a Can be administered at full doses in anephric patients receiving hemodialysis.
Acute or chronic renal insufficiency is common in gynecologic cancer patients due to tumor-mediated obstruction, drug-induced toxicity, or advanced age. The incidence of moderate renal insufficiency dramatically increases with advanced age. For example, in the 60- to 69-year age group, over one third of women have an estimated glomerular filtration rate (GFR) of less than 60 mL/min/1.73 m2 (Fig. 1.1). In addition, serum creatinine levels can be inappropriately low as a consequence of reduced muscle mass, malnutrition, or alterations in fluid balance, and any of the standard formulae will overestimate GFR. This has potential clinical consequences for drugs such as carboplatin, where dosing is based on renal clearance.
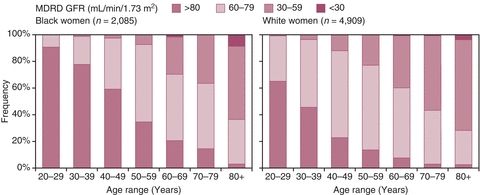
Figure 1.1 Distribution of renal function in nondiabetic adults. Weighted distribution of predicted GFR (mL/min/1.73 m2) based on the MDRD formula from the Third National Health and Nutrition Examination Survey (NHANES III). Source: Adapted from Clase CM, Garg AX, Kiberd BA. Prevalence of low glomerular filtration rate in nondiabetic Americans: Third National Health and Nutrition Examination Survey (NHANES III). J Am Soc Nephrol. 2002:13:1338–1339, with permission.
Several methods are available to estimate GFR (Table 1.2). All of these formulae are based on stable normalized biologic parameters and are less useful in the setting of dynamic changes following acute renal injury or nonrenal fluctuations in serum creatinine and fluid status, such as those that might occur in the postoperative setting or in the presence of large-volume ascites or in patients with abnormal muscle mass. While urine collection for the measurement of creatinine clearance might be thought to provide a better estimate of GFR, it is also subject to great variability in clinical practice. The use of 51Cr-ethylenediamine tetraacetic acid clearance remains the standard for the measurement of GFR, but it is rarely used in clinical practice due to the cost and complexity associated with radioisotopes.
Table 1.2 Commonly Utilized Formulae to Estimate Creatinine Clearance (CRCL, mL/min)
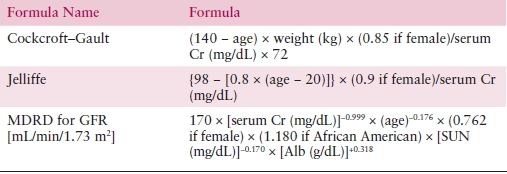
Alb, serum albumin concentration; BSA, body surface area; Cr, creatinine; GFR, glomerular filtration rate; MDRD formula, the Modification of Diet in Renal Disease study equation; SUN, serum urea nitrogen concentration.
Metabolism and Pharmacogenomics
With the expanded knowledge of metabolic pathways and awareness of polymorphisms in key enzymes, it is sometimes possible to identify individuals with a dramatic increased risk of toxicity. For example, dihydropyrimidine dehydrogenase (DPD) controls the rate-limiting step in fluoropyrimidine metabolism, and approximately 10 variant DPD alleles can occur with sufficient frequency to merit consideration of screening, as patients with less active DPD can be at risk for life-threatening mucosal injury and bone marrow suppression after receiving a single standard dose of 5-fluorouracil. While methods are available for screening, current assays can be expensive, and the potential reduction in risk needs to be balanced against the costs of a widespread screening program.
Uridine diphosphoglucuronosyl transferase 1A1 (UGT1A1) is responsible for the glucuronidation of bilirubin and a number of drug metabolites, most notably SN-38, the major active metabolite of irinotecan. Patients with a deficiency in UGT1A1 are at increased risk for life-threatening diarrhea and bone marrow suppression after receiving irinotecan. While the UGT1A1*28 promoter mutation has been studied most extensively, mutations in the coding region can also occur, particularly in Asian populations, and may predict for efficacy in addition to toxicity. Gilbert syndrome is associated with a mild unconjugated hyperbilirubinemia and reduced activity of UGT1A1 that is also associated with an increased risk of toxicity in both homozygous and heterozygous patients.
Drug Interactions
During routine care, patients may receive a variety of drugs, including antiemetics, antihistamines (H1 and H2), steroids, nonsteroidal anti-inflammatory agents, anticoagulants, narcotics, and anti-infective agents. Particular attention should be placed on drugs that could alter renal function, such as aminoglycoside antibiotics, nonsteroidal anti-inflammatory agents, and diuretics in patients with reduced fluid intake.
Increased attention has been focused on drug metabolism and potential interactions at the level of CYP isozymes, particularly CYP-3A4, which is potentially linked to the metabolism of nearly half of all pharmaceutical agents. Drugs that are substrates for the same isozyme may competitively inhibit metabolism, but these interactions are usually not of clinical consequence. Drugs that directly inhibit CYP isozymes without being a substrate for that isozyme are more likely to have clinical consequences. These include itraconazole, ketoconazole, fluconazole, and erythromycin. Other drugs act as inducers of CYP isozymes by increasing gene expression or protein levels, such as glucocorticoids, barbiturates, and rifampin, which can increase the net activity of CYP-3A4, resulting in decreased concentrations of susceptible compounds. Among the anticancer agents that are substrates for CYP-3A4 are cyclophosphamide, ifosfamide, docetaxel, etoposide, paclitaxel (also CYP-2C8), vincristine, vinblastine, tamoxifen, and gefitinib.
Owing to the diversity and rapid adoption of new chemotherapy and nonchemotherapy compounds, information regarding drug interactions is best obtained from online databases (e.g., http://www.medicalletter.com, http://www.micromedex.com, or http://www.druginteractioninfo.org/Home.aspx) or from the drug manufacturer.
DRUG RESISTANCE AND TUMOR CELL HETEROGENEITY
KEY POINTS
- The emergence of drug resistance limits the curative potential of chemotherapy.
- Dosing of chemotherapy must consider the setting and objective of treatment. More intense regimens are best utilized in the adjuvant or neoadjuvant setting.
- Treatment monitoring often encompasses repeat measurements of tumor sites identified on imaging. The common standard to interpret tumor measurements on clinical trial utilizes RECIST criteria.
- Chemotherapy can result in significant toxicities. Patient education and provider knowledge are key to managing the complications of treatment.
The curative potential of chemotherapy is limited by the emergence of drug resistance, which can be either intrinsic or acquired, and may involve one drug or multiple agents (pleiotropic resistance). Of note, tumors with intrinsic drug resistance to natural products tend to arise from duct or other cells lining excretory organs.
Intrinsic drug resistance is likely due to the clonal selection of tumor subpopulations that have survived previous chemotherapy exposure. In contrast, acquired drug resistance develops through somatic mutations, regulation of gene expression, or other phenotypic alterations. Of these, acquired resistance mechanisms may have a reversible component that could influence the timing and selection of subsequent chemotherapy.
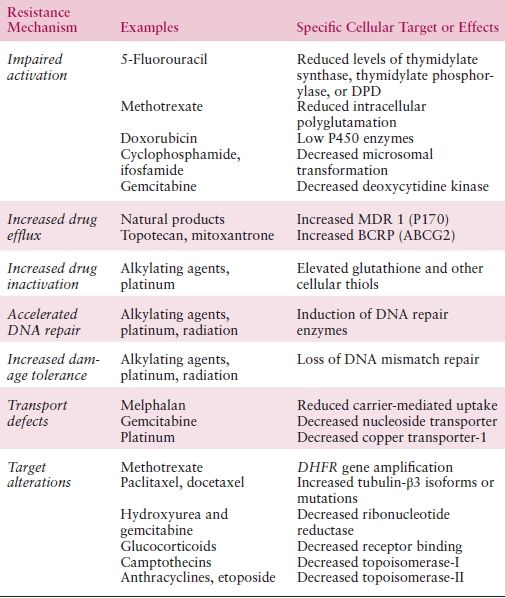
There are two major patterns of drug resistance in gynecologic oncology: (i) pleiotropic drug resistance associated with the overexpression of membrane-associated transport proteins, such as MDR1 (P170 glycoprotein), which has maximal impact on natural products, including the anthracyclines, vinca alkaloids, and taxanes and (ii) resistance due to reduced cellular uptake as a result of the loss of membrane transport proteins, increased detoxification of intermediates by glutathione production, increased damage tolerance due to defective detection, and/or apoptotic signaling, and expanded capacity of DNA repair. These second mechanisms are predominantly responsible for resistance to alkylating agents, including the platinum compounds (Table 1.3).
Table 1.3 Specific Mechanisms of Tumor Drug Resistance
Platinum Resistance and DNA Repair
Multiple mechanisms are associated with platinum resistance and point to potentially important clues to increase the cytotoxicity of these agents.
As a highly polar compound, cisplatin enters cells relatively slowly. Thus, the uptake of platinum can be influenced by several factors, including cation concentrations, pH, and the presence of reducing agents. Membrane transporter proteins, particularly the copper transporter-1 (CTR1), have been shown to play a substantial role in platinum influx. In addition, down-regulation of CTR1 has been shown to be a mechanism of platinum resistance.
Another mechanism of platinum resistance is associated with elevated levels of cellular glutathione (GSH), which also is associated with resistance to other alkylating agents and radiation therapy (RT). However, the exact mechanism by which GSH and other thiol compounds modulate cytotoxicity is unknown.
Enhanced capacity for DNA damage tolerance and repair can play a role in drug resistance to alkylating agents and cisplatin. Loss of DNA mismatch repair system genes such as MLH1 is not uncommon in ovarian cancer, and this appears to increase after exposure to platinum compounds. In addition, functional loss of MLH1 activity in patients with ovarian cancer can occur through hypermethylation-mediated silencing of the MLH1 gene following platinum exposure.
Nucleotide excision repair (NER) is the primary mechanism to remove platinum–DNA adducts from genomic DNA. Excision repair cross-complementing 1 (ERCC1) is a critical gene in the NER pathway, and increased mRNA levels of ERCC1 have been associated with platinum resistance. In addition, ERCC1 may also be prognostic, independent of chemotherapy. In one study of patients with lung cancer, patients assigned to observation who had ERCC1-positive tumors had better survival compared to those whose tumors were ERCC1-negative.
The association between ovarian cancer risk and mutations in BRCA1 and BRCA2 sparked interest in DNA repair after it was recognized that patients with BRCA1/2-associated tumors had improved outcomes compared with those without such mutations. One explanation of this was the association of BRCA1/2 mutations and increased response to agents that target DNA, such as the platinum compounds. How to incorporate drugs that inhibit DNA repair in tumors with loss of BRCA1/2 remains an area of active investigation.
Taxane Resistance
The subject of taxane resistance continues to be an area of active investigation. Overexpression of the drug efflux protein MDR-1 has consistently been associated with resistance to paclitaxel in cells and in retrospective analyses. However, prospective trials that combined an MDR-1 inhibitor with taxanes failed to improve clinical outcomes.
Mutations in the β-tubulin subunit have been associated with paclitaxel resistance in some preclinical models, but this does not appear to be a common mechanism. Still, expression of the tubulin-β3 isoform has been linked to cell survival pathways with a potential impact on clinical outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


