terminal device to grip an object. To close the device the wearer must apply tension through the harness and cable. This tension must be maintained to maintain the grip. Relaxation will open the device. For activities and tasks that require long-term or sustained grip, the option of a locking mechanism is utilized.
Hook terminal devices are the most common voluntary opening terminal device and are made of stainless steel, aluminum, and titanium. They come in various sizes and shapes depending on the intended use. Pediatric hooks are typically aluminum and are canted in shape to allow better visualization of the object in the terminal device especially for fine motor tasks (Shurr and Cook 1990). They can also be coated or covered in a rubber material to improve cosmesis and to limit “slippage” of an object through the hook. Rubber bands around the “fingers” control the resistance to opening and closing. The more rubber bands, the heavier the object that can be held in the terminal device. But that also means the more “power” it will take to open and close the device through the cable and harness control system (Fig. 4).


Fig. 4
Hosmer pediatric voluntary opening hook terminal devices
Hands (mechanical hands ) are the other more common terminal devices. There are both voluntary opening hands and voluntary closing mechanical hands. They come in multiple sizes to best match the size of the contralateral hand according to metacarpal circumference or width. Prosthetic hands are worn with gloves, similar to the passive hands, which come in various shades. As with the passive hands, the gloves are not durable for children, get dirty/stained easily, and are difficult to clean. Although hands offer greater aesthetics, they tend to be less functional than hooks and are heavier in weight. Their friction is internal and only a prosthetist can adjust it so they have limited pinch force. In addition, the glove can restrict the motion making it more difficult to open and close especially for younger users. The most obvious limitation is the fingers (primarily digits 4 and 5) tend to “get in the way of the user” preventing picking up of smaller and flatter objects with compared to the hook. Younger children have greater difficulty controlling a hand as compared to a hook (Fig. 5).


Fig. 5
Hosmer voluntary opening and voluntary closing hand
Hook Versus Hand
The decision to go with a hook or a hand is unique to every patient. As noted above there are pros and cons to both. Typically parents of younger children feel strongly about getting a “hand.” Adolescents and older users frequently request a mechanical hand for aesthetic reasons. It is important for the team to discuss these issues with the user and family so that a decision can be made to meet both their expectations and functional goals. The decision in choosing a hook or hand can very well contribute to prosthetic abandonment whether it be for lack of appearance or secondary to lack of function. Encouragement of trying both terminal devices along with receiving therapy is recommended. The option of having a hook and a hand, especially for older children and adolescences, is an option as well. The terminal devices are relatively easy to change, and most users and families can learn to do this easily.
Child Amputee Prosthetics Project (CAPP) terminal device is a voluntary opening terminal device designed and developed by Carl Sumida, CPO, at UCLA in the mid-1970s. The CAPP terminal device is neither a hook nor a hand. It is made of rubber and has a center-pull to activate opening and closing of the terminal device. The benefit of the CAPP terminal device is that it provides secure grip and excellent pinch (Shaperman 1975). Appearance of the CAPP is sometimes an issue for the user and family. While it may be more functional than a mechanical hand, it is sometimes not well accepted by users and families (Fig. 6).


Fig. 6
CAPP terminal device
Life-touch terminal device is voluntary closing and was introduced in the late 1990s. It has more of the anthropomorphic detail of the hand (with 5 digits), but the fourth and fifth digits are flexed to minimize the issues of the hand’s digits getting in the way when picking up smaller and flatter objects. It is a common terminal device for younger children as it is very functional especially for fine motor tasks. It is limited in grip force as it is voluntary closing. As noted above a locking mechanism can be utilized on the socket for activities requiring prolonged grip (Fig. 7).


Fig. 7
TRS voluntary closing lite touch hand. TRS Catalog. http://www.trsprosthetics.com/catalog-view
Wrist Units
Wrist units are laminated into the distal end of the forearm of the prosthesis. As noted above the wrist unit provides the connection between the terminal device and the prosthesis. In addition it provides passive supination and pronation of the terminal device and friction in the wrist to maintain the terminal device in desired position.
Friction wrist is the most common wrist unit. It is most often round and comes in various sizes: infant, child, medium, and large. The oval-shaped wrist unit is used only for wrist disarticulation deficiencies. The friction on the wrist unit is adjusted with a small Allen wrench that goes into an Allen screw on the side of the wrist unit. Turning the Allen wrench in the clockwise direction increases the friction (inhibiting rotation of the terminal device) and counterclockwise to decrease the friction (allowing easier rotation of the terminal device). Adjusting the friction is easily done by the user (younger children will need assistance) only when needed depending on the functional need for the desired task (Fig. 8).


Fig. 8
Hosmer friction wrist
Flexion wrist while providing for friction also allows for three locking positions of the wrist: neutral (zero degrees), 30°, and 5° of flexion. It is predominantly used with bilateral deficiencies on the dominant side to assist with activities of daily living such as dressing, eating, toileting, etc. Flexion of the wrist allows the terminal device to get closer to the body without requiring shoulder internal rotation. It can also be helpful for some recreational activities that require wrist flexion like violin and guitar. The flexion wrist unit is heavier than the friction wrist, so it is typically not recommended unless there is sufficient need for functional use (Fig. 9).


Fig. 9
Hosmer wrist flexion unit
Quick disconnect wrist allows for rapid change of terminal devices. The user pushes a button (or presses the button against an object) to release one terminal device and then replaces and secures another in its place. This is a much easier and faster process than screwing and unscrewing the terminal device each time a change is needed. This is especially useful if the user has a hook and a hand or when they have activity-specific terminal devices. It is not needed for infrequent need to change terminal devices (Fig. 10).


Fig. 10
Hosmer quick disconnect wrist
Flexible hinges are commonly used in the medium and long transradial prostheses and elbow disarticulation prostheses. In those instances the socket is much lower on the residual limb, allowing for greater range of motion (elbow flexion, supination, and pronation) and comfort. The flexible hinges assist with suspension of the prosthesis. The hinges are made of Dacron or leather and are attached proximally to a triceps pad (which is attached to the harness) and distally to the midline of the forearm of the prosthesis. Their purpose and function is to assist with suspension and stabilization of the prosthesis during active forearm supination and pronation (Fig. 11).


Fig. 11
Flexible hinges
Elbow Joint
Transhumeral and shoulder disarticulation prosthesis requires an elbow unit to provide elbow flexion and extension in order for the terminal device to grasp, hold, and release an object in the desired elbow position. The elbow is activated and controlled with the cable and harness along with shoulder and scapular motion. The prosthetic elbow must be positioned prior to activating the terminal device. Scapular and biscapular motion will flex the elbow to the desired or required position. The elbow is then locked into position at which time scapular and biscapular motion will open or close the terminal device (depending if it is voluntary opening or voluntary closing) to pick up the object and complete the task.
A pre-flexed elbow is used with very young children (less than a year old). There are currently no prosthetic elbow units small enough nor is there a functional or developmental need for bimanual tasks. The goal of the prosthesis at this age is to assist with sitting balance, crawling, and getting the user accustomed to wearing a prosthesis. This design simply creates a longer socket originating proximally at the shoulder and extending down to the wrist unit and terminal device. The socket is flexed approximately 30–40° to assist with crawling and sitting.
A Passive friction elbow is a lightweight friction elbow which also allows for passive humeral rotation. It is not connected to the cable system or harness. It is passively positioned by the contralateral hand or an object such as a table, counter, or desk. It is used with young children who have the functional need for elbow flexion but do not yet have the developmental skills to utilize a cable-activated elbow unit. The friction is sufficient to position the elbow to activate the terminal device but is not sufficient for holding and lifting heavy objects. It offers greater function over the pre-flexed elbow and is the precursor to a locking elbow (Fig. 12).


Fig. 12
LTI friction elbow
Locking elbows allow the prosthesis to flex and lock into position. At rest the prosthesis is not locked. The elbow can “free swing” in walking and running as does the anatomic elbow. As described the cable that controls the elbow is connected to the harness. Tension to the cable flexes the elbow, and it is then locked into position with shoulder depression, abduction, and extension (all at the same time). The terminal device is then able to open or close (depending on whether it is voluntary opening or voluntary closing) as described above. When the task is complete or the elbow position needs to be changed, the same shoulder motions are performed to unlock the elbow. If a new position is required, the process will need to be repeated. Outside locking hinges are used with elbow disarticulation deficiencies. They come in three sizes (child, medium, and adult) and allow for seven different locking positions. Inside locking elbows are used with transhumeral and shoulder disarticulation prostheses. Inside locking elbow units allow for 11 different locking positions and also allow for passive internal and external rotation (substituting for humeral rotation) of the forearm via the turntable. This friction-controlled rotation easily allows the user to passively position the forearm using either the contralateral hand or an object. The friction is constant and does not often need to be adjusted. But when necessary it can be adjusted easily with an Allen wrench. Younger pediatric users sometimes have difficulty locking and unlocking the elbow even with training and practice. One option typically used especially with the unilateral user is to manually control the lock with a “pull strap” fabricated with Dacron. The user will flex the elbow to the desired position, then use their contralateral hand to pull the Dacron loop to lock the elbow so that the terminal device can be activated, and then manually pull the loop again to unlock the elbow. This is typically done for a limited period of time, during initial training, and used only until the user progresses and masters to the more conventional method as described above (Fig. 13).


Fig. 13
Hosmer locking elbow
A forearm lift assist is an adjustable spring that can be added to the locking elbow when the user cannot produce sufficient tension to flex the elbow throughout the full and desired elbow range of motion. It makes it much easier to achieve full elbow flexion. This is particularly important when trying to get the terminal device close to the face or mouth for feeding, shaving, or to assist with dressing and hair grooming. While adding a little more weight, it can be very helpful in optimizing function with the elbow and the prosthesis.
Shoulder Joint
The shoulder is not a joint easy to replace mechanically. Prosthetic options for a shoulder disarticulation or forequarter prosthesis are limited. They offer the ability to passively position the shoulder in flexion, extension, abduction, and adduction with constant (but adjustable) friction. The joint can be locked into position using a cable or switch when needed (Fig. 14).
Socket design : All upper extremity prosthetic sockets are made from a model of the residual limb. The total contact socket is fabricated from thermoplastic or laminated material. It is the foundation for the entire prosthesis. While not weight bearing a well-fitting socket is still required for comfort as well as to optimize the functional outcome of the components, elbow and terminal device. A less than satisfactory socket has a direct effect on the efficiency of the cable and harness and will result in less than optimal function, which may result in the user not wearing, rejecting, or abandoning the prosthesis.
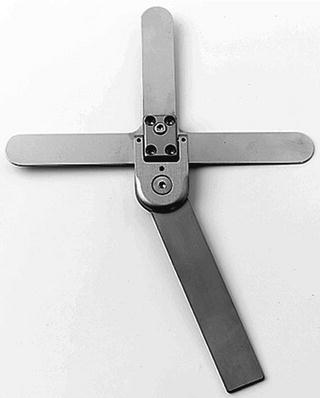
Fig. 14
Hosmer shoulder
Wrist disarticulation and transradial sockets vary in design depending on the length of the residual limb. The longer the residual limb, the more distal the socket trimlines, and the more active pronation and supination are permitted. Typically for mid to long residual limbs, the socket is below the humeral epicondyles but contains the olecranon. Residual limbs shorter than 50 % of the forearm length require more proximal trimlines. This socket typically includes the humeral epicondyles, olecranon, and extends anteriorly to or just distal to the cubital fold. This trimline can limit the elbow flexion range of motion beyond 100°, which can limit the ability of the user to get the terminal device to their mouth, but aids in suspension of the prosthesis. This socket design is sometimes referred to as a “self-suspending or Muenster socket.”
Elbow disarticulation sockets include the humeral epicondyles and can be bulbous in shape. This can tend to result in a larger bulkier socket. In addition the elbow unit must be placed beneath the socket, and this results in the mechanical elbow being distal to anatomic elbow on the contralateral side. Aesthetically this can be an issue, but users tend to have good control of the elbow and terminal device as compared to higher level upper limb deficiencies.
Transhumeral sockets vary in design according to the length and shape of the residual limb. Similar to the transradial socket, the trimlines are determined by the length of the residual limb. The shorter the residual limb, the more proximal the trimlines need to be extended over the acromion, the scapula, and the pectoral muscles. The socket must fit adequately to control rotation and migration of the socket. This is more of an issue in the transhumeral socket than the transradial or elbow disarticulation socket. An ill-fitting socket will limit and interfere with activation of the elbow and terminal device. A well-fit, controlled, and suspended prosthesis is much easier to operate and will assist with maximizing functional outcomes with the elbow and terminal device.
Shoulder disarticulation sockets are often a challenge in that they need to extend in all planes to maximize fit and comfort, minimize rotation and migration, and distribute the weight of the entire prosthesis over a greater surface area to avoid pressure and breakdown on the bony residual limb and acromion process. Flexible inner sockets fabricated with thermoplastics and silicones (for comfort) along with a more rigid frame (for stability) are a commonly preferred design.
Suspension
Locking/lanyard liner: Silicone or similar liners are commonly used in transradial and transhumeral prostheses. In most instances a prefabricated liner can be utilized. They come in many sizes, thicknesses, and material options. The liner is rolled directly onto the residual limb. Each locking liner has a locking “pin” on the distal end which engages into a lock which is laminated directly into the socket. The liner will remain “locked” into the socket until a button on the distal medial side of the socket is pressed at which time the pin disengages from the lock and the socket can be removed. The alternative to a locking pin liner is a lanyard, or strap, made of Dacron or leather that is attached to the socket either at or near the distal end of the liner. The strap then exits the socket through a small cutout in the medial wall of the socket. The Velcro strap attaches to the outside of the socket, typically on the medial wall of the socket. The Velcro strap is removed for doffing of the prosthesis. A major benefit of pin or lanyard lock is decreased dependence for suspension of the prosthesis on the harness. While the harness is still required and it will aid in suspension and control of rotation of the socket, with a locking liner the harness can be dedicated to maximizing operation of the terminal device and elbow. It is important to note that while this system is excellent for suspension of the prosthesis, neither the locking nor lanyard locking liners eliminate the issue of socket rotation and proximal “gapping.” Adequate suspension along with optimal fit of the socket is required to maximize the usefulness and functional outcomes with the prosthesis (Fig. 15).




