Polyostotic Lesions
B. J. Manaster, MD, PhD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Fibroxanthoma (Nonossifying Fibroma)
Fibrous Dysplasia, Polyostotic
Langerhans Cell Histiocytosis (LCH)
Osteomyelitis
Osteochondroma, Multiple Hereditary Exostosis
Leukemia
Ewing Sarcoma, Metastatic
Metastases, Bone Marrow
Less Common
Lymphoma, Multifocal
Osteosarcoma, Metastatic
Hyperparathyroidism/Renal Osteodystrophy, Brown Tumor
Melorheostosis
Rare but Important
Ollier Disease
Maffucci Syndrome
Chronic Recurrent Multifocal Osteomyelitis
Sarcoidosis
Trevor Fairbank
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Polyostotic nature of lesion can narrow differential substantially and is highly valuable characteristic
Information regarding multiple sites can be gained by bone scan, PET/CT, or clinical exam
Lesions listed above range from benign (“leave me alone”) lesions → “Aunt Minnie” lesions → highly aggressive lesions
Most use this alternative approach to sort these out
Helpful Clues for Common Diagnoses
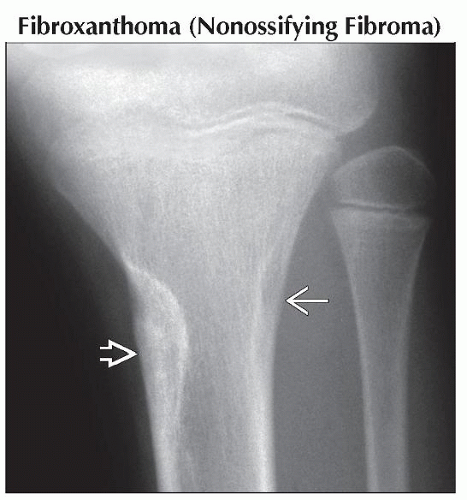
Fibroxanthoma (Nonossifying Fibroma)
Benign fibrous cortical defects (same histologically as NOF but smaller) are often multiple in children
Nonossifying fibroma (NOF) not commonly multiple, except in patients with neurofibromatosis
Both have same natural history of healing
Both are cortically based and metadiaphyseal
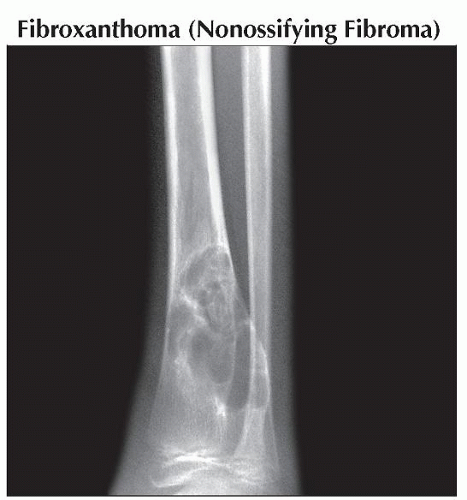
Fibrous Dysplasia, Polyostotic
Lesion may have different appearance in different locations
Skull: Sclerotic
Pelvis: Bubbly, lytic
Long bones: Generally central, metadiaphyseal, mildly expanded, with variable homogeneous ground-glass density
Langerhans Cell Histiocytosis (LCH)
Lesions may be lytic, geographic, and nonaggressive
Lesions may also be extremely aggressive in appearance: Permeative, cortical breakthrough, soft tissue mass, periosteal reaction, with rapid growth
Hint: Skull lesions may have beveled edge appearance due to differential involvement of inner and outer tables
Osteomyelitis
Hematogenous spread usually results in metaphyseal sites
Osteomyelitis can appear extremely aggressive, with permeative change and cortical breakthrough with soft tissue mass; may not be distinguishable from aggressive tumor
Sickle cell patients at risk for multifocal osseous infection; higher predilection for Salmonella
Osteochondroma, Multiple Hereditary Exostosis
Not difficult diagnosis if exophytic (cauliflower) lesions are present
May have only sessile exostoses at metaphyses, which can give appearance of dysplasia; diagnosis often missed
Leukemia
Diffuse marrow infiltration may result in appearance of osteopenia, easily overlooked
Metaphyseal lucent bands may highlight degree of osteopenia
MR shows extent of abnormalities
Ewing Sarcoma, Metastatic
Primary lesion usually highly aggressive; lytic, permeative, cortical breakthrough, large soft tissue mass
May have extensive reactive bone formation, giving appearance of osteoid, with potential confusion with osteosarcoma
Reactive bone formation restricted to bone, does not extend into soft tissue mass (as it does in osteosarcoma)
Most common sarcoma to have osseous metastases; lung and osseous metastases present with equal frequency
Helpful Clues for Less Common Diagnoses
Lymphoma, Multifocal
50% of childhood bone lymphoma is polyostotic (much less frequent in adults)
Lesions highly aggressive: Permeative, cortical breakthrough with soft tissue mass
Generally lytic but may have reactive sclerosis within osseous lesion
In same differential as Ewing sarcoma with metastases, multifocal osteomyelitis, LCH, and metastases
Alternative Differential Approaches
“Aunt Minnie” lesions can generally be identified immediately
Fibroxanthoma (nonossifying fibroma)/benign fibrous cortical defect
Osteochondroma (multiple hereditary exostoses); remember they can be sessile and resemble a metaphyseal dysplasia
Melorheostosis
Sarcoidosis (when lacy appearance is obvious)
Trevor Fairbank
Polyostotic lesions, which are usually monomelic
Fibrous dysplasia (generally unilateral)
Melorheostosis
Ollier disease
Trevor Fairbank
Maffucci syndrome
Polyostotic lesions with an intermediately aggressive appearance
Fibrous dysplasia: Generally central, poorly marginated, but geographic
Langerhans cell histiocytosis: Appearance ranges from nonaggressive geographic to extremely aggressive permeative
Hyperparathyroidism/renal osteodystrophy, brown tumor: Generally lesion is geographic, but surrounding bone abnormal in density & trabecular pattern
Polyostotic lesions with aggressive appearance: These can be indistinguishable from one another by imaging
Langerhans cell histiocytosis: Range in appearance from nonaggressive to highly aggressive
Osteomyelitis
Leukemia
Ewing sarcoma, metastatic
Metastases, bone marrow
Lymphoma, multifocal
Osteosarcoma, metastatic
Chronic recurrent multifocal osteomyelitis
Image Gallery
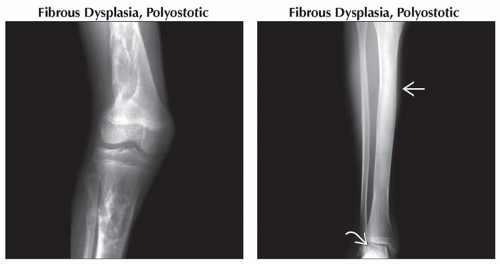 (Left) Anteroposterior radiograph shows mixed lytic and sclerotic lesion involving the metadiaphysis of the femur, tibia, and fibula. The lesions are central and nonaggressive, typical of fibrous dysplasia. (Right) Anteroposterior radiograph shows the mildly expanded and sclerotic, otherwise featureless “ground-glass” appearance of fibrous dysplasia in the tibial diaphysis
 , with a lytic talar lesion , with a lytic talar lesion  in this teenager with polyostotic fibrous dysplasia. in this teenager with polyostotic fibrous dysplasia.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|