Preterm Labor and Preterm Premature Rupture of Membranes
Julie S. Solomon
Janyne E. Althaus
PRETERM LABOR
Preterm labor (PTL) is defined as:
Regular uterine contractions with cervical change before 37 weeks’ gestation
Extreme PTL occurs before 28 weeks’ gestation.
Incidence and Significance
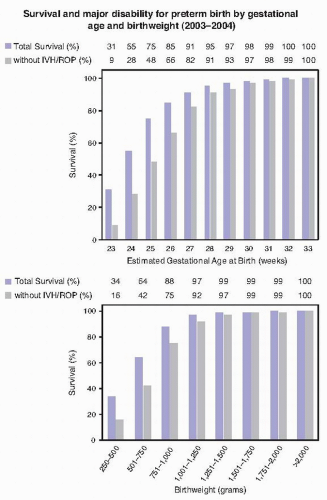
PTL is the leading cause of neonatal morbidity in developed countries (Fig. 9-1).
PTL accounts for 40% to 50% of preterm births. Other causes include preterm premature rupture of membranes, placental abruption, and indicated deliveries. Of the 4 million US births in 2010, 480,000 or 12% were preterm deliveries.
Short-term neonatal morbidity includes respiratory distress syndrome (RDS), hypothermia, hypoglycemia, jaundice, intraventricular hemorrhage, necrotizing enterocolitis, bronchopulmonary dysplasia, sepsis, and patent ductus arteriosus.
Long-term neonatal morbidity includes cerebral palsy, mental retardation, and retinopathy of prematurity.
Etiology
Risk factors include:
Previous spontaneous preterm delivery (PTD):
Most significant risk factor for PTL
Recurrence rate is 17% to 30%.
Infection:
Systemic or local infections including urinary tract infections, pyelonephritis, bacterial vaginosis, sexually transmitted infections, pneumonia, appendicitis, periodontal disease
Chorioamnionitis affects 25% of PTDs.
Pathogens include Ureaplasma urealyticum, Mycoplasma hominis, Gardnerella vaginalis, Peptostreptococci, and Bacteroides species.
Release of cytokines from endothelial cells, including interleukin-1, interleukin-6, and tumor necrosis factor-α, stimulates a cascade of prostaglandin production that stimulates uterine contractions.
Uterine overdistension: multiple gestation, polyhydramnios
Short cervix
History of cervical manipulation
Uterine malformations: bicornuate uterus, leiomyomata, uterine didelphys
Second- or third-trimester vaginal bleeding: placenta previa, placental abruption
Other: anxiety, depression, stressful life events (divorce, separation, death), low level of education, low socioeconomic status, African American race, maternal age (younger than 18 or older than 40 years)
Prevention
Any discussion on the prevention of PTD should note that the most important risk factor, history of prior spontaneous PTD, cannot be modified.
Educate patients about the early signs of PTL.
Treat infections promptly, especially urinary tract infections and lower genital tract infections.
It is notable that treatment of some infections, such as trichomoniasis, actually increase risk of PTD.
Treatment of infection may not remove risks.
The mechanism of causation may be from associated inflammation rather than infection.
Empiric broad-spectrum antibiotics have not been shown to reduce PTL and delivery and are associated with neonatal morbidity.
Chorioamnionitis is an indication for delivery, and PTD should not be avoided in this case.
Broad-spectrum treatment should take place while moving towards delivery.
Progesterone supplementation with 17-hydroxyprogesterone (17-OHP)
Dose:
250 mg of 17-alpha-hydroxyprogesterone caproate intramuscularly (IM) every week
progesterone vaginal suppositories (90 to 200 mg) every night at bedtime
Progesterone has been shown to prolong gestation for women with prior history of PTL.
Vaginal progesterone has been shown to prolong gestation for women with a short cervix <20 mm.
Suggested therapy begins at 16 to 22 weeks of gestation and is continued until 33 to 36 weeks of gestation.
There is no evidence to support progesterone therapy for patients with active PTL.
Cerclage
There are different techniques of cerclage placement, and a variety of nonabsorbable suture material can be used (see Chapter 8).
Progesterone supplementation can be considered, where indicated, in addition to a cerclage if placed.
An additive effect has not been demonstrated in the literature.
Cerclage may be considered for a variety of indications:
Patient with both a cervix <25 mm before 24 weeks of gestation and a history of PTD <37 weeks
Meta-analyses of randomized controlled trials have demonstrated that cerclage may be beneficial in this population.
Patients with a cervix <25 mm and no history of PTD are optimally treated with vaginal progesterone without cerclage placement.
Cervical incompetence based on patient history
Generally placed around 12 to 14 weeks of gestation
There is limited evidence demonstrating the benefit of cerclage in this population.
“Rescue” cerclage placed with advanced cervical dilation in the second trimester to prevent further dilation
There is little evidence demonstrating the benefit of this intervention.
Cerclage has many limitations:
Cerclage is contraindicated in cases of infection, ruptured membranes, or active labor.
There is no evidence to support its use in multiple gestations for any indication and the suggestion that risk may outweigh benefits.
The wide variety of indications and patients selected for cerclage have led to limited evidence-based recommendations.
Cerclage, even when evidence based, may only be beneficial in one third of cases.
Abdominal cerclage may be considered in future pregnancies where vaginal cerclages have previously failed.
Screening
History of prior spontaneous PTD is the largest risk factor.
Cervical length (CL):
Patients with a CL <25 mm have a high risk of PTL/PTD and are eligible for either progesterone therapy (with CL<20 mm) or with cerclage therapy (if they have a history of a prior PTD). Screening is specifically indicated in patients with known or suspected risk for PTL/PTD (including personal history).
Fetal fibronectin (FFN)—optional adjunct to clinical management:
Should only be used as an adjunct to clinical management and is not indicated for routine screening
Collect from 24 to 34 weeks’ gestation with signs and symptoms of PTL.
Should be the first test performed during exam. The sample is taken from the posterior fornix
Invalid with vaginal bleeding, ruptured membranes, or a history of intercourse or vaginal exam within 24 hours
FFN has a negative predictive value of 99% for delivery within 7 days.
The positive predictive value for delivery within 7 days is as low as 14%; a positive result provides little clinical insight.
Evaluation
Establish best dating for gestational age using last menstrual period, fundal height, ultrasound data, and prenatal records if available.
Obtain vital signs
A temperature >38°C or fetal or maternal tachycardia may indicate an underlying infection.
Hypotension with fetal or maternal tachycardia may suggest placental abruption.
Physical exam
Fundal tenderness on exam may suggest chorioamnionitis or placental abruption.
Costovertebral angle tenderness may suggest pyelonephritis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree