Chapter 241 Polioviruses
Epidemiology
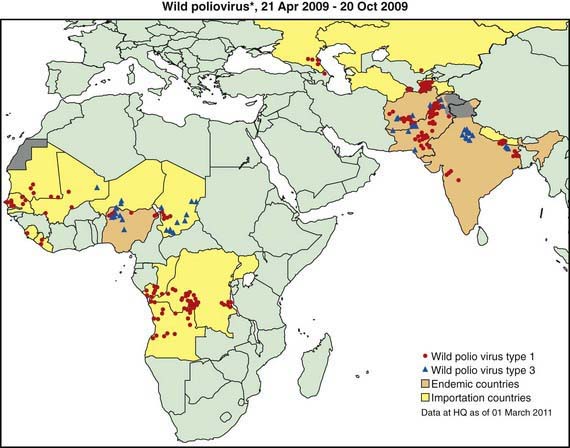
The most devastating result of poliovirus infection is paralysis, although 90-95% of infections are inapparent but induce protective immunity. Clinically apparent but nonparalytic illness occurs in about 5% of all infections, with paralytic polio occurring in about 1/1,000 infections among infants to about 1/100 infections among adolescents. In developed countries prior to universal vaccination, epidemics of paralytic poliomyelitis occurred primarily in adolescents. Conversely, in developing countries with poor sanitation, infection early in life results in infantile paralysis. Improved sanitation explains the virtual eradication of polio from the USA in the early 1960s, when only about 65% of the population was immunized with the Salk vaccine, which contributed to the disappearance of circulating wild-type poliovirus in the USA and Europe. Poor sanitation and crowding have permitted the continued transmission of poliovirus in certain poor countries in Africa and Asia, despite massive global efforts to eradicate polio, which in some areas involve an average of 12-13 doses of polio vaccine administered to children in the 1st 5 yr of life (Fig. 241-1).