HISTORY OF THE BIOPHYSICAL PROFILE
The BPP was developed in 1980 by Manning and Associates
1 and utilizes traditional electronic fetal monitoring (EFM) in combination with a sonographic fetal evaluation. Manning viewed this technique as “undertaking an intrauterine physical examination, analogous to Apgar scoring.”
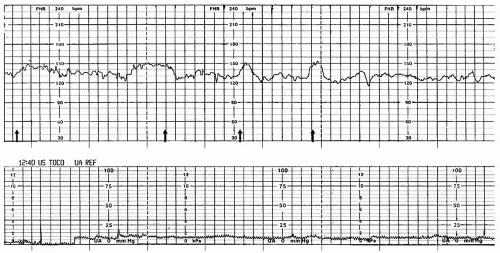
As the fetal central nervous system (CNS) matures with advancing gestational age, fetal behavior develops in a specific order. Fetal tone (FT) begins to be evident by ultrasound around 7.5 to 8 weeks of gestation, followed by fetal movement (FM) beginning around 9 weeks’ gestation. Fetal breathing becomes regular at 20 to 21 weeks, followed by development of fetal heart rate (FHR) control (the ability to accelerate and decelerate) at the end of the second or beginning of the third trimester.
With an insidious or chronic loss of fetal oxygenation, the fetus begins to lose these same behaviors, but in the
opposite order in which they developed. So, in the event of chronic oxygen deprivation, initially there will be the loss of fetal heart reactivity followed by a decrease or loss of fetal breathing movements (FBM). If the oxygen deprivation continues, a decrease in amniotic fluid will occur. Ultimately, there will be a loss of FM with, finally, the loss of FT.
1 Although factors other than deoxygenation may cause a change in some or all of these behaviors, these are the parameters that, when present, were determined to be predictive of fetal oxygenation, and thus they are used as the basis of the BPP.
FHR reactivity, tone, movement, and breathing are CNS activities that respond to acute hypoxic changes. Additionally, decreased amniotic fluid volume (AFV), in the absence of ruptured membranes or fetal renal abnormalities, may be an indicator of chronic fetal compromise as oxygenated blood is shunted from the fetal kidneys to the vital organs. Knowledge of the five parameters, their progressive emergence throughout gestational age, and pattern of decline with increasing hypoxia can provide invaluable information regarding the oxygenation status of the fetus.
The five parameters assessed in the Manning BPP are:
The BPP has a very low false-negative rate, meaning that a score of 8/10 or 10/10 is highly predictive of adequate fetal oxygenation and the absence of fetal metabolic acidemia. However, each single BPP parameter has a high false-positive rate, meaning, for example, that absence of fetal breathing alone may be the result of sleep cycles, medication affects, or some unknown cause other than deoxygenation. The false-positive rate can be greatly reduced when the parameters are combined. The specific criterion for each parameter was defined by Manning with a scoring system of 2 points if the parameter is present and 0 if it is absent (
Table 13-1).
1,
2 There is no partial score.
In 1983, Vintzileos et al.
3 proposed a modification to Manning’s scoring system. In addition to Manning’s five parameters, Vintzileos introduced a sixth parameter: placental grading based on the degree of maturation of the placenta. A mature placenta is given the highest score, and the immature
placenta a low score. Additionally, the change to the scoring system for each parameter included adding a middle point value option, a score of 1, that accounted for the observation of partial fetal behaviors, borderline amniotic fluid levels, and/or the inability to grade the placenta (
Table 13-2).
3Both forms of BPPs have similar neonatal outcome predictive value. Whichever BPP point system is chosen to be used in a particular health care setting should be clarified and established in a protocol. Potentially, clinical management could be adversely impacted if only a raw score is reported. For instance, a loss of 2 points for oligohydramnios and 2 points for absence of FM would give a score of 8 (out of 12) on the Vintzileos scale and a 6 (out of 10) on Manning’s. In this example, the raw score of eight on the Vintzileos scale would be falsely reassuring if it is believed to be based on the Manning criteria. It is imperative to express the score with both the numerator and denominator (8/12 or 8/10) so that the test may be interpreted correctly. For the purposes of this chapter, the BPP parameters
and scoring system presented will be based on the Manning 10-point criteria.