Point-of-Care Sonography in Gynecology and Reproductive Medicine
The three most common indications for point-of-care (POC) sonography in gynecology include the evaluation of the endometrial thickness, the measurement of follicles during ovarian stimulation with assisted reproductive technologies, and the localization of intrauterine devices (IUDs) pre- and postinsertion. In addition, POC sonography is utilized to measure retained residual urine following birth and in urogynecologic bladder assessments, among other indications.
However, prior to performing any gynecologic sonogram, it is essential to know the anatomy of the female pelvis. It is recommended to have a standard pelvic sonogram performed prior to performing any POC ultrasound. Following the performance of a complete pelvic sonogram, a “limited” or POC gynecologic ultrasound examination can be restricted to a specific organ or measurement.1 The purpose of this chapter is to describe the anatomic structures and the measurement of these structures sonographically, as well as the documentation and communication of findings.
In the gynecologic or reproductive medicine specialty, a limited or POC sonogram may involve any one or all of the processes listed in Table 10-1. Although POC sonograms following a successful assisted reproductive procedure may include sonographic confirmation of pregnancy, sonography in the first trimester of pregnancy is discussed in Chapter 11.
TABLE 10-1 LIMITED PELVIC ULTRASOUND EXAMINATION | ||
|---|---|---|
|
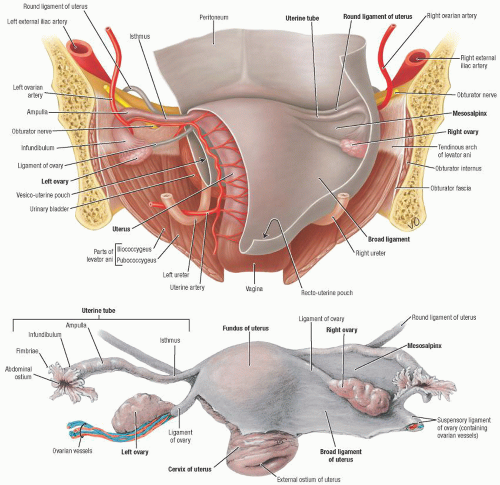
ULTRASOUND ANATOMY OF THE FEMALE PELVIS
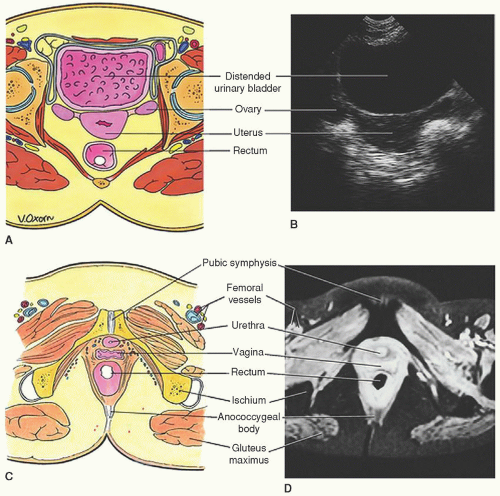
The female pelvis can be imaged using the transabdominal (TA) or transvaginal (TV) approach. TA sonography (TAS) requires a full urinary bladder to displace air-filled bowel from the lower abdomen and to provide an acoustic window through which to visualize the pelvic organs (Figure 10-1). An acoustic window is a structure that has no acoustic impedance (no returning ultrasound signals) and is referred to as anechoic. This absence of returning sound waves imparts a black image on the monitor. This lack of impedance allows for passage of sound and enhanced visualization of deeper structures. In the TA approach, the depth of penetration into the body is much deeper, so more structures can be accessed, but it has inherently less resolution than the TV approach.
TVS requires an empty urinary bladder and is performed with high-frequency transducers. High frequency is better for resolution and visualization of the structures, but the depth of penetration of a high-resolution transducer, such as the vaginal probe, is shallower. For TV ultrasound, this penetration depth is accomplished by literally getting physically closer to the structures by way of the tip of the vaginal wand being in close proximity to the structure being imaged. In many circumstances, it is helpful to use both TAS and TVS to visualize the entire pelvis.
URINARY BLADDER
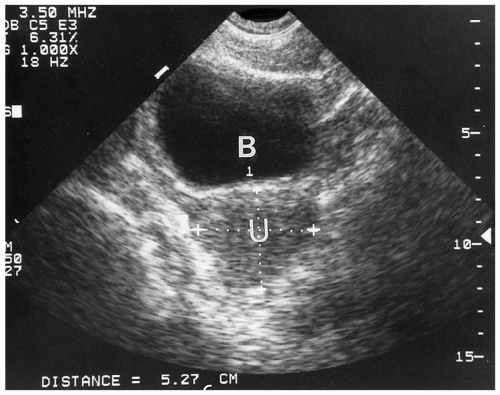
The urinary bladder is an important landmark in identifying pelvic anatomy. The bladder walls are
composed of a thick (detrusor) muscle that is lined with a thin mucosa and covered externally by a serosal layer. Bladder distention causes a thinning and stretching of the bladder wall, which then appears as a thin echogenic line. With partial distention, the detrusor muscle is relaxed and appears as a hypoechoic layer around the inner mucosa (Figure 10-2). Ureters can be recognized when they are abnormally filled with fluid. They can be distinguished from the adjacent iliac vessels by their more echogenic walls, anatomical path, and by color Doppler. A urine jet can be seen in grayscale or color Doppler as the ureters enter into the posterior portion of the bladder.
composed of a thick (detrusor) muscle that is lined with a thin mucosa and covered externally by a serosal layer. Bladder distention causes a thinning and stretching of the bladder wall, which then appears as a thin echogenic line. With partial distention, the detrusor muscle is relaxed and appears as a hypoechoic layer around the inner mucosa (Figure 10-2). Ureters can be recognized when they are abnormally filled with fluid. They can be distinguished from the adjacent iliac vessels by their more echogenic walls, anatomical path, and by color Doppler. A urine jet can be seen in grayscale or color Doppler as the ureters enter into the posterior portion of the bladder.
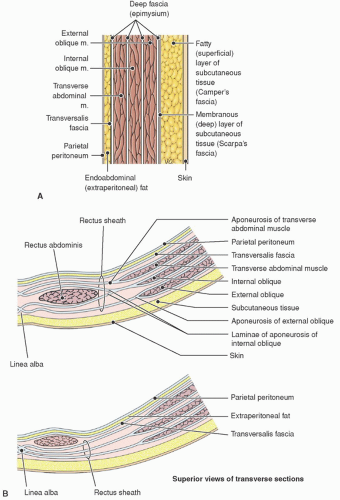
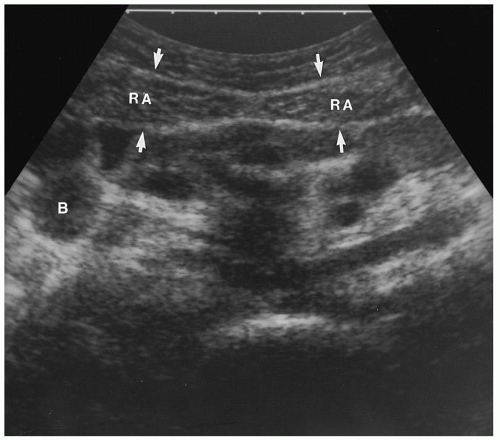
PELVIC MUSCULATURE
On ultrasound, muscles appear as hypoechoic bands of tissue, with low-level echoes and thin linear hyperechoic striations. The skeletal muscles of the false pelvis include the rectus and transverse abdominis and the iliopsoas muscles (Figures 10-3 and 10-4).
The muscles of the true pelvis include the obturator internus muscles, the piriformis muscles, and
the muscles of the pelvic diaphragm. The latter are composed of three paired muscles: the coccygeus, the pubococcygeus, and the iliococcygeus, which form the floor of the true pelvis and support the pelvic organs (Figures 10-5 and 10-6).
the muscles of the pelvic diaphragm. The latter are composed of three paired muscles: the coccygeus, the pubococcygeus, and the iliococcygeus, which form the floor of the true pelvis and support the pelvic organs (Figures 10-5 and 10-6).
The pubococcygeus and iliococcygeus muscles together form the levator ani muscles (Figure 10-7). The iliopsoas muscles can be identified in the sagittal (longitudinal) imaging as linear structures along the pelvic sidewall that are medial and slightly anterior to the iliacus muscles and as ovoid structures that are anterior and lateral to the urinary bladder on transverse imaging (Figure 10-8).
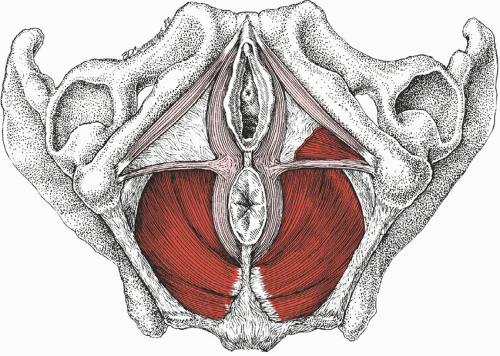 FIGURE 10-5. Pelvic floor muscles as seen from below in the supine female subject. The muscles of the pelvic diaphragm are dark red, and the associated pelvic muscles are light red. |
The obturator internus muscles run parallel to the lateral walls of the bladder on transverse scans, but are more difficult to identify in the sagittal plane. The muscles of the pelvic diaphragm are seen best in the transverse plane at the level of the cervix.
Many pelvic muscles are difficult to evaluate sonographically. It is not unusual for normal muscles to be mistaken for free fluid, a mass, or other pathology; therefore, it is important to recognize the appearance of muscles, where they attach, and how each muscle is oriented.
PELVIC VASCULATURE
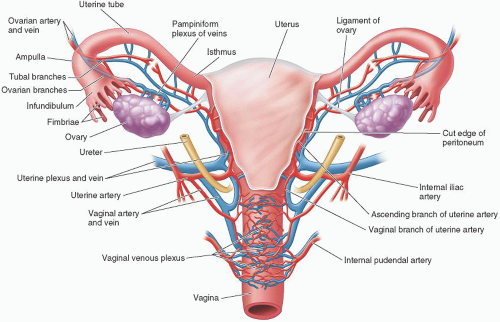
The common iliac arteries branch into the internal and external arteries. The internal and external iliac veins join to form the common iliac vein. The internal iliac vessels lie posterior and slightly lateral to the ovaries and are important landmarks to help identify and locate the ovaries (Figure 10-9), especially when the ovaries are small and lacking follicles.
The internal iliac arteries have a width of 5 to 7 mm and are pulsatile, whereas the veins are typically larger (1 cm), more medially located, and do not pulsate. The blood supply to the uterus and vagina
is via the uterine artery, which is a branch of the internal iliac artery (Figure 10-10).
is via the uterine artery, which is a branch of the internal iliac artery (Figure 10-10).
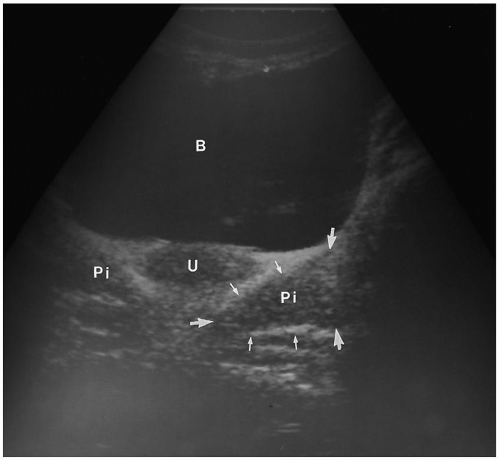 FIGURE 10-6. Transverse transabdominal image through a full bladder (B) showing the uterus (U) and the piriformis muscles (Pi) within the arrows, posterior to the cervix. |
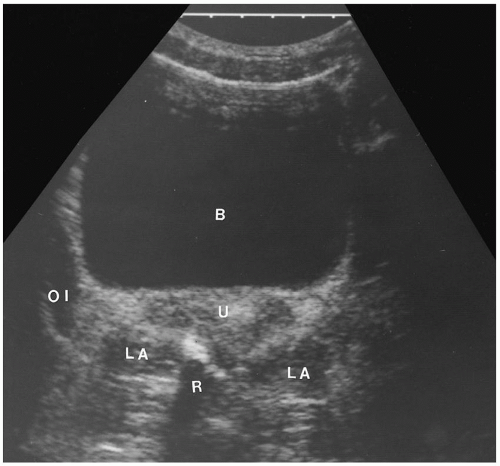 FIGURE 10-7. Transverse transabdominal image of levator ani (LA) muscles, the right obturator internus muscle (OI), bladder (B), and rectum (R), posterior to cervix. |
The uterine arteries give rise to the arcuate arteries, which encircle the uterus and branch into the radial arteries. The radial arteries pass through the myometrium, become the straight arteries at the level of the endometrium, and then branch to form spiral arteries. The blood supply to the endometrium
is from the straight and spiral arteries, the latter being responsive to hormonal changes of the menstrual cycle. The ovarian blood supply is from both the ovarian and uterine artery and vein. The ovarian artery enters the ovarian hilum via the mesovarium, whereas the uterine artery reaches the ovarian hilum via the broad ligament.
is from the straight and spiral arteries, the latter being responsive to hormonal changes of the menstrual cycle. The ovarian blood supply is from both the ovarian and uterine artery and vein. The ovarian artery enters the ovarian hilum via the mesovarium, whereas the uterine artery reaches the ovarian hilum via the broad ligament.
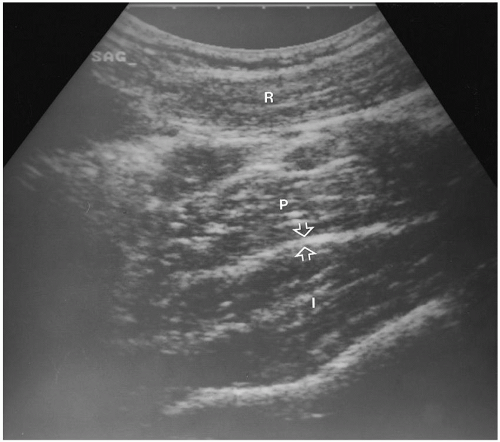 FIGURE 10-8. Sagittal transabdominal image with transducer angled laterally to demonstrate the long axis of the psoas major (P), and the iliacus muscles (I), with interposed fascial plan (arrows). |
UTERUS
The uterus is the most prominent landmark in the pelvis and can be visualized by both TA and TV ultrasound (Figures 10-11 and 10-12). In the nonpregnant uterus, the cervix represents approximately one-third to one-half of the total uterine length and is approximately twice the diameter of the corpus. The adult uterus is approximately 6 to 8 cm in length and 3 to 5 cm wide.
The typical uterine position is anteverted, although a full bladder will displace an anteverted uterus into a more horizontal position (Figure 10-13). Variations include retroverted uterus, which is the posterior angulation of the uterus and cervix relative to the vagina; retroflexed uterus, which describes the posterior angulation
of the uterine corpus relative to the cervix; and anteflexed, which is the anterior angulation of the uterine corpus relative to the cervix (Figures 10-14 and 10-15).
of the uterine corpus relative to the cervix; and anteflexed, which is the anterior angulation of the uterine corpus relative to the cervix (Figures 10-14 and 10-15).
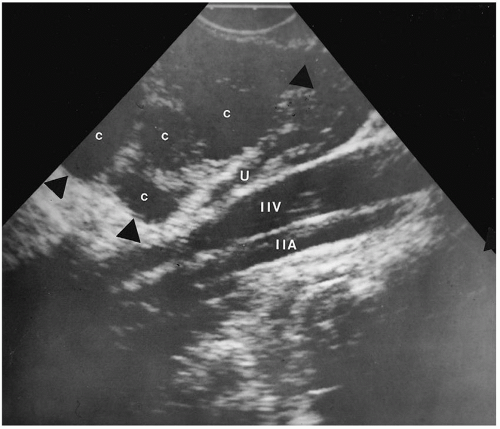 FIGURE 10-10. Sagittal transvaginal scan of left internal iliac artery (IIA) and vein (IIV) posterior to the ovary (arrowheads). |
Myometrium
The myometrium, which exhibits medium to low-level homogeneous echoes, can be distinguished from the endometrium, which varies in thickness and echogenicity throughout the menstrual cycle. Uterine blood vessels can be imaged using both TA and TV sonography. When seen, arcuate arteries appear as anechoic tubular structures at the periphery of the myometrium. Calcifications may be seen within the arcuate arteries of elderly patients and appear as echogenic foci along the periphery of the uterus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree