Point-of-Care Sonography in the First Trimester
During the first trimester of pregnancy, clinical situations may warrant a limited or point-of-care (POC) ultrasound examination when a specific piece of information is needed to provide optimum bedside care in a timely fashion. Some of the more common clinical presentations leading to a POC ultrasound examination include vaginal spotting or bleeding, lower abdominal cramping or pain, or the inability of the clinician to auscultate fetal heart rate (FHR). However, a POC ultrasound is not intended to replace a standard first-trimester ultrasound. If a standard ultrasound study has not been performed prior to the POC imaging, it is recommended that, whenever reasonably possible, the POC scan be followed with a complete standard study.1 But if critical information is needed when a standard ultrasound is not available, a POC ultrasound is a valuable tool for providing timely diagnostic assistance.
The intention of this chapter is to describe each of the components of the standard first-trimester ultrasound examination from which components may be used for the POC sonogram. For comparison purposes, some abnormal findings are presented to assist with distinctions from normal findings.
INDICATIONS FOR FIRST TRIMESTER STANDARD SONOGRAM
In 1984, The National Institutes of Health convened a task force to determine if routine sonography was appropriate for all pregnancies. Their conclusion was that not all pregnant women would benefit from a routine ultrasound, and therefore a list of appropriate indications was generated for sonography for all trimesters of pregnancy.2 That basic premise still exists today; however, the indications for a first-trimester ultrasound examination have been updated in recent years1,3 and are shown in Box 11-1. It should be noted that many of the individual indications identified are also indications for a POC ultrasound examination under certain clinical situations.
DISCRIMINATORY ZONE IN FIRST TRIMESTER EVALUATION
Serum screening for quantitative beta human chorionic gonadotropin (β-hCG) has been the “gold standard” for many years in assessing the stable patient for an abnormal pregnancy. Although it is not diagnostic, it still may be used in conjunction with sonographic evaluation. However, the best approach for patient management will depend on both the availability of the testing procedure, the skills of the clinician performing the sonogram, and the interpretation of the results of each.
In the past, certain ranges or cutoffs of β-hCG levels (known as the “discriminatory zone”) were used in conjunction with specific first-trimester ultrasound findings to differentiate between viable and nonviable pregnancies. Research has shown many drawbacks to that system, and its use is no longer recommended. Doublet and Benson4 determined that there are potential errors in image interpretation that can lead to errors in management when utilizing this approach: (1) the failure to conclude there is a definite or probable viable pregnancy in conflict with ultrasound images showing such a finding, and
(2) the failure to conclude that there is sonographic confirmation or likelihood of the presence of an ectopic pregnancy despite ultrasound images supporting that finding.
(2) the failure to conclude that there is sonographic confirmation or likelihood of the presence of an ectopic pregnancy despite ultrasound images supporting that finding.
BOX 11-1 Indications for First-Trimester UItrasound Examination
Confirm the presence of an intrauterine pregnancy
Evaluate a suspected ectopic pregnancy
Define the cause of vaginal bleeding
Evaluate pelvic pain
Estimate gestation age
Diagnose or evaluate multiple gestations
Confirm cardiac activity
Localize and remove an intrauterine device
Assess for certain fetal anomalies
Evaluate maternal pelvic masses or uterine abnormalities
As an adjunct to chorionic villus sampling, embryo transfer
Measure nuchal translucency as part of aneuploidy screening
Evaluate a suspected hydatidiform mole
The first potential error may come from failing to see a “double sac sign (DSS)” or the “intradecidual sign (IDS),” interpreting the findings as a nonviable pregnancy, and moving forward with medical or surgical intervention. The double sac sign is thought to represent the two layers of decidua surrounding the intrauterine fluid collection and does occur in most, but not all, normal pregnancies. There is no data to support that the absence of this finding is consistent with an abnormal pregnancy.
The second problem is the misdiagnosis of a pseudogestational sac, which refers to fluid in the uterine cavity that is occasionally seen in women with an ectopic pregnancy. Fluid in the endometrium is more likely to be a gestational sac than a pseudogestational sac. When nonspecific intrauterine fluid collection is seen, the odds of a gestational sac over a pseudogestational sac are approximately 245:1.
If no intrauterine sac is seen and the patient’s quantitative β-hCG is well above a discriminatory level where one expects to see an intrauterine pregnancy (IUP), there should be concern for an ectopic pregnancy. If a sonogram shows a definite extrauterine pregnancy (embryo with cardiac activity), then the presence or absence of a pseudogestational sac is clinically irrelevant.3
Doublet and Benson5 also investigated the interobserver agreement, frequency of occurrence, and the prognostic importance of the DSS, the IDS, and other sonographic findings in early pregnancies. As for the occurrence of these signs, the interobserver agreement was poor because the sonographic images frequently did not demonstrate either sign. The presence of a DSS or IDS was also unrelated to β-hCG levels, first-trimester outcome, presence of an inner echogenic ring, or decidual presence. The conclusion was that the sonographic appearance of an early gestational sac, before visualization of a yolk sac or embryo, is highly variable. Therefore, it is advised that if a round or oval intrauterine fluid collection is sonographically visualized in a woman with a positive β-hCG, it should be treated as a gestational sac until proven otherwise, regardless of whether it demonstrates a DSS or an IDS. Performing medical and surgical interventions has the potential to damage an IUP, and these procedures should be avoided unless a viable pregnancy is definitely excluded by follow-up β-hCG values or sonograms.5
TRANSVAGINAL SONOGRAPHY IN THE FIRST TRIMESTER
One of the most important prognostic indicators in the first trimester is the crown-rump length (CRL) of the fetus. It is the most accurate biometric measurement for the prediction of gestational age, as well as having predictive value in determining survivability of a pregnancy.6 The development of the vaginal sonography, along with improved resolution, has led to improved accuracy. Transvaginal sonography (TVS) uses higher frequency transducers, which provides a 40% to 50% improvement in lateral and axial resolution over transabdominal sonography (TAS). Although the American Institute of Ultrasound in Medicine (AIUM)1 states that first-trimester ultrasound may be performed by the TA approach only, most sonographers employ both TV and TA transducers during the standard first-trimester scan. Initially, patient acceptance in the use of the vaginal probe was a concern, but when women presented with early pregnancy issues, the TV probe was acceptable.7
THE STANDARD SONOGRAPHIC EXAM IN THE FIRST TRIMESTER OF PREGNANCY
Membranes, Yolk Sac, and Umbilical Cord
With a normally developing pregnancy, certain parameters are expected to be visible by TVS at specific gestational ages. The identifiable gestational sac is typically present at 5 weeks’ gestation. The yolk sac, located within the chorioamniotic space, becomes visible at 5.5 weeks. A small fetal pole containing an active fetal heart can be seen by 6 to 6.5 weeks, with the beat occurring around the same time. The thin and wispy amniotic membrane is sonographically visualized at 7 weeks. The chorioamniotic space obliterates as the amniotic cavity grows to the size of the chorion. By 14 to 16 weeks’ gestation, the amnion fuses with the chorion, making the two sonographically indistinguishable. Further details are described below.
gestational Sac
Endometrial implantation of the blastocyst occurs approximately 9.5 days after conception. Prior to
the identification of a normal gestational sac, the endometrium appears secretory. Sonographically, a double-echogenic ring or decidual reaction is produced by the decidual capsularis and the decidua parietalis.
the identification of a normal gestational sac, the endometrium appears secretory. Sonographically, a double-echogenic ring or decidual reaction is produced by the decidual capsularis and the decidua parietalis.
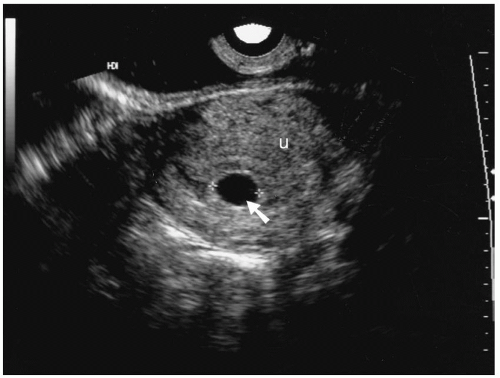 FIGURE 11-1. Transvaginal sonographic image of a normal 6.5-week gestational sac (arrow) showing the sac within the uterus (U). |
The normal gestational sac can be seen as early as 4 to 5 weeks of gestation or when the sac is 2 to 5 mm in size.6,8 The gestational sac size has been used to predict gestational age before the identification of the embryo. The normal gestational sac typically appears ellipsoid or circular in shape. Sonographically, the sac appears as a hypoechoic or anechoic area in or near the midline of the uterus (Figure 11-1). The gestational sac size is obtained by measuring the gestational sac in all three dimensions at the chorionic margin (Figure 11-2). One of these planes should be made at the largest diameter of the sac. These measurements are then averaged together.
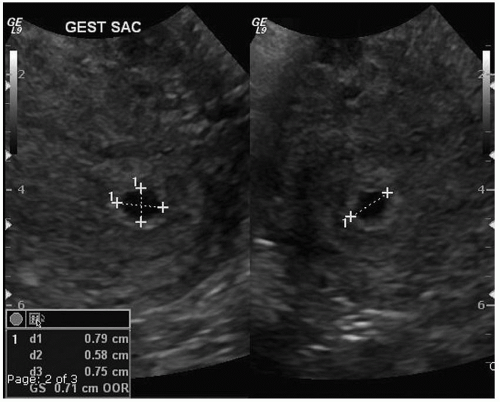 FIGURE 11-2. Gestational sac measurement in two coronal views. The sac is the anechoic area within the uterine cavity, which is hyperechoic. |
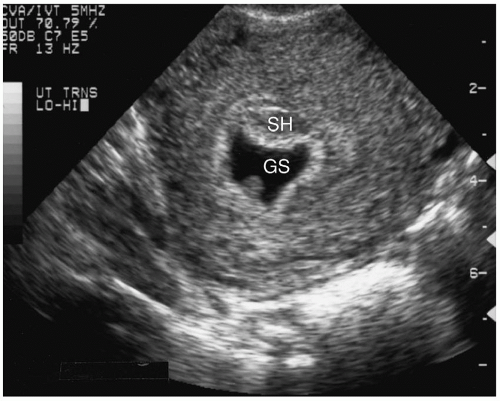 FIGURE 11-3. An irregular gestational sac, as seen in this transvaginal image, has been associated with an abnormal pregnancy. GS, gestational sac; SH, subchorionic hemorrhage. |
A mean sac diameter of 25 mm or greater with no visible embryo is diagnostic of a failed pregnancy. An abnormal shape to the gestational sac may suggest an abnormal pregnancy (Figure 11-3).9 Additionally, the gestational sac should increase in size by 1 to 1.2 mm/day. Any abnormal growth of the gestational sac is a poor prognostic sign.10
The yolk sac is the next structure that becomes visible, typically between 5 and 6 weeks of gestation. It is located outside the amnion and appears as an echogenic ring with an anechoic center (Figures 11-4 and 11-5). Recent studies suggest that an irregular yolk sac shape is unrelated to an increased risk of spontaneous abortion.11
The yolk sac, fetal pole, and fetal heart can be seen earlier by TV ultrasound than by the TA approach (Table 11-1). Therefore, if the scan has been performed transabdominally without evidence of any of the identifiable fetal anatomy or landmarks, a TV approach should be used.
The Embryo/Fetus
An embryo can first be identified with a TV transducer at approximately 5 to 6 weeks’ gestation. Cardiac motion should be observed when the embryo is 2 mm
or greater in length. If cardiac activity is not observed when the embryo is greater than 7 mm in length, a subsequent scan 1 week later is recommended to confirm a viable versus a nonviable pregnancy. This should be performed prior to any medical or surgical interventions.1,3 The fetal number should be confidently identified beginning at approximately 8 weeks’ gestation.
or greater in length. If cardiac activity is not observed when the embryo is greater than 7 mm in length, a subsequent scan 1 week later is recommended to confirm a viable versus a nonviable pregnancy. This should be performed prior to any medical or surgical interventions.1,3 The fetal number should be confidently identified beginning at approximately 8 weeks’ gestation.
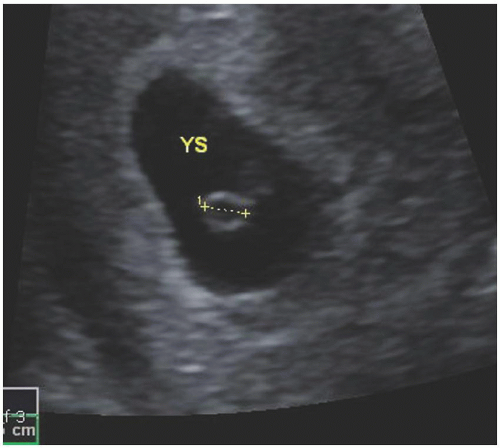 FIGURE 11-4. Gestational sac with presence of yolk sac,measured (YS).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|